1. Background
Bipolar disorder is the sixth cause of disability worldwide among young adults and imposes a high social cost on the patients and their caregivers. It may occur in childhood but is more common in late adolescence and early adulthood (1). It is classically defined as clinical periods of depression and high mood (mania) interspersed with periods of natural mood (2). Bipolar disorder is a chronic, severe, and refractory mood disorder in which the main treatment goal is to prevent acute bouts and relapse (3, 4). In general, bipolar disorder is classified into two types: Type I, which requires at least one manic episode with or without a major depressive episode, and type II, which requires at least one hypomanic episode and one major depressive episode (5).
Patients with bipolar II disorder (BP-II) suffer from different problems, including emotional disorders, e.g., the loss of emotional self-regulation, which is an important process in research, treatment, psychopathology, and some physical pathology states (6, 7). Emotional self-regulation refers to actions that modify the intensity and type of emotional experiences (8, 9). This process is central to models of psychopathology, so much so that emotion regulation difficulty is regarded as the leading cause of disorders such as stress, anxiety, and depression (10). Emotional self-regulation involves all solutions and strategies for accepting, altering, and coping with stressful environments and events, which includes all internal and external processes responsible for maintaining, monitoring, appraising, and correcting emotional reactions (11). Emotion regulation is a key component of the coping process, playing an important role in normal and abnormal cognitive and emotional processes and making people respond more flexibly to environmental events, challenges, and stresses (12). Emotional self-regulation contributes to triggering, creating, increasing, maintaining, and decreasing positive and negative emotions in response to events (12, 13). In general, emotional self-regulation comprises two parts: Positive/adaptive and negative/maladaptive strategies. Maladaptive strategies, unlike adaptive ones, have a destructive impact on mental health, well-being, and quality of life (14).
Several methods are available to improve emotional and psychological traits, including emotional schema therapy and dialectical behavior therapy (15, 16). Emotional schema therapy is an integrative approach that combines and uses the strategies of cognitive-behavioral therapy, schema therapy, metacognitive model, and emotionally focused therapy (17). This therapy aims to identify and correct maladaptive beliefs and interpretations that disrupt emotional experiences; it also attempts to create new, adaptive, and flexible beliefs, interpretations, and strategies for emotional experiences (18, 19). Erfan et al. (20) concluded that emotional schema therapy can be an effective intervention for the treatment of mood symptoms and impulsivity in patients with bipolar disorder.
As an innovative cognitive-behavioral therapy, dialectical behavior therapy emphasizes the training of both individual and group skills and emotion regulation skills; the idea is that thoughts about and interpretations of positive and negative events affect health and psyche more than the external events themselves (21, 22). The goal of dialectical behavior therapy is to alleviate the suffering of people with emotional problems, improve their mental health, reduce negative emotions and experiences, and increase positive emotions (23, 24). Afshari et al. (22) reported that dialectical behavior therapy can effectively mitigate manic and depressive symptoms and improve executive functions in patients with bipolar disorder.
Studies show that less than half of patients with BP-II have demonstrated a favorable long-term response to treatment; even if treatment continues, many patients do not achieve complete recovery, and, at the same time, many patients have low acceptance of continuous drug treatments (25). The symptoms of BP-II, such as frequent episodes of depression, affect the cognitive regulation of emotions and quality of life. Few studies have examined cognitive emotion regulation in patients with BP-II in Iran. Given the necessity of psychotherapy interventions for patients with BP-II, an innovation of the present study was the comparison of emotional schema therapy and dialectical behavior therapy on these patients.
2. Objectives
Based on the issues outlined above, the present study aimed to investigate the effects of emotional schema therapy and dialectical behavior therapy on emotional self-regulation in patients with BP-II.
3. Methods
3.1. Study Design and Participants
This was an experimental study with a pretest-posttest design and a control group. The research population comprised patients with BP-II visiting counseling and psychology centers of Dezful (Iran) in 2022. The minimum sample size was estimated at 13 per group based on the study conducted by Akhavan and Sajjadian (26) with σ = 3.58 (standard deviation), d = 4.58 (experimental and control groups' posttest mean difference), test power = 0.90, and α = 0.05. However, considering the risk of attrition, the sample size for each group was increased to 15.
3.2. Sampling Method
The participants who met the inclusion criteria were selected via convenience sampling. A total of 45 patients with BP-II were selected and randomly assigned to three groups: Emotional schema therapy, dialectical behavior therapy, and control. A table of random numbers was used for the random allocation of participants. The inclusion criteria were a diagnosis of BP-II based on the diagnostic and statistical manual of mental disorders by a psychiatrist, having a minimum education level of a high-school diploma, age of 20 - 40 years, at least one year has passed since the onset of BP-II, no history of receiving emotional schema therapy or dialectical behavior therapy, and not using other treatment methods simultaneously. The exclusion criteria were missing more than one session, lack of cooperation, or withdrawal from participation. The Cognitive Emotion Regulation Questionnaire-short form (CERQ-short) was used to measure emotion regulation. All the groups filled out the questionnaire in two phases of pretest and posttest. The participants were assured of the confidentiality of their data and provided informed consent.
3.3. Intervention Programs
The first intervention program consisted of twelve 90-minute sessions of emotional schema therapy (Table 1). The emotional schemas sessions were developed by Leahy (17), and the Persian version of the sessions was provided by Khanzadeh et al. (27). The second intervention program consisted of eleven 90-minute sessions of dialectical behavior therapy (Table 2). This protocol was designed by Chapman (28); the intervention was used by Narimani et al. (29), and the results showed good validity.
| Sessions | Content |
|---|---|
| 1 | Introduction; establishing a therapeutic relationship; stating the rules of the sessions; introducing the emotional schema model; validating emotions; identifying emotional, cognitive, and behavioral symptoms of disorders; differentiating thoughts, feelings, and behaviors |
| 2 | Introducing emotional strategies, identifying the patients’ troublesome strategies and emotional schemata |
| 3 | Identifying techniques for using emotions, emotional labeling and observation, describing and recording emotions |
| 4 | Using emotion normalization and stress relief techniques, practicing stress relief in the face of stressful emotions |
| 5 | Challenging and coping with incorrect emotional beliefs, the emotion acceptance technique, recognizing the advantages and disadvantages of emotions and the misconceptions about them |
| 6 | A challenge to relieve the patients of troublesome strategies, training the tolerance of mixed feelings, identifying useful strategies for coping with emotions |
| 7 | A challenge to relieve the patients of troublesome strategies (contd.), recognizing misconceptions about and misinterpretations of emotions, negative emotional schemata |
| 8 | Challenging misconceptions about and misinterpretations of emotions (contd.), proper reactions to these misconceptions and misinterpretations, e.g., a sense of shame and guilt |
| 9 | Challenging misconceptions about and misinterpretations of emotions (contd.), using the technique of climbing the semiotic ladder and showing appropriate and adaptive behaviors in the face of positive beliefs and interpretations, e.g., greater values |
| 10 | Challenging misconceptions about and misinterpretations of emotions (contd.), creating a space for emotions, handing out a list of techniques and skills |
| 11 | Practicing the skills taught in previous sessions, review and summary of the sessions |
| 12 | Review and summary of the sessions, posttest |
| Sessions | Content |
|---|---|
| 1 | Introduction; establishing a therapeutic relationship; stating the rules of the sessions; introducing the general principles of dialectical behavior therapy; introducing the emotional, cognitive, and behavioral symptoms of disorders |
| 2 | Mindfulness training (emotional and wise awareness), attentional shift and distraction skills, description of emotions without judgment or evaluation |
| 3 | Examining and identifying thoughts and emotions, identifying internalizing and externalizing coping responses, examining thoughts and feelings that lead to emotional and self-destructive behaviors |
| 4 | Examining and identifying thoughts and feelings that lead to emotional and self-destructive behaviors, recording thoughts and feelings that lead to maladaptation |
| 5 | Distress tolerance and emotional management through mindfulness, relaxation, attentional shift, and distraction |
| 6 | Controlling impulsive behaviors and practicing their control and management |
| 7 | Identifying the consequences of emotion dysregulation, improving the use of emotion regulation processes, the outcomes of cognitive-behavioral avoidance, and planning to prevent it |
| 8 | Monitoring and managing one’s behaviors; identifying self-destructive behaviors and their consequences; reducing cognitive, behavioral, and emotional vulnerability; increasing positive emotions |
| 9 | Emotion regulation through the identification of emotions themselves, identifying the cause and purpose of emotions, reducing negative and increasing positive emotions |
| 10 | Providing emotional responses and transforming negative emotions into positive ones |
| 11 | Increasing the efficiency of interpersonal relationships by improving relations with friends and acquaintances, establishing interest-based relations, practicing the skills taught in the previous sessions, a summary of the sessions |
3.4. Instruments
Cognitive Emotion Regulation Questionnaire-short form: Developed by Garnefski and Kraaij (30) in 2006, this 18-item questionnaire assesses two dimensions of emotion regulation: Adaptive (10 items) and maladaptive (8 items). The items are scored on a five-point Likert scale from 1 (never) to 5 (always). The score of each dimension is the sum of the scores of the items. The final score ranges from 10 to 50 for the adaptive and from 8 to 40 for the maladaptive self-regulation dimension. A higher score indicates more adaptive or maladaptive emotion regulation. The CERQ-short was validated by Garnefski and Kraaij (30) and demonstrated satisfactory internal consistency (alphas ranged from 0.67 to 0.81) and criterion validity. Mohsenabadi and Fathi-Ashtiani (31) reported that the divergent and convergent validity of CERQ subscales had a significant correlation with Depression Anxiety Stress Scales. Moreover, the authors reported that the reliability coefficients (Cronbach's alpha) for adaptive and maladaptive coping strategies were 0.95 and 0.88, respectively (31). In the present study, Cronbach's alpha for this questionnaire was 0.89.
3.5. Data Analysis
The Shapiro-Wilk test was used to evaluate the normality of the data distribution. When the test assumptions were confirmed, an analysis of covariance with a Bonferroni post-hoc test was performed in SPSS v. 26 (IBM, Chicago, IL, USA) to compare the pretest and posttest data related to the dependent variables. The significance level was α = 0.05.
4. Results
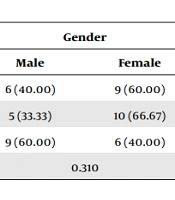
The participants included 45 men and women with BP-II with an average age of 29.62 ± 7.10 years. Table 3 shows the demographic variables of the participants in the experimental and control groups.
| Groups | Age (y) | Duration of Illness (y) | Education | Gender | ||
|---|---|---|---|---|---|---|
| High-school | Higher | Male | Female | |||
| Emotional schema therapy | 30.27 ± 6.84 | 4.18 ± 2.39 | 8 (53.33) | 7 (46.67) | 6 (40.00) | 9 (60.00) |
| Dialectical behavior therapy | 29.71 ± 7.11 | 3.75 ± 2.09 | 6 (40.00) | 9 (60.00) | 5 (33.33) | 10 (66.67) |
| Control | 28.87 ± 7.30 | 4.48 ± 2.41 | 9 (60.00) | 6 (40.00) | 9 (60.00) | 6 (40.00) |
| P | 0.792 | 0.742 | 0.791 | 0.310 | ||
a Values are expressed as mean ± standard deviation (SD) or No. (%).
Table 4 shows the mean and standard deviation (SD) of the pretest and posttest scores of the adaptive and maladaptive emotional self-regulation, divided by the emotional schema therapy, dialectical behavior therapy, and control groups.
| Cognitive Emotion Regulation and Phases | Emotional Schema Therapy Group | Dialectical Behavior Therapy Group | Control Group |
|---|---|---|---|
| Adaptive emotional self-regulation | |||
| Pretest | 16.60 ± 3.04 | 17.73 ± 3.15 | 18.46 ± 3.66 |
| Posttest | 20.60 ± 2.99 | 21.60 ± 3.33 | 18.06 ± 3.36 |
| P b | 0.001 | 0.003 | 0.757 |
| Maladaptive emotional self-regulation | |||
| Pretest | 16.20 ± 2.90 | 17.26 ± 2.89 | 15.80 ± 2.51 |
| Posttest | 12.66 ± 2.22 | 14.13 ± 2.35 | 16.13 ± 2.64 |
| P b | 0.001 | 0.003 | 0.728 |
a Values are expressed as mean ± standard deviation (SD).
bt-test.
The Shapiro-Wilk test confirmed the assumption of the normality of distribution of the research variables, i.e., adaptive (W = 0.963, P = 0.826) and maladaptive (W = 0.968, P = 0.879) emotional self-regulation, on the pretest and posttest, divided by the groups. There was a significant difference between the experimental and control groups in terms of adaptive (F = 129.29, P = 0.001) and maladaptive (F = 97.31, P = 0.001) emotional self-regulation (P < 0.001; Table 5).
| Variables and Source | SS | df | MS | F | P | η2 | Power |
|---|---|---|---|---|---|---|---|
| Adaptive emotional self-regulation | |||||||
| Posttest | 386.50 | 1 | 386.50 | 560.85 | 0.001 | 0.94 | 1.00 |
| Group | 178.20 | 2 | 89.10 | 129.29 | 0.001 | 0.87 | 1.00 |
| Error | 26.19 | 38 | 0.69 | ||||
| Maladaptive emotional self-regulation | |||||||
| Posttest | 195.91 | 1 | 195.91 | 301.53 | 0.001 | 0.89 | 1.00 |
| Group | 126.45 | 2 | 63.22 | 97.31 | 0.001 | 0.84 | 1.00 |
| Error | 24.69 | 38 | 0.65 |
Table 6 presents the results of the Bonferroni post-hoc test to compare the effects of the interventions on each dependent variable. A comparison of the means of the two experimental groups showed that both interventions almost equally increased adaptive and decreased maladaptive self-regulation in the patients with BP-II (P < 0.001). There was no significant difference between the effects of emotional schema therapy and dialectical behavior therapy on adaptive (P = 0.999) and maladaptive (P = 0.078) emotional self-regulation of patients with BP-II (P < 0.001) (Table 6).
| Cognitive Emotion Regulation and Groups | Mean Difference | SE | P |
|---|---|---|---|
| Adaptive emotional self-regulation | |||
| Emotional schema therapy - dialectical behavior therapy | -0.095 | 0.313 | 0.999 |
| Emotional schema therapy - control | 4.407 | 0.314 | 0.001 |
| Dialectical behavior therapy - control | 4.502 | 0.322 | 0.001 |
| Maladaptive emotional self-regulation | |||
| Emotional schema therapy - dialectical behavior therapy | -0.705 | 0.304 | 0.078 |
| Emotional schema therapy - control | -4.033 | 0.305 | 0.001 |
| Dialectical behavior therapy - control | -3.328 | 0.313 | 0.001 |
Abbreviation: SE, standard error.
5. Discussion
The present study investigated the effects of emotional schema therapy and dialectical behavior therapy on emotional self-regulation in patients with BP-II. Emotional schema therapy and dialectical behavior therapy both decreased the maladaptive and increased the adaptive emotional self-regulation of the patients, and there was no significant difference between the two interventions. In line with these results, Ghasemkhanloo et al. (32) reported that emotional schema therapy effectively reduced depression and maladaptive strategies of cognitive emotion regulation in patients with major depressive disorder. Moreover, Narimani et al. (29) reported that dialectical behavior therapy effectively alleviated maladaptive strategies and increased adaptive cognitive, emotional regulation strategies in methamphetamine abusers.
A central strategy and main pillar of dialectical behavior therapy is emotion regulation. Examples of techniques used for emotion regulation are busying oneself by calling a friend or cleaning the room, engaging in tasks such as cooking, comparing oneself with those who are in a worse situation, intentionally fostering positive emotions by watching a movie, temporarily suppressing painful situations by building up an imaginary wall between oneself and situations or problems, replacing thoughts, and strengthening other senses such as listening to loud music (16). These techniques can manage and transform negative emotions into positive ones in patients with BP-II. Emotion regulation can increase patients' skills in controlling negative emotions in interpersonal relationships. Training interpersonal skills to patients with BP-II also boosts their ability to solve interpersonal conflicts and boosts self-confidence, all of which enhance emotion regulation by improving social relations (22).
Dialectical behavior therapy aims to alleviate the suffering of people who have emotional problems, improve their mental health, reduce their negative emotions and experiences, and increase their positive emotions (24). Dialectical behavior therapy, especially the skills of mindfulness and emotional regulation, makes patients with BP-II pay more attention to their current emotional needs (24). As such, patients with BP-II can make a mindful decision and, by practicing the technique and skills of distress tolerance and interpersonal relationships, they can implement effective coping strategies in the right situation. In this therapy, patients with BP-II can overcome distressing emotions and face challenging situations by using self-talk and self-soothing techniques (32). Dialectical behavior therapy can thus regulate emotions in patients with BP-II through appropriate solutions and strategies.
Emotional schema therapy is an integrative approach that combines the strategies of cognitive-behavioral, metacognitive, and emotionally focused therapies. According to this therapeutic approach, when an emotion is evoked, interpretations, reactions, and emotion regulation strategies determine whether the emotion will persist, intensify, or diminish (20). In this therapy, the therapist uses emotion induction and normalization techniques as important elements to motivate and express emotions. To improve emotion regulation strategies, the therapist prepares patients with BP-II cognitively to accept emotions and thoughts by explaining the disadvantages of suppression, inefficient coping strategies, distinguishing between thoughts and emotions, catastrophizing, and connecting emotional schemas with ineffective barriers (15). The core of emotional schema therapy is emphasizing emotion regulation, especially emotion acceptance. Therefore, by using techniques such as mindfulness and acceptance of effective and ineffective emotions, this treatment helps patients with BP-II to identify and gain a conscious view of their emotions (31).
Emotional schema therapy and dialectical behavior therapy were derived from the third wave of psychotherapy and share many principles and benefits; as such, both methods effectively and equally reduced maladaptive emotional self-regulation and increased adaptive emotional self-regulation in patients with BP-II. The main concepts and advantages of emotional schema therapy include introducing emotional schemata; recognizing emotional symptoms; differentiating thoughts, feelings, and behaviors; identifying negative emotional schemata; becoming aware of emotional strategies; identifying emotional schemata; and the techniques of using emotions (15). Moreover, the main concepts and advantages of dialectical behavior therapy include introducing the general principles of dialectical behavior therapy; introducing emotional symptoms; training mindfulness and the skill of attentional shift; managing emotions through mindfulness, attentional shift, and relaxation; and recognizing the consequences of emotion dysregulation.
This research was not free from limitations, including the limitation of the scope of the study to patients with BP-II in Dezful (Iran) and not using random sampling. Moreover, some demographic characteristics, e.g., socioeconomic status, which the researcher could not control, may have affected the results. Similar studies on patients with BP-II should be conducted in other cities with different cultural and social structures to better generalize the results.
5.1. Conclusions
According to the concepts and advantages of the two treatments, both are expected to improve emotional traits. Since emotional self-regulation is part of emotional traits, both methods can almost equally reduce maladaptive and increase adaptive emotional self-regulation in patients with BP-II. Therefore, it is suggested that counselors, therapists, and healthcare professionals administer one or both interventions to alleviate maladaptive emotional self-regulation, promote adaptive emotional self-regulation, or improve other psychological variables in patients with BP-II.