1. Background
Cerebral palsy (CP) is the most prevalent neurological motor disability in children (1). The incidence rate of this condition, caused by non-progressive brain injuries during brain development, is estimated to be between 2 and 2.5 per 1000 live births. Cerebral palsy often entails sensory and cognitive deficits, communication and behavioral issues, and seizures (2). Children with cerebral palsy face significant limitations in daily activities such as bathing, eating, dressing, and social participation, necessitating long-term care (3). These difficulties, coupled with secondary musculoskeletal problems, negatively impact their quality of life (4). Quality of life (QOL) is defined as an individual’s perception of his/her well-being across various domains, including physical, social, emotional, and spiritual aspects of life (5). Research has identified several factors associated with lower QOL scores in children with CP, including being older than 6, having swallowing disorders, experiencing more intense chronic pain, and having higher levels of motor impairment (6). Among non-ambulatory children with CP, feelings of sadness, difficulties in understanding their parents, and not attending school were significant predictors of lower quality of life (7).
Clinical trials have shown that QOL can be improved through pharmacological treatments and motor control interventions (8). Studies reveal that individuals with disabilities encounter a wide range of attitudinal, physical, and systemic barriers when accessing healthcare. According to the World Health Survey report, individuals with disabilities are twice as likely to experience inadequacies in the skill sets of care facilities to meet their needs and are three times more likely to be overlooked by the healthcare system. Healthcare costs for individuals with disabilities are 50% higher than for those without disabilities, and covering healthcare needs is unaffordable for half of the people with disabilities (9). Provision of rehabilitation services early in life can enhance function and participation. Understanding utilization patterns of current health facilities can assist in providing more suitable services for people with disabilities (10) The Cerebral Palsy Quality of Life Questionnaire (CP QOL-Child) was the first tool specifically designed to assess the QOL of children and adolescents with CP based on the international classification of functioning, disability, and health (ICF) (11). The QOL of individuals receiving health services can indicate the effectiveness of medical and rehabilitation services in enhancing the physical, emotional, psychological, and social functions of patients. Moreover, achieving the highest levels of QOL is the ultimate goal of the healthcare system (12).
Access to information about the QOL of community members can aid in the allocation of evidence-based resources and the provision of appropriate services, which can improve various aspects of life (13, 14).
2. Objectives
It was unclear which aspects of the QOL of children with CP are related to access to rehabilitation centers, assistive devices, and home modifications. Consequently, this study was designed to explore the relationship between access to rehabilitation services and various aspects of QOL in children with CP in Saqqez County, Kurdistan province, Iran.
3. Methods
3.1. Study Design
This study was cross-sectional. To include all known children with CP in Saqqez County, we opted for consensus over sampling. Since children with disabilities are typically registered with the Welfare Organization to avail themselves of any available facilities, this organization was utilized to reach out to families of children with CP.
3.2. Participants
All 127 parents of children with CP aged 4 - 12 years registered with the Welfare Organization in Saqqez County were informed about the study and invited to participate. Of those invited, all except one agreed to participate, resulting in 126 parent-child with CP being enrolled in the study.
3.3. Scales
The Physical Rehabilitation Services Accessibility Questionnaire (10) and the parental proxy version of the CP QOL-Child (15) were employed as measurement tools.
3.3.1. Physical Rehabilitation Services Accessibility Questionnaire
The Physical Rehabilitation Services Accessibility Questionnaire is a Persian checklist comprising 17 items, with a 5-point Likert scale ranging from never = 0 to many times = 4. The items are organized into four factors: Affordability, transport, social support, and information access, as determined by factor analysis. The score for each factor and the total score are calculated by summing the item scores and can also be presented as a percentage. The face, content, construct validity, and reliability of the questionnaire have been established by Shirazikhah et al. The reported Cronbach’s alpha values for affordability, transport, social support, and information access were 0.86, 0.80, 0.79, and 0.79, respectively (16).
3.3.2. Quality of Life Questionnaire for Children with Cerebral Palsy (Parental Proxy Version CP QOL)
The Quality of Life Questionnaire for Children with CP (Parental Proxy Version CP QOL-Child) comprises 66 items that evaluate seven domains of quality of life in children aged 4 - 12 years with CP. These domains include participation and physical health, social well-being and acceptance, feelings about functioning, emotional well-being and self-esteem, access to services, pain and impact of disability, and family health. Completing the questionnaire by the child's family caregiver takes approximately 15 - 20 minutes. Domain scores range from 0 to 100, with higher scores indicating better quality of life in all domains except for the Pain domain, where higher scores indicate more pain. This scale does not calculate a total QOL score. Previous validations of this tool have checked its content validity, concurrent validity (correlation of domain scores with those of the kid-screen and CHQ), construct validity (convergent/divergent), internal reliability, and retest reliability (17). The Persian version of the questionnaire was utilized in this study (18).
It is important to note that the items in the "Physical Rehabilitation Services Accessibility Questionnaire" focus on access to rehabilitation services in clinics, assistive technologies at home, and home adaptations. However, it does not assess accessibility to in-home rehabilitation services, respite care, or special social facilities such as additional learning support in kindergarten, preschool settings, or community service facilities, which are inquired about in the Access to Services domain of the CP QOL-Child questionnaire.
3.4. Data Collection
The questionnaires were administered through face-to-face or phone interviews, depending on the participants' preferences.
3.5. Data Analysis
The Kolmogorov-Smirnov test indicated that the 'services accessibility' scores did not follow a normal distribution. Hence, a non-parametric test was utilized. The Spearman correlation coefficient was employed to identify the relationships between variables. Data analysis was conducted for the entire group as well as for each age subgroup: '4 to 6 years old (preschool children)' and '6 - 12 years old (primary school-aged children)'. The analysis was carried out using IBM SPSS version 23, and the significance level for tests was set at 0.05.
3.6. Ethical Considerations
The study received approval from the Ethics Committee of the University of Social Welfare and Rehabilitation Sciences (IR.USWR.REC.1399.035). Informed consent was obtained from all individual parents included in the study prior to the interviews.
4. Results
The study included a total of 126 children. The majority of the children were male (n = 75, 59.5%). The mean age and standard deviation were 8 ± 2.36 years. Approximately 21% of the children (n = 27) had only motor disabilities, while the others had additional issues, with speech and language deficits being the most common (n = 61, 48.4%). About 55% of school-aged children (6 - 12 years old) were attending school, but only one child aged 4 - 6 years was enrolled in kindergarten. Table 1 displays the mobility function of the children with CP in the study.
| Gross Motor Function Classification System (GMFCS) | Without Help (Levels I and II) | With a Little Help (Level III) | With Moderate Help (Level IV) | Totally Dependent to Others (Level V) |
|---|---|---|---|---|
| Age, y | ||||
| 4 - 6 | 9 (33.3) | 0 (0) | 12 (44.4) | 6 (22.3) |
| 6 - 12 | 36 (36.3) | 12 (12.1) | 24 (24.3) | 27 (27.3) |
a Values are expressed as No. (%).
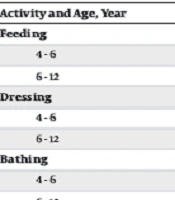
Table 1 indicates that 9 (33.3%) of the children aged 4 - 6 and 36 (36.3%) of the children aged 6 years and older were independent in their mobility function. Parents reported their children’s daily living activities. The results, presented in Table 2, show that 12 (44.4%) of the children aged 4 to less than 6 and 38 (38.4%) of the children aged 6 - 12 years with CP were independent in feeding. The rates of independence in dressing were 3 (11.2%) and 23 (23.2%), and in bathing, 1 (3.7%) and 19 (19.2%), respectively.
| Activity and Age (y) | Without Help | With a Little Help | With Moderate Help | Totally Dependent on Others |
|---|---|---|---|---|
| Feeding | ||||
| 4 - 6 | 12 (44.4) | 4 (14.8) | 3 (11.2) | 8 (29.6) |
| 6 - 12 | 38 (38.4) | 22 (22.3) | 6 (6) | 33 (33.3) |
| Dressing | ||||
| 4 - 6 | 3 (11.2) | 4 (14.8) | 4 (14.8) | 16 (59.2) |
| 6 - 12 | 23 (23.2) | 17 (17.1) | 14 (14.2) | 45 (45.5) |
| Bathing | ||||
| 4 - 6 | 1 (3.7) | 0 (0) | 5 (18.5) | 21 (77.8) |
| 6 - 12 | 19 (19.2) | 11 (11.2) | 6 (6) | 63 (63.6) |
a Values are expressed as No. (%).
The quality of life of children with CP aged 4 - 6 and 6 - 12 years is shown in Table 3.
| Domains | 4 - 6 Years Old | 6 - 12 Years Old | Total Group | P-Value b |
|---|---|---|---|---|
| Social wellbeing and acceptance | 73.79 ± 19.28 | 78.99 ± 15.68 | 77.87 ± 16.57 | 0.001 |
| Feeling about functioning | 62.84 ± 14.49 | 67.10 ± 18.87 | 66.19 ± 18.06 | 0.279 |
| Participation and physical health | 59.97 ± 17.03 | 65.91 ± 18.39 | 64.64 ± 18.21 | 0.037 |
| Emotional wellbeing and self-esteem | 68.90 ± 15.74 | 76.09 ± 15.93 | 74.50 ± 16.10 | 0.039 |
| Access to Services | 43.63 ± 24.18 | 44.90 ± 30.45 | 44.63 ± 29.14 | 0.427 |
| Pain c and impacts of disability | 50.53 ± 15.57 | 48.44 ± 20.17 | 48.89 ± 19.21 | 0.697 |
| Family Health | 67.01 ± 21.34 | 59.31 ± 25.57 | 60.96 ± 24.84 | 0.154 |
a Values are expressed as mean ± SD.
b P-value of independent groups t-test.
c In the domain of pain, lower scores mean better quality of life.
As depicted in Table 3, the QOL domain scores ranged from 44.63 ± 29.14 in the 'access to services' domain to 77.87 ± 16.57 in the 'Social well-being and acceptance' domain. According to the results of independent groups t-tests, the QOL domain scores of children aged 6 - 12 years were significantly higher than those of children aged 4 - 6 years in the domains of “Social wellbeing & acceptance” (78.99 ± 15.68 vs. 73.79 ± 15.68; P < 0.001), “Participation & physical health” (59.97 ± 17.03 vs. 64.64 ± 18.21), and “Emotional wellbeing & self-esteem” (76.09 ± 15.93 vs. 68.90 ± 15.74; P = 0.039).
No relationship was found between the children's age group and access to rehabilitation services. The scores for access to rehabilitation services in the entire group are summarized in Table 4.
| Accessibility Factors | Total Group b |
|---|---|
| Affordability | 58.13 ± 27.39 |
| Transport | 62.90 ± 30.29 |
| Social support | 60.65 ± 29.90 |
| Information access | 26.72 ± 24.95 |
| Total accessibility | 53.87 ± 22.08 |
a Range of scores in each domain was 0 – 100.
b Values are expressed as mean ± SD.
Table 4, according to parental reports, shows that access to information was lower than other types (26.72 ± 24.95) of access, with scores ranging from 58.13 to 62.90 on a 0 - 100 scale.
Table 5 outlines the relationships between access to rehabilitation services and quality-of-life domain scores of children with CP. Since the CP QOL-Child scores were not normally distributed among the groups, Spearman correlation coefficients were calculated.
| Correlation | Total Score of Having Access to Rehabilitation Services | |||||
|---|---|---|---|---|---|---|
| Domain of Quality of Life | 4 - 6 Years | 6 - 12 Years | Total | |||
| r | P | r | P | r | P | |
| Social wellbeing and acceptance | -0.01 | 0.605 | 0.18 | 0.074 | 0.12 | 0.18 |
| Feeling about functioning | 0.02 | 0.885 | 0.28 | 0.004 a | 0.23 | 0.013 a |
| Participation and physical health | -0.21 | 0.278 | 0.21 | 0.042 a | 0.11 | 0.19 |
| Emotional wellbeing and self-esteem | -0.26 | 0.186 | 0.22 | 0.023 a | 0.12 | 0.16 |
| Access to services | -0.23 | 0.241 | 0.36 | < 0.001 a | 0.30 | 0.003 a |
| Pain and impact of disability | -0.34 | 0.075 | -0.25 | 0.010 a | -0.27 | 0.002 a |
| Family health | 0.44 | 0.021 a | 0.46 | < 0.001 a | 0.46 | < 0.001 a |
a P < 0.05, Spearman correlation coefficient.
Table 5 reveals that among children aged 6 - 12, access to rehabilitation services had a significant correlation with all CP QOL-Child domain scores except for 'social wellbeing and acceptance'. However, for children aged 4 - 6 years, only the family health domain score showed a correlation with access to rehabilitation services. In the entire group of children aged 4 - 12 years, the highest correlation coefficient was between access to services and the family health domain of the CP QOL-Child (r = 0.46, P < 0.001).
5. Discussion
The relationships between different domains of 'quality of life of children with CP' and 'access to services' were not the same. Additionally, the relationship between these variables were not similar in children aged 4 - 6 (preschool aged children) and those aged 6 - 12 years (school aged children).
The 'family health' domain of the CP QOL-Child was related to 'access to rehabilitation services' across both age groups. Conversely, the 'acceptance and social welfare' domain did not correlate with 'access to rehabilitation services' in any of the aforementioned age groups. The relationships between other domains of the CP QOL-Child and 'access to rehabilitation services' were significant only among school-aged children. Several reasons might explain these discrepancies:
The absence of a correlation between 'access to services' and the 'social wellbeing and acceptance' domain could stem from the nature of the services inquired about, which included rehabilitation centers, health, medical and surgical interventions, assistive technologies, and home modifications. None of these services include social skills training or address the social environments of the children. This finding aligns with the results of the study examining the relationship between environmental barriers and quality of life of school-aged children with CP (8 - 12 years) in Tehran, which found that only the 'family health' and 'access to services' domains of CP QOL-Child were related to environmental barriers. In the current study, CP QOL-Child scores in the 'social wellbeing and acceptance' domain (77.87 ± 16.57) were higher than all other domain scores. This score was also higher than those reported in Tehran, the capital city of Iran (72.62 ± 15.13) (19), Delhi, India (57.66 ± 11.5) (20), and Dhaka, Bangladesh (67.4 ± 8.4) (21), and was close to the scores recorded in Melbourne, Australia (78.09 ± 12.18) (22) and less than reported score for Finland (81.9 ± 11.5).
The differences observed between the two age groups in other domains could be attributed to parents' greater difficulty in recognizing emotions in preschool children compared to older ones. Previous studies have indicated that mothers of preschool-aged children require more information to accurately identify emotions in children's facial expressions (23). Additionally, some questionnaire items related to functions and participation might not be expected by parents of younger children to be achievable. Moreover, half of the children aged 6 - 12 years were attending school, allowing parents to more precisely evaluate their children’s QOL as these children had opportunities to interact with peers or participate in age-appropriate activities within the school environment.
The mean score for the pain and impact of disability domain of QOL for children with CP was 48.89. This score was higher than that reported for children with CP in Melbourne, Australia (33.18) but lower than in Dhaka, Bangladesh (53.0), and Finland (64.8). The gap between parental expectations and experiences could play a significant role in their judgments and scores. Higher expectations and concerns of parents regarding their children with CP might lead them to report higher scores of pain and impact. Conversely, the life standards of children without CP in each community could also influence parents' judgments about the pain and impacts of CP on their children's QOL; as the perception of QOL is related to individuals' concerns, expectations, and standards, as mentioned in the World Health Organization’s definition of QOL (24).
The relationship between access to rehabilitation services and the QOL of children with CP had not been previously studied in Iran. However, using the quality of life questionnaire for the blind, Sarabandi et al. found that there was a relationship between the utilization of rehabilitation services and the QOL of individuals with blindness, aged seven years or older, in Zahedan County, Iran (25).
A previous study on barriers to attending rehabilitation sessions in Birjand city, Iran, revealed that the 'high cost of rehabilitation services,' long distance between home and rehabilitation clinics,' 'difficulties in transporting the child,' 'poor weather conditions in some seasons,' and 'lack of time' were the most prevalent barriers to regular attendance at rehabilitation sessionss, as mentioned by parents. However, only the correlation between 'morning-only opening hours of rehabilitation clinics' and regular attendance was found to be statistically significant (26).
In this study, access to information (26.72 ± 24.95) was reported to be much lower than other domains of service accessibility. Part of this observed difference might be related to the wording of the questionnaire items. Questions about 'accessibility to information' solely inquired about the frequency of parents accessing the information they needed without asking if low access to information was a barrier to accessing rehabilitation services. In contrast, other items in the questionnaire addressed this point as well. Similar findings were reported in studies on children with Autism in Iran and Canada, where families of children with autism spectrum disorders also faced difficulties in accessing information about their children's condition (27).
The limitations of this study are as follows: Only the parental-proxy version of the CP QOL-Child Questionnaire was used to assess the children's quality of life because a significant number of children were unable to answer questions themselves. Parents' perceptions of their children's quality of life and feelings may not fully align with the children's own perspectives. Studies have shown that parents tend to rate their children’s physical quality of life lower than the children themselves report (28).
Furthermore, accurately judging the feelings of younger children, especially when their ability to communicate is impacted by CP, can be challenging. The age range of 4 - 12 years was chosen due to the limitations of the tool. Therefore, generalizing the results of this study to other age groups should be done with caution.
5.1. Conclusions
Overall, the quality of life of school-aged children with CP was related to access to rehabilitation services, with the exception of the social well-being and acceptance domain. Interventional studies could clarify the effects of improvements in different aspects of accessibility on the quality of life for this group of children. The results of this study suggest that, in children under six years of age, only the family health domain of the CP QOL-Child is likely to be sensitive to changes in access to rehabilitation services. Although the scores for the social well-being domain were relatively better than those for other domains of quality of life, interventions that directly focus on the social well-being of children, in addition to current rehabilitation services, might aid in further improvements in this area.