1. Background
A stroke, also known as a cerebrovascular accident, is the abrupt onset of a neurological disorder that can be traced back to a focal vascular cause. Ischemic stroke is one of the most common vascular disorders of the brain (1). This chronic condition can affect all aspects of a person’s life and family (2). The alterations in mentality, cognition, and mobility, in turn, affect one’s ability to care for oneself, body perception, level of activity, and overall sense of recovery. As a result, the individual’s roles and responsibilities within their family and society are disrupted, leading to inefficiency and reduced Quality of Life (QoL) (3). The QoL, which refers to an individual’s perception of themselves, is influenced by cultural and value systems. In turn, a person’s goals, standards, and desires are significantly impacted by their physical and mental well-being, level of independence, social relationships, and personal beliefs (4). Studies have shown that stroke lowers the QoL in three dimensions: Physical, mental-spiritual, and social (5, 6).
Every year, over 400,000 individuals are discharged from the hospital following acute stroke episodes, experiencing varying degrees of disorder and physical disabilities. Around 30% of individuals recover, while approximately 40% remain disabled (7). Interventions have the potential to enhance QoL, expedite recovery, decrease hospitalization duration, and ultimately lower patient costs. The Mindfulness-based Stress Reduction (MBSR) intervention, which is delivered to patients in the field of consciousness, provides patients with a focused, flexible, and moment-to-moment revelation of the flow of thoughts, feelings, and physical sensations. Mindfulness-based interventions induce positive changes in psychological functions and promote self-management and adaptability (8, 9). Initially, MBSR was developed to improve psychological functions by integrating conventional mindfulness exercises. Introduced by Kabat-Zinn way back in 1990, MBSR has been supported by research evidence indicating its effectiveness in addressing a broad spectrum of clinical and non-clinical psychological symptoms (10).
Cognitive rehabilitation therapy (CRT) is another method used to improve psychological characteristics and restore lost cognitive capacities by providing targeted stimuli and specific exercises (11). Cognitive and psychological problems can be addressed through CRT, a treatment method that focuses on restoring or compensating for damaged functions. This is achieved through rigorous training, repetition, and practice (12). This intervention encompasses a complex array of methods aimed at enhancing comprehension, understanding, attention, learning, recall, and problem-solving abilities (13). Also, CRT starts and concludes with assessments. The assessment encompasses various aspects such as self-awareness, orientation, attention, forgetting, visual and motor processing, planning, memory, organization, and problem-solving (14).
2. Methods
A pretest-posttest quasi-experimental study was conducted with a follow-up period. Three groups were considered in the study, namely MBSR, CRT, and control. The statistical sample was selected from ischemic stroke patients referred to the neurology department and clinic of Razi Hospital in Birjand from June 2018 to June 2021. Based on the inclusion criteria, 36 patients were selected purposively and assigned to study groups using a simple randomization method. All the listed people were then assigned to the three groups of MBSR, CRT, and control by lottery, with 12 people in each group. The target sample was determined to be 12 per group using Cohen’s table taken from Stevens, considering the minimum power of the test (74%), average effect size, and attrition probability. The inclusion criteria included the following: first ischemic stroke, diagnosis based on either MRI or CT scan, a period of at least six months but no more than three years since the stroke, an age range of 40 to 70 years, having at least a secondary education level, receiving the same drug treatment, confirmation of memory and attention disorder, absence of verbal, motor, or hearing disability, and absence of alcohol and drug addiction. The exclusion criteria included the following: absence from more than three sessions, reluctance to undergo treatment, occurrence of severe stress, memory improvement prior to the completion of the intervention, and experiencing another stroke.
Because of the coronavirus epidemic, patients were invited over the phone to cooperate. Before the interventions, explanations were provided regarding the objectives, duration of the research, research procedure, cooperation guidelines, and the confidentiality of information. After providing informed consent, the subjects completed the demographics form and the Stroke-specific QoL (SS-QOL) scale. The MBSR and CRT interventions were delivered as 12-week programs, one hour per week, over three months. The control group received drug treatment without any additional intervention. Two months after the completion of the interventions, a meeting was convened to conduct a general evaluation and assess the effectiveness of the interventions. Subsequently, the questionnaires were once again completed.
- Demographic characteristics form
The included specifications encompassed factors such as age, gender, marital status, number of children, occupation, level of education, income, place of residence, housing status, duration of illness, and history of physical and mental illness.
- Stroke-specific Quality of Life Scale
The scale, developed by Williams et al. in 1999, consists of 49 items to assess the QoL of stroke patients. These items are scored on a 5-point Likert scale, ranging from strongly disagree to strongly agree (15). In the Iranian context, the instrument was first used by Azimi Ghandomani et al. The Cronbach’s alpha coefficient was reported to be 0.95, indicating high internal consistency. Additionally, a correlation coefficient of 0.68 was observed. The questionnaire was administered to 12 experts to evaluate its content and formal validity and 10 patients to evaluate its reliability; the test-retest coefficient was 0.78, and Cronbach’s alpha was 0.90 (4).
- Mindfulness-based Stress Reduction
Mindfulness-based stress reduction is an effective intervention in treating psychological complications associated with chronic diseases. It was developed by Kabat-Zinn to reduce stress and pain symptoms. It is a multi-component therapy delivered in groups (16). This intervention aims to help people accept and communicate with their inner experiences and increase their awareness of conscious behaviors (17). Mindfulness meditation has been shown to enhance an individual’s attention, thereby fostering heightened awareness and emotional capacity (18). Sisk acknowledges that mindfulness can provide insight to assist individuals in anticipating and creating a new approach to life and a different way of living (19). In the present study, the intervention was carried out in accordance with the protocols of Kabat Zinn (20) and Stahl and Goldstein (21) (Table 1).
| Sessions | Content |
|---|---|
| 1 | Introduction and communication between members, administration of a pretest, mindfulness training, mindful breathing and feedback, assignment of homework (meals to be taken mindfully), distribution of educational pamphlets and CDs |
| 2 | Homework review, explanation about stress, mindful breathing, mindful eating and feedback, homework (10-15 minutes of mindful breathing every day, mindfulness in daily activities: brushing teeth, showering, washing dishes), distribution of educational pamphlets and CDs |
| 3 | Homework review, explanation about anxiety, body scan meditation, mindfulness to sounds and thoughts, homework (taking notes of pleasant experiences, the way events happen, degrees of awareness, emotions, thoughts, and reactions), distribution of educational pamphlets and CDs |
| 4 | Homework review, explanation about depression, mindful walking meditation and feedback, STOP meditation, homework (taking notes of unpleasant experiences, the way events happen, degrees of awareness, feelings, thoughts, and reactions), distribution of educational pamphlets and CDs |
| 5 | Homework review, explanation of attention, mindful sitting and feedback, meditation to bring the eight attitudes to life, homework (engaging in the three-minute breathing space and body scan at least three times a day), distribution of educational pamphlets and CDs |
| 6 | Homework review, explanation of memory, mindful yoga and feedback, pain awareness meditation, homework (being mindful of daily activities: brushing, showering, washing dishes, and mindful breathing meditation), distribution of educational pamphlets and CDs |
| 7 | Homework review, explanation of executive functions, conscious self-questioning and feedback, RAIN meditation, homework (checking the conscious mind, practicing the three-minute breathing space), distribution of educational pamphlets and CDs |
| 8 | Homework review, loving-kindness meditation, and feedback, habits awareness meditation, homework (practicing mindful sitting with awareness of breathing, body, sounds, and thoughts; integrating mindfulness into all daily activities), distribution of educational pamphlets and CDs |
2.1. Powell’s Cognitive Rehabilitation Training
The cognitive rehabilitation intervention is a therapeutic system that uses brain-behavior relationships to facilitate performance change. This is achieved through various processes, including the creation or reinforcement of previously learned behavioral patterns, the development of new cognitive patterns using compensatory cognitive mechanisms, the establishment of new activity patterns through external compensatory mechanisms, and the facilitation of individuals in compromising with their cognitive disability to enhance overall performance (22). The basis for improving cognitive deficits through CRT lies in the brain’s neural flexibility property. The foundation of behavioral and structural changes in the brain is rooted in dendritic and synaptic fibers (23). The current study administered CRT following Powell’s rehabilitation protocol (24) (Table 2).
| Exercises | Cognitive Skills | Instruction |
|---|---|---|
| Memory, session | ||
| 1 | 1- Remembering daily activities, 2- Remembering arrangements, 3- Assigning homework | 1- Provide information about yourself for other members to remember at the end of the session., 2- Create an alphabetical shopping list, recalling the sequence of movements or sounds, recalling the order of words in the form of a story, and creating a shopping list |
| 2 | 1- Recalling pictures, 2- Recalling people’s names from their faces, 3- Examining assignments | 1. Examine the image for one minute; recall the details immediately and thirty minutes later., 2- Look at the pictures with names for a few minutes; then, recall the faces of people without names. |
| 3 | 1- Segmentation, 2- News report, 3- Examining assignments | 1- Memorize the set of pictures by dividing them into small groups or putting them into categories (immediately and 30 minutes later) 2- Read a paragraph and then tell about it. |
| 4 | 1- Remembering numbers, 2- Using memory aids, 3- Examining assignments | 1- Techniques to recall numbers: Segmenting, relating, using rhythm, visualizing the pattern, 2- Use educational aids: Notepads, tagging, indexing, calendars, and messaging devices |
| Attention, session | ||
| 1 | 1- Latent words, 2- Examining assignments | Concentration enhancement exercise: Find the words in the list that have shared characteristics and mark them with underlines and crosses. |
| 2 | 1- Counting of “s”, 2- Examining assignments | Count the number of times the proposition “from” is used in the excerpt that is read aloud. |
| 3 | 1- Remembering, 2- Division and change of attention, 3- Examining assignments | 1- Exercise to improve the ability to think of two things or more at a time, 2- Review the letters of the alphabet and consider names that begin with these letters. |
| 4 | 1- Practicing several previous stimuli, 2- Examining assignments | Exercise for sustained attention: Step one: Preparation; step two: One return; step three: Two returns |
3. Results
A total of 33 people (10 people in the intervention group 1, 11 people in the intervention group 2, and 12 people in the control group) participated in the study. The frequency distribution of the participants according to gender, age group, education level, and marital status is shown in the table below. According to the chi-square test, there was no significant difference in gender, age groups, and education level distribution between the study groups (Table 3).
| Variables | No. (%) | P-Value | ||
|---|---|---|---|---|
| Experimental CRT | Experimental MBSR | Control | ||
| Sex | 0.73 | |||
| Male | 4 (40) | 4 (36.4) | 3 (25) | |
| Female | 6 (60) | 7 (63.6) | 9 (75) | |
| Age groups | ||||
| 40 - 50 | 4 (40) | 3 (27.3) | 3 (25) | 0.77 |
| 51 - 60 | 2 (20) | 5 (45.4) | 5 (41.7) | |
| 61 - 70 | 4 (40) | 3 (27.3) | 4 (33.3) | |
| Education level | 0.99 | |||
| High school | 1 (10) | 2 (18.2) | 2 (16.66) | |
| Diploma | 3 (30) | 3 (27.3) | 3 (25) | |
| Associate degree | 1 (10) | 1 (9) | 2 (16.66) | |
| Bachelor’s degree | 3 (30) | 3 (27.3) | 3 (25) | |
| Master’s degree or higher | 2 (20) | 2 (18.2) | 2 (16.66) | |
| Marital status | 0.40 | |||
| Married | 10 (100) | 10 (90.9) | 10 (83.3) | |
| Single | - | 1 (9.1) | 2 (16.7) | |
3.1. Examining the Assumptions of the Repeated Measures Analysis
The significance level of the Shapiro-Wilk test for the groups in all three stages was greater than 0.05, confirming the normality of the data on the QoL in the experimental and control groups. The significance level of the Box’s M test was 0.118, indicating that the QoL did not change over time in any of the three groups. The significance level for QoL in Mauchly’s sphericity test was 0.000, indicating that the null hypothesis based on the sphericity of the variance-covariance matrix was not supported. The significance level for the pretest in Levene’s test was greater than 0.05, suggesting the homogeneity of the error variances; however, the significance level for the posttest and follow-up was less than 0.05, indicating the non-homogeneity of the error variances in these two stages.
| Groups | Indicator (Mean ± SD) | P-Value |
|---|---|---|
| Experimental CRT | 0.103 | |
| Pretest | 176.30 ± 19.49 | |
| Posttest | 182.50 ± 23.42 | |
| Follow-up | 180.70 ± 22.10 | |
| Experimental MBSR | ||
| Pretest | 179.64 ± 20.68 | |
| Posttest | 191.91 ± 11.67 | |
| Follow-up | 187.36 ± 8.95 | |
| Control | ||
| Pretest | 187.50 ± 14.67 | |
| Posttest | 186.50 ± 11.63 | |
| Follow-up | 183.58 ± 15.19 |
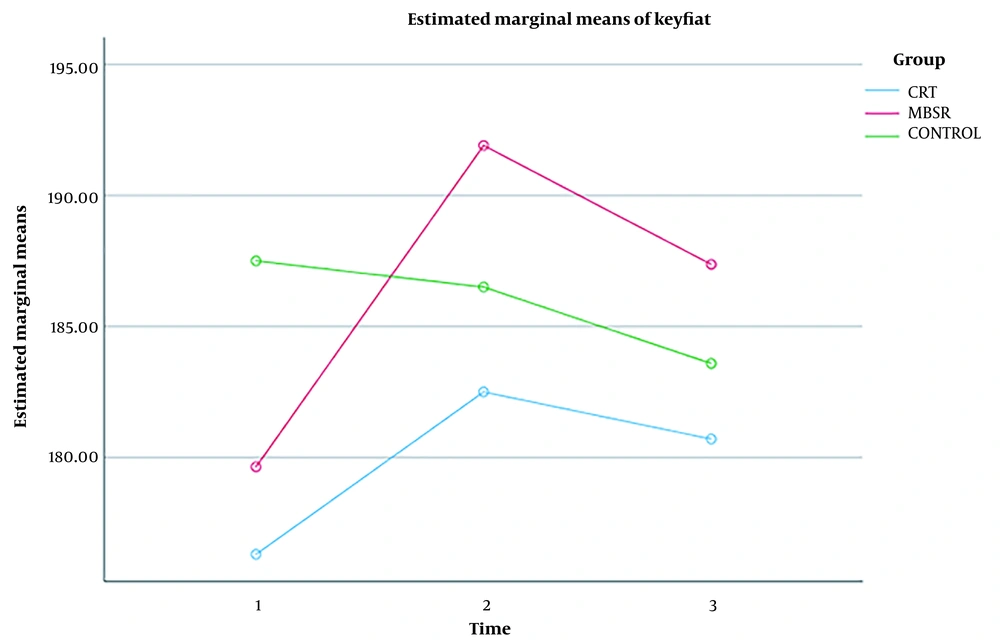
Table 4 displays the interpretation of the results of the repeated measures analysis of variance. The significance level was greater than 0.05, indicating that this variable had no effect on the means and that the QoL scores of the three groups studied did not differ significantly over time.
The Bonferroni test was used to assess the stability of effectiveness and changes in study groups over the three time periods. The results of this test showed only a statistical difference between the posttest and follow-up in the mindfulness group (Table 5).
| Groups | Category | Differences in Means | Standard Error | P-Value |
|---|---|---|---|---|
| Cognitive rehabilitation | ||||
| Pretest | Posttest | - 6.200 | 4.921 | 0.718 |
| Follow-up | - 4.400 | 4.458 | 1 | |
| Posttest | Pretest | 6.200 | 4.921 | 0.718 |
| Follow-up | 1.800 | 2.065 | 1 | |
| Follow-up | Pretest | 4.400 | 4.458 | 1 |
| Posttest | - 1.800 | 2.065 | 1 | |
| Mindfulness | ||||
| Pretest | Posttest | - 12.273 | 4.679 | 0.076 |
| Follow-up | - 7.727 | 5.002 | 0.460 | |
| Posttest | Pretest | 12.273 | 4.679 | 0.076 |
| Follow-up | 4.545* | 1.498 | 0.038 | |
| Follow-up | Pretest | 7.727 | 5.002 | 0.460 |
| Posttest | - 4.545* | 1.498 | 0.038 | |
| Control | ||||
| Pretest | Posttest | 1 | 2.078 | 1 |
| Follow-up | 3.917 | 2.009 | 0.232 | |
| Posttest | Pretest | - 1 | 2.078 | 1 |
| Follow-up | 2.917 | 1.549 | 0.259 | |
| Follow-up | Pretest | - 3.917 | 2.009 | 0.232 |
| Posttest | - 2.917 | 1.549 | 0.259 |
a The cases marked with an asterisk (*) indicate a significance level of less than 0.05. However, it should be noted that no significant difference was actually observed.
The trends of mean scores of QoL in three groups are portrayed in Figure 1.
4. Discussion
The study’s findings revealed that the mindfulness intervention had a comparatively greater impact on QoL. However, from a statistical standpoint, none of the interventions proved effective in enhancing QoL. Furthermore, there was no significant difference between mindfulness-based and cognitive rehabilitation methods in improving QoL.
According to statistics, stroke is responsible for 25% of morbidities that result in the inability to perform daily tasks and activities. Each day, stroke survivors become more aware of the reduced motor function and impaired communication that are caused by the condition. The recent changes to the body not only affect the individual’s mental image but also create a fear of disability and communication difficulties. The disability that has been created causes challenges in carrying out daily tasks, self-care, work, leisure activities, social interactions, and fulfilling one’s roles (25). In explaining the current findings regarding the effectiveness of MBSR on QoL, it can be stated that regular practice of mindfulness exercises leads to positive changes in certain psychological functions. These changes include stress reduction and emotional regulation, which in turn contribute to the development of self-management skills and adaptability in handling stressful situations. Additionally, practicing MBSR can enhance physical abilities and foster the capacity to approach problem-solving with flexibility (17).
According to Tisdale, mindfulness training teaches individuals how to alter habitual behaviors associated with the state of dominance by redirecting cognitive resources towards neutral objectives, such as breathing or experiencing the present moment. In conscious attention, information transmission shifts from defective cycles to focus on the current experience. Defective processing cycles become less accessible when attention is used in this manner. In other words, by emphasizing the thorough and neutral experience of life, MBSR aids in fostering a more steady and unresponsive approach to life, even in stressful circumstances. Furthermore, a non-reactive acceptance of the current situation has the potential to effectively facilitate a more positive assessment of the disease, enhanced coping abilities, and decreased stress levels. Practicing meditation regularly enables individuals to respond more calmly to their surroundings and the events that unfold throughout the day (26).
By practicing mindfulness, individuals can engage in a transformative experience that they have intentionally cultivated. This process facilitates the alignment and enhancement of their thoughts, mood, and overall QoL. Mindfulness necessitates the utilization of specific behavioral, cognitive, and metacognitive strategies to enhance the attention process. This, in turn, aids in the prevention of negative mood, negative thinking, and the inclination towards worrisome responses. As such, mindfulness facilitates the cultivation of a fresh perspective and the emergence of pleasant thoughts and emotions. Mindfulness can assist individuals in effectively managing stress and illness. This approach enhances the state of conscious mind in individuals and raises performance by reducing mental rumination and emotional avoidance while also increasing self-regulating behaviors (27). The physical health domain of QoL includes various factors such as daily life activities, dependence on drugs, energy levels, fatigue, mobility, pain levels, discomfort, sleep quality, rest, and the ability to work. The occurrence of a stroke leads to significant changes in these aspects. When a person experiences a stroke, they face limitations in all functions and require care. Their autonomy is diminished, and their ability to take care of themselves and feel confident is affected. Ultimately, this results in a decreased QoL (28).
This research demonstrates that the MBSR intervention positively impacts individuals’ QoL. By increasing people’s awareness of the present moment, MBSR exercises affect the cognitive system and information processing, thereby enhancing QoL (29). The present study bears some resemblance to the study conducted by Davazdah Emamy et al. (30). In their study, they examined the QoL of individuals across four domains: physical function, emotional well-being, pain, and general health. Although there was an improvement in these scores compared to the pretest stage, no significant difference was observed when compared to the scores of the control group. The inconsistency of the results of this study with previous studies may have been attributed to the study’s implementation during the peak of the COVID-19 outbreak, which likely impacted the patients’ QoL. It may also be attributed to the chronic nature of the disease and the physical complications and limitations it causes.
4.1. Conclusions
In general, it can be stated that mindfulness training results in an increase in behavioral responses associated with attention. Given that attention serves as the basis and initial stage for all cognitive activities, the involvement of stroke patients in mindfulness training programs can potentially enhance cognitive skills typically impacted by the disease. In other words, mindfulness exercises have an impact on the cognitive system. They can enhance the capacity and ability of the information processing system. These exercises can help prevent negative emotions, foster new positive perspectives, and ultimately improve one’s QoL by employing behavioral, cognitive, and metacognitive strategies. Regarding the efficacy of MBSR, it is suggested that this treatment procedure be used as a complementary therapy.