1. Introduction
Cervical cord injury is a high-level spinal cord injury in which the patient develops tetraplegia, sensory and bowel dysfunction below the level of injury, manifested as neurogenic bladder and neurogenic rectum. Autonomic dysreflexia (AD), or autonomic hyperreflexia, is a common group of clinical syndromes characterized by autonomic dysfunction after spinal cord injury in the T6 or higher level (1). The incidence of AD after spinal cord injury is as high as 90% (2). Common risk factors for AD include urinary factors, gastrointestinal irritants, stress injuries, fractures below the level of injury, and painful irritation (3). It can lead to hypertensive crises, paroxysms, intracranial hemorrhages, and even death if left untreated (4). Early identification and elimination of possible triggers is the key to preventing AD onset (5).
This paper reports on a tetraplegic patient with a cervical medullary injury who developed AD during intermittent catheterization. We investigated the occurrence of and factors influencing AD during intermittent catheterization and explored the etiology of AD and nursing interventions through a literature review based on urodynamics combined with a bladder scanner. After precise catheterization timing and other interventions, the number of AD episodes was significantly reduced, leakage was decreased, and urine volume was controlled in the normal range with good results.
2. Case Presentation
A male patient, aged 24, was admitted to a hospital emergency ward with a diagnosis of cervical fracture with spinal stenosis. On February 19, 2019, he underwent a surgical procedure under general anesthesia. The procedure involved the anterior subtotal resection of the cervical 6 vertebral body, as well as the resection of the cervical 5/6 and cervical 6/7 interbody. Additionally, it included spinal canal reduction, interbody fusion, and internal fixation. Additionally, iliac bone extraction was performed, and he was treated with analgesia, anti-infection, sputum removal, and symptomatic support after surgery. This time, he was treated for motor and sensory dysfunction of the extremities with diaphoresis.
On September 10, 2021, he was admitted to our department for rehabilitation treatment. His diagnosis on admission included spinal cord injury (C4 AISA level), neurogenic bladder, and postoperative multiple fractures of cervical 4 - 7. Besides, he was clear and mentally competent and used a wheelchair for mobility. Physical examination showed a body temperature of 36.7°C, a pulse rate of 82 beats per minute, a respiratory rate of 19 breaths per minute, and a blood pressure of 105/68 mmHg. The patient exhibited sensory impairment below the head and neck, as well as varying degrees of muscle atrophy in the extremities. The bilateral C4 and above levels were normal, while the C5 levels were decompensated, and those below C6 were absent. Urodynamic examination combined with asynchronous cystography showed hypoesthesia of the bladder in the storage phase, decreased compliance, hyperreflexia of the detrusor muscle, and Safety Bladder Capacity (SBC) of 294 mL at a Detrusor Leak Point Pressure (DLPP) of < 40 cmH2O. The contraction of the urinary muscles in the bladder during voiding was weak. There was no abnormality in the urological ultrasound.
2.1. Treatment and Regression
After admission, the patient was given rehabilitation training to improve his daily living activities and hand function and prevent muscle atrophy. He also received intermittent catheterization with the assistance of others for urination, 4 - 8 times a day, with a catheterization volume of about 150 - 400 mL, accompanied by leakage of about 50 - 200 mL. Defecation occurred once a day, assisted by an open plug. He was given methylcobalamin dispersible tablets to nourish the nerves, baclofen to reduce muscle tone, and solifenacin succinate + mirabellum extended-release tablets to reduce urine leakage. On September 28th, the patient complained of noticeable urine leakage and increased sediment in the catheterized urine. He also reported experiencing a sudden headache without any apparent cause, as well as flushing, sweating, and a vertical hair reflex. These symptoms were more prevalent at night. The urine routine showed leukocytes 3+. Considering the urinary tract infection, he was given amoxicillin clavulanate potassium orally and bladder flushing twice a week. One week later, the urinary routine was normal, so the indwelling catheter was removed, and the intermittent catheterization with hydrophilic coating was continued 6 - 7 times a day. On examination, the patient appeared alert, irritable, flushed, and sweaty. The patient had a vertical hair reflex, and his vital signs were as follows: A body temperature of 36.87°C, a heart rate of 98 beats per minute, and a blood pressure of 170/110 mm Hg. He was diagnosed with autonomic hyperreflexia following a spinal cord injury. As part of his treatment, he received oxygen, had his head elevated, was administered sublingual nifedipine 10 mg, and underwent urinary catheterization. The department promptly provided medical and nursing consultation, adjusted the plan based on the patient's risk assessment results, and guided the plan for drinking, urination, physical therapy, and daily behavior. This guidance was based on factors such as urodynamic results, measurements from a portable bladder scanner, and a urination diary. The goal was to determine the optimal time for catheterization and identify any triggering factors.
2.2. Risk Assessment
According to the patient's condition, he underwent a comprehensive evaluation once again. Based on the patient's complaints and the timing of the occurrence of AD, it was determined that the patient was currently having regular bowel movements with the aid of a stool softener once a day. There were no adverse effects, such as skin breakage or pain. The family members were skilled in performing catheterization with assistance. Occasionally, the urine was turbid. Autonomic dysreflexia typically occurs during periods of an overinflated bladder or a urinary tract infection. Additionally, deep sleep at night was more prevalent.
2.3. Prevention Strategies: Early Identification of Autonomic Dysreflexia
Based on the risk factors for paroxysms, the patient and caregivers were informed to promptly report any symptoms such as headache, blurred vision, flushed skin, sweating, vertical hair, nasal congestion, and elevated blood pressure to the healthcare provider for early management.
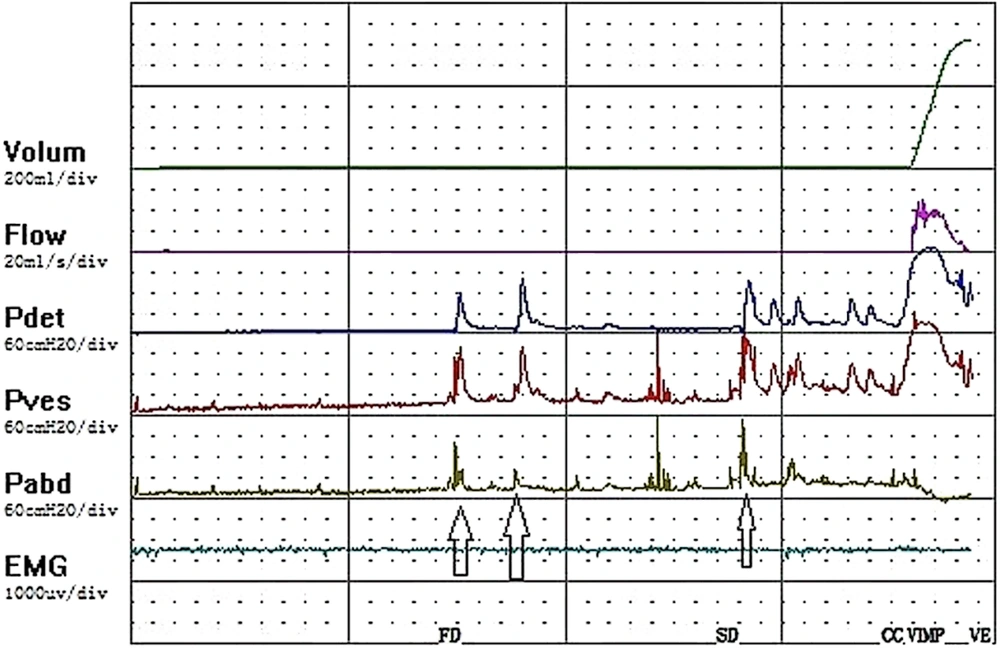
The patient complained of frequent nocturnal episodes. Therefore, the patient and caregivers should be informed to promptly report any signs and symptoms of AD. They should also cooperate with medical personnel to quickly assess possible causes, especially if the underlying cause has not been identified yet. Additionally, it is important to promptly eliminate any factors that may trigger the episodes. To provide immediate relief, the patient should be seated in an upright position with the head of the bed elevated. Furthermore, any tight clothing, stockings, or constricting devices should be loosened. Urodynamic assessment results showed that bladder safe volume was low, detrusor leakage point pressure was high, and the risk of upper urinary tract damage was high (Figure 1).
2.4. Bladder Management: Drinking Plan
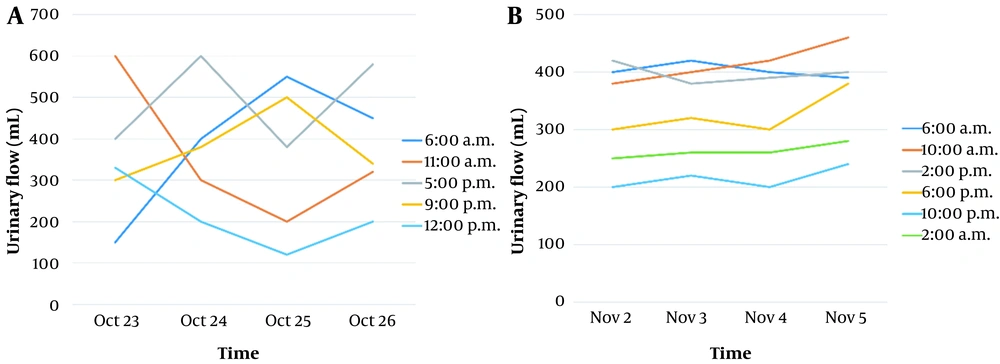
The bladder diary of this patient (Figure 2) showed that the patient did not use a teacup and measuring cup with a scale but instead relied on rough estimates. The recordings were vague and based on memory, lacking detailed information. Thus, the patient was informed about the significant correlation between the bladder diary and the occurrence of AD. They were asked to initially enhance the 72-hour comprehensive bladder record from October 8 (excluding holidays) in order to gain insight into the patient's urine production patterns and other relevant conditions. The patient's original drinking schedule was as follows: 400 mL of water at three meals (including thin rice, soup, fruit, etc.) and 200 mL of water between three meals at 10:00, 15:00, and 20:00 for a full day of 1,800 mL. Based on the bladder diary and the patient's reality, a personalized drinking schedule was adopted, based on the "Practice Guidelines for the Care of Neurogenic Bladder (2017 edition). The patient's water intake was limited to 2,000 mL per day based on the patient's water intake plan from the Neurogenic Bladder Care Practice Guidelines (2017). Based on the patient's diet, water intake, training therapy, bathing, sleep, and waking time, the patient and family members redesigned the water plan to include information on meal times, food types, and the time to drink water or fruit. They instructed the patient not to drink after 20:00 and to avoid diuretic foods such as watermelon, tea, coffee, and stimulating acidic and spicy foods. The water intake plan was adjusted; the amount of water consumed at three meals remained unchanged, and the amount of water consumed was adjusted to 150 mL at 9:00 a.m. and 10:00 a.m., 200 mL at 15:00 a.m., and 100 mL at 20:00 a.m. After 20:00 a.m., no more water was consumed as far as possible because the patient had taken solifenacin succinate + mirabellum extended-release tablets for a long time. The patient was instructed to disperse the 100 mL of drinking water at 20:00 to 50 mL each time and drink when thirsty. We instructed family members to bring the planned water intake to the physiotherapy room, set the alarm, bring graduated teacups and measuring cups, and supervise patients to finish at the specified time to ensure that the water intake plan was implemented and recorded carefully in detail. Reducing the amount of water consumed in the evening and at night would avoid excessive nocturnal urination and ensure the patient's rest. Intermittent catheterization was performed regularly. After a week of continuous follow-up, including the inspectors during the morning and afternoon physical therapy operating hours, the patient could implement the above drinking plan according to the norms.
2.5. Bladder Management: Intermittent Catheterization
Ideally, the schedule for intermittent catheterization should be volume-based, meaning it should be within the safe capacity of the patient's bladder to achieve the maximum bladder capacity possible (6, 7). The frequency of urinary catheterization in this patient was 4 - 8 times a day in the usual way. Due to the presence of frequent daytime rehabilitation training, the patient was catheterized after waking up at 6:00 a.m., before going out for physical therapy at 1:00 p.m., while taking a bath at 5:00 p.m., before going to bed at 10:00 p.m., and when he felt his abdomen was full, during which the leakage volume ranged from 50 - 200 mL, with a high volume at night, all of which were taken to collect urine from the urine bag. Given the above, based on the bladder diary and urodynamic findings of this patient, the bladder volume and urine production pattern of the patient was closely monitored using a bladder scanner (PadScan HD 5), and the timing of catheterization was corrected for the patient's self-perceived sense of bladder fullness by measuring the bladder volume one hour after excessive water intake, one hour before each fixed leakage time, and before performing intermittent catheterization. If the measured bladder capacity was less than 50% of the safe capacity, catheterization could be delayed; if the measured bladder capacity was more than 50% of the safe bladder capacity and did not exceed the safe capacity, catheterization should continue to be given as usual; if the capacity exceeded the safe capacity, catheterization should be given immediately, and the patient and the helper should carefully record the voiding log and visually inform the patient through the bladder scanner that he could not follow his sense of bladder fullness because of his reduced sense of bladder fullness during the storage period. The patient should be informed visually through the bladder scanner. Because of their diminished sense of bladder fullness during the storage period, the timing of catheterization should not be based on their sense of fullness, nor should it be based on the occurrence of symptoms such as leakage, headache, and blushing, but should be done in advance according to the safe capacity of the bladder before the occurrence of symptoms such as leakage, with the focus on ensuring urine storage and voiding at low pressure, firstly to protect renal function and secondly to reduce incontinence. After nearly a week and observing the entire process of physiotherapy, the timing of catheterization for this patient has been adjusted as follows: the morning catheterization at 6:00 remains unchanged, an additional catheterization will be done before the 10:00 physiotherapy session, the afternoon catheterization will be delayed to 14:00, rehabilitation treatment will be conducted after catheterization, the timing of catheterization before bathing and eating will be changed to 18:00 after bathing, and the patient will not consume any liquids after 19:00. After 7:00 p.m., we do not drink food containing much water, and avoid diuretic and sodium-containing food, such as watermelon, tea, spicy and sour food. We catheterize once before bedtime at 22:00 and once more at 2:00 a.m. according to the frequent occurrence of AD at night and the relatively small safe capacity of the patient's bladder, and the nurse in charge is responsible for teaching and supervising the patient.
2.6. Bladder Management: Bladder Flushing
Patients with neurogenic bladder due to spinal cord injury are routinely given bladder flushing twice a week to reduce the probability of bladder stones, urinary tract infection, hydronephrosis, and renal failure to remove residual urine volume and residue from the bladder diverticulum (8, 9). This patient routinely undergoes bladder flushing twice a week. According to the patient's occasional discomfort, such as urethral irritation when AD occurs, the patient was recently observed to have a lot of urine sediment and odor. According to the study by Adriaansen et al. (10), on-demand bladder irrigation was used, which is not necessary when the urine is normal. When there is sediment, flocculent, or odor in the urine, the irrigation frequency is once a day until the urine is clear and odorless, as observed by the naked eye. In this case, the frequency of bladder flushing was changed from 2 times a week to once a day and continued for nearly one week until the urine was clear and odorless and the urine routine was normal. At the same time, according to the study by Xiang et al. (11), the family members were instructed to improve their bladder flushing home care methods and strictly hand hygiene and other operational procedures prone to urinary tract infection. After close monitoring, flushing on demand, and standardized intermittent catheterization for nearly one month, the patient had no more AD symptoms caused by urinary tract irritation. The patient resumed regular intermittent catheterization, reduced leakage, no obvious urinary tract infection was seen, and the results were satisfactory.
3. Discussion
Currently, the main treatment modality for patients with neurogenic bladder is intermittent catheterization (12-14). However, it often happens in the clinic for patients that do not follow the drinking and voiding schedule, and some patients prefer to receive catheterization according to their self-perception (15), which leads to the inability to control the safe bladder volume effectively. During the treatment and care of this patient, after discussion by the multidisciplinary team of medical, nursing, and rehabilitation physiotherapy, we considered the overall situation based on the results of the urodynamic examination, asynchronous cystography, and bladder scanner and actively provided personalized treatment plans to remove predisposing factors, reduce the risk of upper urinary tract damage, and put in place comprehensive care measures such as drinking plan, intermittent catheterization timing, and bladder flushing to achieve further regular storage, intermittent urinary control, and low-pressure voiding (16), so that the patient resumed regular intermittent catheterization, no more frequent AD symptoms, and reduced leakage, which played an active and effective role in maintaining normal bladder function in this patient and played an important role in the patient's disease regression and prognosis with satisfactory results.
The findings of this study highlight the importance of nursing interventions in managing patients with frequent AD during intermittent catheterization for cervical medullary injury. The nursing care plan implemented in this study involved a personalized approach to assessing the risk of abnormal AD based on urodynamic guidance and a bladder scanner, which proved effective in preventing AD. Previous studies also found that nursing intervention could improve the urinary incontinence of old patients (17, 18). Compared to that, this study provides the change in urinary state by measuring the urinary flow at different times before and after the nursing intervention. Additionally, the nursing interventions utilized in this study included active control of AD, prevention, early detection, acute episode management, timely adjustment of fluid intake, precise bladder care, selection of the best catheterization timing, patient education, and implementation of a personalized care plan. These interventions were successful in maintaining normal bladder function and preventing the occurrence of AD in the patient. The results of this study suggest that a comprehensive nursing care plan that includes personalized assessment and management of AD, as well as patient education, can effectively improve outcomes for patients with cervical medullary injuries who require intermittent catheterization. Future studies could further investigate the efficacy of these interventions in larger patient populations and evaluate their long-term effects on bladder function and overall quality of life.
3.1. Limitations/Future Directions
The current study has several limitations. This is a case report, and the results aimed to report the experience of only a single institution. Second, this study only reported the clinical outcomes of only one patient, which is a small number for generalization. Third, longer periods would contribute to obtaining more reliable results.