1. Context
The spread of the coronavirus disease 2019 (COVID-19) has driven states around the world to apply drastic measures to restrict the transmission of the virus in the community. Nevertheless, the disease evolved rapidly into an ongoing pandemic. Within the first 48 months of the pandemic, more than 6.9 million deaths from this infection have been reported worldwide (1). Unfortunately, these numbers continue to grow (albeit at a slower rate) despite the implementation of open vaccination programs in almost all countries. The outbreak of COVID-19 caused an onerous burden on the operation of health services and posed enormous challenges to health personnel with unprecedented intensity. In most cases, health professionals selflessly responded to the increased demands of health care, and their commitment was widely recognized by society. Nevertheless, the toll of the COVID-19 pandemic on the lives of health workers was devastating around the world (2).
Not surprisingly, health professionals constitute a high-risk group in a setting of high viral or microbial transmissibility (such as in the COVID-19 pandemic) because they are front-line caregivers for infected patients and contact numerous individuals in everyday practice (3). Those with advanced age and underlying comorbidities are at increased risk of mortality in case of infection with the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) (4). Many healthcare workers were infected with the pathogen, and several of them lost their lives in the first phases of the pandemic (5). Moreover, the COVID-19 crisis caused high rates of stress, anxiety, and depression among health workers (6, 7).
Countries have currently embraced ‘open-up’ strategies based on the populations’ vaccination coverage and natural immunity and because new variants seem to be causing fewer hospitalizations and deaths. Tolerant policies have allowed society to return to normal functioning; however, they carry the risk of prolonging the presence of SARS-CoV-2 within the community. Given the impossibility of a worldwide eradication of COVID-19 in the foreseeable future, global human coexistence with SARS-CoV-2 will probably continue to exist (8). Consequently, health professionals will continue to expose themselves to the harsh reality of the effort to manage the disease, at least for some time to come. Furthermore, the possibility of facing a similar pandemic in the future from zoonotic reservoirs and in association with environmental changes is not negligible (9).
Doctors and nurses constitute an essential component of health care, as their scientific and professional roles are inextricably related to health protection and promotion. Therefore, an effective response to any public health crisis depends largely on the proper fulfillment of caring duties by clinicians. Within a context of epidemic or pandemic intensity, medical and nursing practitioners have critical roles in the containment of the pathogen in the community, the prompt diagnosis of the disease, and the appropriate treatment of infected patients. In addition, they are obliged to maintain the delivery of ordinary emergency and routine health services. Their commitment to treat, despite the precarious circumstances, is mainly dictated by bioethics, which encourages them to disregard personal health risks and heavy workloads. Societal pressure on health workers due to the extraordinary demands for health care is also a factor of motivation.
However, the presence of a pandemic (or even an epidemic) creates some moral dilemmas and opposing perspectives. Two main views have been expressed. On the one hand, it has been suggested that health professionals should have the choice to opt out of the activities for the management of a communicable threat after weighing up their volition to participate and the potential personal risks. On the other hand, it has been supported that the devotion to the endeavor against an infectious disease should be unconditional as long as necessary precautions are applied to minimize the spread of the responsible pathogen. To address these issues, both the scientific community and policymakers need to demarcate the boundaries – if any exist – of the ethical and legal obligations deriving from healthcare duties during a public health crisis.
2. Evidence Acquisition
The present article examined the nature and scope of the medical and nursing professions and the societal impact of the COVID-19 pandemic, whereupon it investigated their interrelationship. In addition, this study analyzed the lessons that were learned from this public health emergency and proposed certain ethical positions for health services and clinicians in similar probable situations in the future. A narrative review is a comprehensive report on a specific subject, also containing analysis and critique (10). Due to its lack of methodological restrictions, this approach is appropriate for in-depth examination of a given matter, particularly in novel cases where existing evidence is insufficient (11). The targeted selection of the relevant literature can allow for a flexible strategy for presenting critical views on the topic of interest (12). Therefore, this article used a narrative approach to summarize the existing theory about the relationship between clinicians and society, elaborate on the consequences of a pandemic or epidemic on social cohesion and the operation of health systems, and speculate on possible future stances in similar conditions.
3. Results
3.1. The Nature and Scope of Medical and Nursing Professions
There is a strong moral bond between doctors and patients, as well as a diachronic tradition of doctors’ commitment to the benefit of the sick. The special nature of medical duties derives from certain distinct features of the medical profession. Doctors have unique technical and scientific skills to provide aid in individual and public health issues. Their expertise renders physicians absolutely necessary for the provision of health care. By virtue of their professional role, they are also morally obliged to deliver their services according to social demands, even in situations of public health crisis. In addition to the social and moral commitment, there are also legally binding terms that determine the occupational behavior of doctors. In cases of salaried employment, physicians must offer services in accordance with the terms of contract enforcement and the relevant legislation. In cases of self-employment, the delivery of care is governed by the regulations of the state and the responsible medical association.
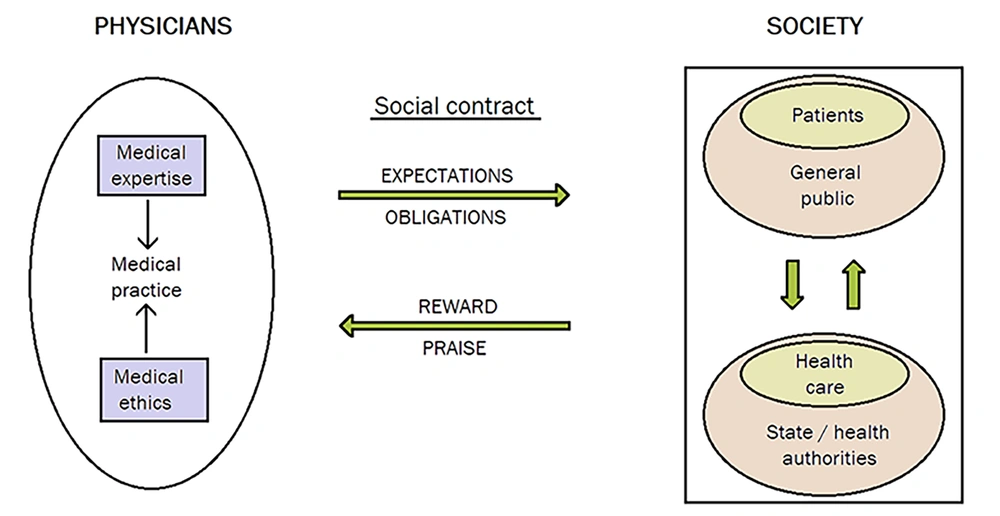
The special technical knowledge and skills of doctors, the ethical imperatives for health protection and promotion, and state laws and regulations constitute the factors that shape the medical professionalism through which physicians are put at the service of society (13). In parallel, the state and responsible health authorities regulate access to health care for citizens; nevertheless, the role of the public is to elect the government and, consequently, to approve (or disapprove) the relevant health policies (14). Both parties (physicians and society) enter into a social contract, according to which doctors offer services within predetermined acceptable standards of care, and society recompenses them with financial remunerations and moral accolades (15). Figure 1 is a schematic representation of the relationship between medical practitioners and society.
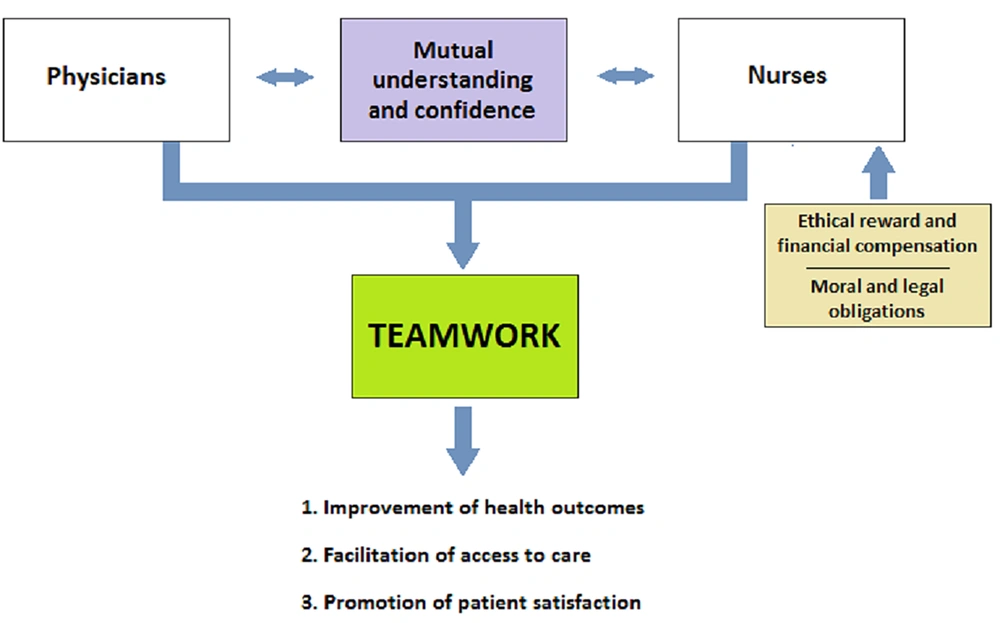
Similar (or even stronger) ethical and legal principles guide the work of nursing practitioners. Nurses serve the public with a moral obligation to cover the needs of all patients. Furthermore, legal standards are established by responsible authorities to maintain the integrity of the profession (16). The role of nurses enhances the full potential of health services to improve clinical outcomes and facilitate access to care. Interprofessional cooperation and teamwork between nurses and physicians are essential for improving the quality of health services and promoting patient satisfaction (17). The necessary compensation and recognition of the work of nursing practitioners are fundamental prerequisites for their contribution to health care. Figure 2 is a depiction of the contribution of nurses to clinical practice.
The distinction between working within the prescribed duties (both ordinary and extraordinary) and performing supererogatory actions is usually vague. After all, professionalism is principally based on personal commitments and sensitivities; however, institutional principles only provide general guidance. Clinicians are certainly expected to continue to offer their standard services during a public health crisis. Nonetheless, the willingness to deliver care or the potential of imposing such an obligation starts to fade in excessively precarious conditions. Practicing medicine and nursing during the outbreak of a morbid communicable disease unavoidably entails a probable serious danger to the health of those involved. The circumstances of a pandemic might mandate health professionals to work at the limits of their competencies and prompt a measurable and immediate risk of illness and death, working burnout, and psychological distress. For that reason, it is important to expect reciprocity to some extent from society toward health workers, as happened in the case of the COVID-19 pandemic (18).
3.2. The Societal Impact of the COVID-19 Pandemic
The COVID-19 infection spread rapidly around the world and radically affected every aspect of daily life. The pandemic inflicted a greatly adverse impact both on socioeconomic activities and on the provision of health care (19). Countries throughout the world imposed a series of protective measures to contain the dissemination of the pathogen, including lockdowns, confinement orders, border closures, trade restrictions, and travel limitations. In addition, the extended vaccination of the population was applied in most countries but at various rates of acceptance. Unfortunately, both the outbreak of COVID-19 and the associated preventive actions impinged on individuals, communities, markets, businesses, and organizations worldwide. The pandemic revealed the global interconnection of communities, where there is a chain reaction in the occurrence and diffusion of adverse effects.
The pandemic disrupted the operation of the primary (the extraction of natural resources and agriculture) and secondary (manufacturing, construction, and processing) sectors of the economy due to decelerations in the production and manufacturing of goods and delays in the transportation and distribution of commodities. Furthermore, a decline in the activities of the tertiary (services) economic sector occurred, especially within the fields of hospitality, transportation and tourism, real estate, education, financial services, and sports (20). The sharp downturn in the national and global economy decimated labor (both waged and self-employed) and consequently degraded livelihoods, thereby placing millions of individuals at risk of poverty. In addition, individuals encountered undue psychological stress and a serious threat to their mental well-being, deriving from the fear of getting sick or passing the virus to others, social isolation from peers and family members, and frustration due to the interruption of usual activities (21).
As effective vaccines and medications became widely available and less clinically severe SARS-CoV-2 variants emerged, most countries withdrew their restrictive policies. The goal was to ease the impact of lockdowns and quarantines on the economies of both communities and countries and on the well-being of individuals and populations. However, the profound adverse effects of COVID-19 will possibly last for many years, albeit to a progressively lesser gravity. Similar to most disasters, the pandemic exacerbated existing social inequalities. The precarity disproportionately affected disadvantaged groups, leaving large populations at greater risk for poor health. The recovery is expected to occur only after an intense and long-lasting effort (22).
The novel coronavirus outbreak generated extreme conditions for health care, especially during the outbreak waves (23). Under the circumstances of the pandemic, the urgent need to contain the disease and manage the infected patients sharply heightened the demands on health systems and facilities. The COVID-19 outbreak also adversely affected the capacity of health services to maintain the delivery of surgical (24) and routine care (25) due to the shift in priorities and the physical distancing recommendations. The heavy workload and the depletion of the available resources were critical threats to the resilience of health systems around the globe, with a resultant potential deterioration of public health at a national and international level. Although the strain on health systems due to the pandemic has been relieved for now, containing the spread of the virus and managing the clinical features of the infected patients while performing all the ordinary healthcare duties at the same time will continue to be essential and strenuous tasks. Therefore, the demand from health systems to operate swiftly and effectively remains; however, the pressure is gradually decreasing over time.
Since the onset of the pandemic, physicians and nurses have lain at the core of the challenges in health care. They are constantly encountering increased work demands in an uncontrollable occupational environment. Health workers are more likely to contract SARS-CoV-2 in comparison to the general population, most probably due to workplace exposure and physical proximity to patients. This susceptibility is still evident (although with lower relative risk) even when appropriate protective equipment is used (26). Moreover, the COVID-19 pandemic induced a destructive impact on health professionals' mental well-being due to the stressful situations occurring in their daily work (27, 28). After almost 4 years in the fight against the pandemic, the adverse effects on clinicians have become chronic and emphatically threaten the resilience of the health workforce.
3.3. Lessons Learned from the COVID-19 Crisis
In the exceptional times of a pandemic, health professionals are caught between their obligation to care for patients and their need to protect their own health. Both sides of this fragile balance put restrictions on each other, and the resultant equilibrium could subvert the social contract between clinicians and society. Any effort to solve this ‘Gordian knot’ must be based on the principles of bioethics and social justice. The management of the COVID-19 outbreak showed that the ideal goal would be to protect the provision of health care and the fiduciary relationship between health professionals and patients without posing intolerable risks to the health and professional integrity of the health personnel (29).
For this purpose, all parties involved (health authorities, associations, systems, services, unions, and professionals) can use the valuable experience gained from the COVID-19 crisis. Unambiguous and systematic guidelines are necessary to delineate the rights and responsibilities of medical and nursing practitioners. Ethical and administrative regulations issued by health organizations can assist caregivers in deciding the degree of appropriate involvement. Such strategies reorient moral challenges from a focus on the individual to a system-wide perspective (30). Special attention should be given to vulnerable subsets of professionals, such as those of older age or with underlying chronic conditions, who are probably more susceptible to complications from an infection.
However, the personal volition to serve in the various healthcare activities after assessing the respective risks should be a pivotal factor, especially in situations where absolute protection is not guaranteed (31). Opting out of frontline work by quitting the working position (in the case of salaried employment) or ceasing the delivery of services (in the case of self-employment) puts an additional burden on the rest of the health workforce and undermines patients' trust in clinical staff. Clinicians might only consider refraining from specific tasks (not the entire gamut of their duties) when there is an excessive danger of significant harm, and the relevant protective measures are disproportional (32).
In the course of the COVID-19 pandemic, shortages of health personnel frequently occurred due to the increased demands for health care and sick leaves or preventive quarantines. In such situations, physicians and nurses might be called upon to offer services outside the range of their specialty. The assignment of unfamiliar duties would be an unacceptable situation in standard care. Nonetheless, every licensed clinician has a basic clinical knowledge and ability to care for patients. With the depletion of human resources, it is reasonable to occasionally ask doctors and nurses to use their scientific competence outside the strict framework of their specialty in times of extreme need. This tactic necessarily presupposes the presence of adequate supervision by specialized colleagues (33).
The risk of contracting a pathogen (such as SARS-CoV-2) is a serious occupational hazard for health professionals. Therefore, reliable protective measures, such as personal protective equipment and organizational safety protocols, must be available in order to limit undue peril (34). A continuous assurance of adequate protection is a prerequisite for any obligation to treat. All caregivers must be thoroughly trained to comply with the implemented precautions. Regulatory authorities and employers should make increased efforts to establish sustainable working hours for the staff; therefore, adequate rest is secured. In addition, free-of-charge testing for the prevailing infection should be easily available for health workers, and open access to care in the event of contracting the pathogen must be secured. Furthermore, the provision of compensation in the form of life insurance or sickness benefits and allowances for hazardous working conditions could be strong incentives and an important recognition of clinicians’ work. Finally, potential legal repercussions need to be addressed (35).
3.4. Clinical Implications for the Future
States around the world have already transitioned from the acute phase of the COVID-19 pandemic to a chronic coexistence with the virus. However, SARS-CoV-2 will continue to be an occupational threat to health professionals in the foreseeable future. It is expected that COVID-19 will become endemic with repeated reinfections, seasonality in temperate zones, and regular upsurges in cases. Furthermore, the inevitable relaxation of control measures might facilitate the transmission of the pathogen (36). Heretofore, neither vaccination nor natural infection appears to be successful in achieving absolute long-term sterilizing immunity, especially against the new variants. Although it is assumed that each possible subsequent variant of SARS-CoV-2 will be less pathogenic and more transmissible than its predecessor, the occurrence of a more dangerous mutation cannot be totally excluded. Under these circumstances, the risk for health professionals in the post-acute stages of the pandemic will vary across time and region and, in some cases, will be significant. In addition, the risk of a pandemic from a new pathogen in the future possibly lurks and demands the alertness of authorities, systems, services, and professionals. The post-pandemic era can serve as an opportunity to prepare for the next potential threat, either from an infectious agent or from any other public health crisis (37).
It is an obvious assumption that both doctors and nurses expose themselves to some degree of inherent risk when treating patients. Nevertheless, some health workers might have reasonable reservations about their involvement in providing health care under the extraordinary circumstances of a pandemic. Their hesitation is primarily due to the serious personal risks posed by a possible infection. Their fear of contracting the pathogen and passing it on to their kin is an important inhibitory factor. Furthermore, some physicians might be reluctant or unable to manage the workload that inevitably emerges from the increased need for clinical care during a public health crisis. Their concerns might be exacerbated in cases where they are called upon to provide care outside the normal scope of their practice. The unease with unfamiliar duties aggravates the feeling of insecurity on the part of some doctors. Despite the existing difficulties and dangers, the responsibility of clinicians to treat patients remains imperishable.
The view that mandates doctors and nurses to remain active in a pandemic must be based on essential principles governing the medical and nursing professions. Due to the precarious conditions prevailing in a pandemic or epidemic, clinicians’ devotion to their duties extends beyond the narrow obligation to care for the sick. Firstly, clinical practice is implicitly connected with accepting the mission to offer services in times of emergency. Health systems have invested significant resources for this purpose. Therefore, society can reasonably rely on doctors and nurses to protect public health in the midst of an outbreak of a communicable disease. Secondly, health professions are characterized by highly specialized expertise, which is necessary for the provision of health care. Therefore, doctors and nurses are expected to be the primary actors in the effort to mitigate the burden on health systems, particularly in times of greatest need.
Advances in technology have fueled societal expectations from health care. The outbreak of an infectious disease can further overstretch the demands on health services and clinicians. However, the primacy of patient welfare is a core value of both medical and nursing professionalism, even in times of epidemic or pandemic. Therefore, health professionals ought to be well-trained to respond to conditions of urgency. Special seminars and training courses can be organized by responsible bodies for this purpose. In addition, health services must operate in such a way as to ensure greater coherence in the delivery of clinical care and to support health personnel in a safe and sustainable manner. Inevitably, this issue requires securing resources to be used for seasonal or permanent recruitment of personnel, an adequate supply of logistics and equipment, and the establishment of contingency plans.
4. Conclusions
The COVID-19 pandemic drastically reshaped the provision of health care; however, the priority of medical and nursing practitioners to protect individual and community health remained unaltered. Doctors and nurses are among the most important defenders of society in extraordinary moments of uncertainty, fear, and anxiety. The COVID-19 crisis proved that, in most cases, they selflessly use their scientific knowledge and technical skills to provide health care despite personal risks associated with exposure to pathogens, physical exhaustion, and emotional stress. However, health care in the era of a pandemic is more than fighting a disease. It also concerns the acknowledgment of the needs, experiences, and feelings of individuals in a vulnerable situation and the sustainability of an overburdened health system. Society is certainly obliged to applaud the work of those who make sacrifices to respond to the demands of a public health crisis. However, doctors and nurses must have the personal volition to participate in the fight against the novel coronavirus or any other future public health crisis, regardless of obligations, accolades, and incitements. The COVID-19 crisis was an appointment with history that taught us that every competent physician and nurse should be present in the fight against public health threats. Although the transmission of the novel coronavirus remains a global emergency, humanity will eventually overcome the crisis, just as it has defeated many infectious diseases in the past. Then, if our descendants ask every one of us what we did in the pandemic, we will be justified in answering: “What did I do? I was at the forefront, saving the world.”