1. Background
Lung isolation techniques are designed to provide one-lung ventilation (OLV) in patients undergoing thoracic surgery. One-lung ventilation is often required to facilitate surgical exposure. It may also protect the other lung, on the opposite side of surgery, from becoming contaminated, e.g., in the case of bronchopleural fistula. Isolation can be achieved by using double-lumen endobronchial tubes (DLTs) as the most commonly used technique (1), a bronchial blocker (BB), and single-lumen endo¬bronchial tubes (SLTs). Hypoxemia is a common disorder during thoracic surgery defined as a decrease in oxygen saturation (SpO2) measured by pulse oximetry of less than 85 to 90% (2). It may also be defined as an arterial oxygen tension (PaO2) of less than 60 mmHg when the patient is being ventilated at an inspired oxygen fraction (FiO2) of 1.0. (3). Right-sided surgery (right lung collapse) and left-sided ventilation (4), low PaO2 before OLV, body mass index (BMI) (5), and the patient’s position during surgery (6) are among the factors that may predict the possibility of hypoxia during OLV. Hypoxemia (oxygen saturation <90%) during OLV in the lateral position is seen in 1-9% of patients (7, 8). It is not exactly clear how patient position affects the intensity of hypoxemia during OLV. In the lateral position, the majority of the ventilation is applied to the upper lung, whereas the lower lung is hypoventilated. The blood flow, based on gravitational blood distribution, drops in the non-dependent upper lung (9) and decreases arterial oxygenation (10).
However, it is not clear how patient position affects the intensity of hypoxemia during OLV. In general, PaO2 gradually declines after the beginning of OLV toward a plateau value that matches the ratio of ventilation and perfusion in the ventilated lung (11). The patient’s position during surgery influences the plateau value and PaO2 reduction rate after changing the ventilation to OLV because the distribution of pulmonary perfusion between dependent and non-dependent lungs is affected by gravity (12).
Patients with chronic pulmonary obstructive disease (COPD) have been shown to be less prone to hypoxemia during OLV (13). Smoking is the most important risk factor, and about 50% of smokers develop COPD. It is less clear how a patient’s position affects the PaO2 and intensity of hypoxemia in patients with a positive history of smoking. Although several studies have been conducted on patients undergoing thoracic surgery in recent years, the effect of position on arterial oxygen pressure (PaO2) has not been evaluated separately in two groups of smokers and nonsmokers.
2. Objectives
We hypothesized that changing from the supine to the lateral position during OLV and two-lung ventilation (TLV) in thoracic surgery under general anesthesia would affect PaO2 in two groups of smoker and nonsmoker patients.
3. Methods
3.1. Study Design
This single-blinded prospective pilot study was approved by the Ethics Committee of the Shiraz University of Medical Sciences, Shiraz, Iran (IR.SUMS.MED.REC.1397.464).
The patients were divided into 2 groups of smokers (≥ 40 packs/year) and nonsmokers, with 15 members each. Anesthesia was induced with midazolam (0.02 mg/kg), fentanyl (1 - 3 μg/kg), and morphine (0.1 mg/kg) as premedication, and sodium thiopental (3 - 5 mg/kg) as induction. Tracheal intubation was facilitated with atracurium (0.5 - 0.6 mg/kg). One-lung ventilation was performed using an appropriate size of DLT (according to the patient’s sex and height), guided, and confirmed to be at the correct position of DLT by a fiberoptic bronchoscope and auscultation. General anesthesia was maintained with an infusion of propofol (50 - 150 μg/kg/min) and remifentanil (0.1 - 0.3 μg/kg/min). Before induction of anesthesia, a 20-gauge radial artery catheter was placed after the local injection of 1 cc of lidocaine 2%. The lungs were ventilated with volume-controlled ventilation, a tidal volume (TV) of 5 - 6 ml/kg ideal body weight, fractions of inspired oxygen (FiO2) of 1.0, peak airway pressure < 30 cmH2O, plateau airway pressure < 25 cmH2O, inspiratory/expiratory (I/E) ratio of 1: 2, an inspiratory pause of 10% of the total inspiration time, respiratory rate (RR) of 10 - 12 breaths/minute, and positive end-expiratory pressure (PEEP) of 5 - 10 cmH2O. The respiratory rate was adjusted to maintain an end-tidal CO2 (EtCO2) of 35 - 40 mmHg.
3.2. Participants
Adult patients (≥ 18 years old) with the American Society of Anesthesiologists (ASA) physical status of I and II and preoperative SpO2 > 90% who underwent thoracotomy under general anesthesia were included. They had no positive history of cardiovascular or liver disease, renal failure, seizure or other neurologic disorders, or allergic reactions to the study agents. Patients who were unable to communicate or refused to participate were excluded.
3.3. Data Collection
Hemodynamic data (systolic arterial pressure, diastolic arterial pressure, and heart rate), PaO2, and SpO2 were recorded at the following points: (1) baseline: Before the induction of anesthesia in the supine position, (2) 5 min after the supine position in TLV and (3) OLV, (4) 5 min after the lateral position in TLV and OLV (5). Blood sampling from an arterial catheter was performed to obtain blood specimens for arterial blood gas (ABG) analysis or for other laboratory testing. Blood gases were processed within 5 minutes of extraction, and the values were corrected for body temperature.
3.4. Data Analysis
The data were analyzed in SPSS v. 19 (SPSS Inc. Chicago, Il, USA). The mean values of each continuous variable in smokers vs. nonsmokers were calculated and compared parametrically using the t-test, and within groups, a comparison was performed by the paired t-test. A P-value of less than 0.05 was considered statistically significant.
3.5. Ethical Consideration
The study was approved by the Ethics Committee of the Shiraz University of Medical Sciences, Shiraz, Iran (IR.SUMS.MED.REC.1397.464). The participants provided written informed consent before enrolment in the study. All the steps of the study were performed according to the Declaration of Helsinki.
4. Results
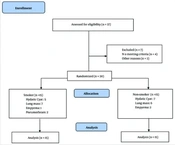
Thirty patients were enrolled in the study and divided into two groups of smokers and nonsmokers (Figure 1).
Table 1 shows the patients’ characteristics and preoperative hemodynamics in both groups. No statistical differences were observed between smokers and nonsmokers regarding the demographic data.
| Demographic Data | Smoker (N = 15) | Nonsmoker (N = 15) | P-Value |
|---|---|---|---|
| Male/female | 12/3 (80/20) | 9/6 (60/40) | 0.23 |
| Age (y) | 42.4 ± 17.7 | 36.07 ± 15.06 | 0.30 |
| SBP (mmHg) | 127.17 ± 15.39 | 119.93 ± 1.96 | 0.16 |
| HR (beats/min) | 81.40 ± 20.13 | 81.60 ± 21.29 | 0.97 |
Abbreviations: N, number of patients (percentage); Hb, hemoglobin, SBP, systolic blood pressure, HR, heart rate.
a The values are expressed as means ± standard error of the mean (SEM).
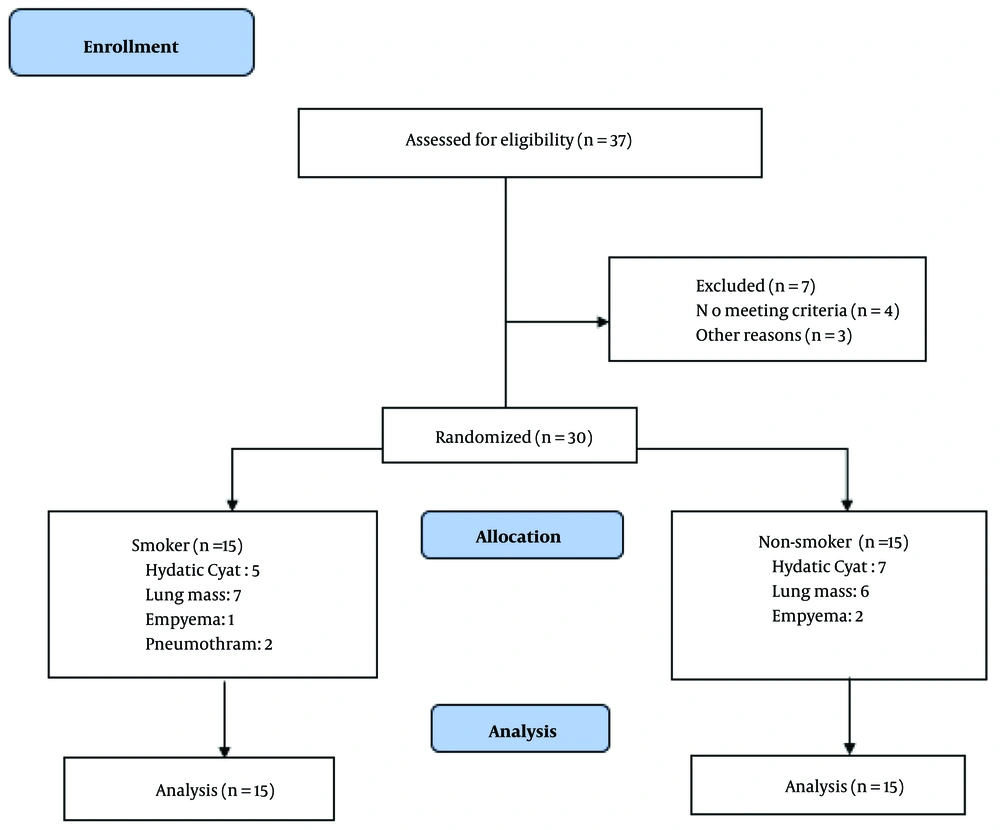
Figure 2 shows the PaO2 levels in two smoker and nonsmoker groups during OLV and TLV in the lateral and supine positions. Except during supine TLV, PaO2 levels were higher in smokers than in nonsmokers (Figure 1). These differences were clinically significant.
The levels of PaO2, PaCO2, and SpO2 were compared during one- and two-lung ventilation techniques in the supine and lateral positions, separately in smoker and nonsmoker patients. Changing the position from supine to lateral caused a relative decrease in PaO2 (except during TLV in the smoker group) during TLV and OLV (Table 2). The reduction in PaO2 levels when switching from supine TLV to lateral OLV (72.12 mmHg) was less in smoker patients than in nonsmoker ones (95.28 mmHg).
| Variables | Ventilation | Position | PaO2 (mmHg) (Mean ± SD) | P-Value a |
|---|---|---|---|---|
| Smokers (n = 15) | TLV | Supine | 218.87 ± 64.96 | 0.375 |
| Lateral | 228.83 ± 65.43 | |||
| OLV | Supine | 169.31 ± 74.59 | 0.149 | |
| Lateral | 146.74 ± 76.90 | |||
| Nonsmokers (n=15) | TLV | Supine | 219.27 ± 47.29 | 0.059 |
| Lateral | 177.34 ± 77.13 | |||
| OLV | Supine | 135.73 ± 51.08 | 0.461 | |
| Lateral | 123.98 ± 38.30 |
Abbreviations: OLV, one-lung ventilation; TLV, two-lung ventilation; n, number.
at-test.
As shown in Table 3, changing the position from supine to lateral resulted in a nonsignificant decrease in SpO2. However, the reduction in SpO2 when switching from supine TLV to lateral OLV was less in smokers (99.02 ± 0.66 to 97.75 ± 1.27) than in nonsmokers (98.76 ± 1.97 to 96.50 ± 2.83).
| Variables | Ventilation | Position | PaO2 (mmHg) (Mean ± SD) | P-Value a |
|---|---|---|---|---|
| Smokers (n = 15) | TLV | Supine | 99.02 ± 0.66 | 0.446 |
| Lateral | 98.82 ± 0.86 | |||
| OLV | Supine | 98.22 ± 1.26 | 0.452 | |
| Lateral | 97.75 ± 1.27 | |||
| Nonsmokers (n = 15) | TLV | Supine | 98.76 ± 1.97 | 0.221 |
| Lateral | 97.27 ± 1.98 | |||
| OLV | Supine | 97.43 ± 1.66 | 0.245 | |
| Lateral | 96.50 ± 2.83 |
Abbreviations: OLV, one-lung ventilation; TLV, two-lung ventilation; n, number.
at-test.
The partial pressure of carbon dioxide (PaCO2) levels were higher in smokers than in nonsmokers, although changing the position from supine to lateral did not affect the PaCO2 levels (Table 4).
| Variables | Ventilation | Position | PaO2 (mmHg) (Mean ± SD) | P-Value a |
|---|---|---|---|---|
| Smokers (n = 15) | TLV | Supine | 38.91 ± 6.53 | 0.554 |
| Lateral | 38.11 ± 7.06 | |||
| OLV | Supine | 41.43 ± 5.42 | 0.722 | |
| Lateral | 40.69 ± 6.64 | |||
| Nonsmokers(n = 15) | TLV | Supine | 35.09 ± 6.98 | 0.058 |
| Lateral | 35.73 ± 7.06 | |||
| OLV | Supine | 39.15 ± 6.75 | 0.068 | |
| Lateral | 36.93 ± 5.36 |
Abbreviations: OLV, one-lung ventilation; TLV, two-lung ventilation; n, number.
at-test.
5. Discussion
The vast majority of thoracic procedures are performed with the patient in a lateral position, with few exemptions, i.e., bilateral lung transplant done in a supine position. Hypoxemia during OLV occurs in about 10% of cases (14). Right-sided thoracotomy (right lung collapse) and left-sided ventilation, restrictive lung disease, and the patient’s position during surgery (1) are factors associated with oxygen desaturation during OLV. However, it is less clear how the patient’s position affects the intensity of hypoxemia during OLV and TLV in smoker and nonsmoker patients.
In this study, we compared the levels of PaO2, PaCO2, and SpO2 in both smokers and nonsmokers during one- and two-lung ventilation techniques in the supine and lateral positions. We found that PaO2 had a higher level in smokers than in nonsmokers in most of the studied conditions, especially during TLV in the lateral position. Although this difference was not statistically significant, it was clinically significant.
Patients with obstructive lung disease had lower forced expiratory volume in 1 s (FEV1), and the auto-PEEP in them causes air-trapping, reduces atelectasis, and, thus, improves oxygenation. Air trapped in the nonventilated lung tends to delay the onset of desaturation and hypoxemia (15).
Our data suggested that the effect of different positions on arterial oxygenation in smoker and nonsmoker patients during OLV and TLV was not statistically significant. However, changing from the supine to the lateral position affected PaO2 and caused a relative decrease in PaO2, and this was particularly pronounced in patients with normal pulmonary function during TLV. In contrast, in a study on patients with a lung mass, PaO2 was significantly higher in left and right lateral decubitus positions than in the supine position (16). Rossi et al. declared that the lateral decubitus position was preferred for open thoracic surgery to maintain high PaO2 levels during OLV (12). In these studies, no comparison was made between smokers and nonsmokers.
Hypoxemia during OLV is caused by venous admixture through shunts and areas of low ventilation/perfusion (V/Q) gas-exchanging units [18]. It has been reported that the increased use of the supine position may adversely affect the prevalence of hypoxemia (14); patients who are well-oxygenated during TLV will have a PaO2 of approximately 350 - 400 mmHg, and when it is converted to OLV, they will have a PaO2 of approximately 150 - 200 mmHg while receiving FiO2 1.0 (18).
Bardoczky et al. evaluated oxygenation during OLV and TLV in the supine and lateral positions when they used three FiO2 values. Arterial oxygen pressure decreased in all the groups during OLV compared to the TLV, but the rate of decline was significantly lower in the lateral position compared to the supine position (12).
Our study had some limitations. The main limitation was the small sample size. Due to the outbreak of the coronavirus disease 2019 (COVID-19), we could not recruit enough participants.
5.1. Conclusions
The present study showed that in patients undergoing open thoracotomy under general anesthesia by the DLT technique, the PaO2 level was higher in smokers than nonsmokers. Moreover, the effect of patient position on PaO2 during OLV and TLV in both smokers and nonsmokers was not significant.