1. Background
Maternal care is an essential goal of healthcare systems worldwide and has been the focus of several studies (1, 2). Recent research has concentrated on improving maternal outcomes via enhanced recovery pathways (3). One of the influential factors in this regard is the mode of delivery (4). Cesarean section (CS), which was advised against due to its alarming complications, including mortality, over a century ago, is now the most common surgery in obstetrics. It is performed for one in three women in the US and four in five women in some other countries (5, 6). Our country is no exception to this challenge (7). Although CS is commonly performed, it is always prone to potential complications. Moreover, the relative risk of complications is much higher in emergency situations (8) or when maternal co-morbidities such as hypertensive disorders (9), gestational diabetes (10), anemia (11), thyroid diseases (12), and cardiovascular diseases (13) are present. Medical co-morbidities are increasingly prevalent in pregnancy and are associated with adverse outcomes (14).
Studies have investigated the relationship between maternal co-morbidities and outcomes. However, considering the variety of influential factors in this regard, including differences in maternal socio-economic status and the level of provided care, their findings cannot be generalized. Therefore, each hospital should be aware of the health status of admitted pregnant women and how they are managed. According to available data from other studies, comparing the achieved results could be a significant indicator of each center's quality performance. A search of the literature revealed no similar study in our province. Considering that Alzahra Hospital is the only referral academic center for all types of obstetric and gynecological surgeries, including both elective and emergency situations, it is worthwhile to investigate this issue in this center.
2. Objectives
This study aimed to evaluate the relationship between maternal co-morbidities and adverse outcomes of cesarean sections.
3. Methods
3.1. Study Design
After obtaining the approval of the Ethics Committee of GUMS, this retrospective study was conducted at Al-Zahra Hospital in Rasht, Iran. This referral and academic center, affiliated with GUMS in the north of Iran, specializes in all emergency and elective types of obstetric and gynecological surgeries. After collecting the primary data, the relationship between maternal co-morbidities, their number, cesarean section outcomes, and the first-minute Apgar score were investigated.
3.2. Participants
The medical documents of all pregnant mothers who underwent cesarean sections during 2023 were sorted from the hospital registry system.
3.3. Sample Size
The minimum sample size, considering the 20% frequency of high-risk pregnancies based on research, a 95% confidence limit, and accepting a 5% margin of error, was determined to be 246 people.
3.4. Scales
To analyze the data for normal distribution, a two independent t-test was used; otherwise, the equivalent non-parametric test was applied. A P-value of less than 0.05 was considered significant.
3.5. Data Collection
The desired information included pregnant women's demographic data, maternal co-morbidities (such as hypertensive disorders, gestational diabetes mellitus, anemia, thyroid disorders, and cardiac diseases), and cesarean outcomes, which were defined as mortality or complications including postoperative ICU admission due to maternal hemodynamic instability, excessive bleeding during the operation, and respiratory problems. The first-minute neonate’s Apgar score was also recorded.
3.6. Data Analysis
The obtained data were analyzed using the Statistical Package for Social Sciences (SPSS), version 21.
3.7. Ethical Consideration
The study protocol was approved by the Research Ethics Committee of Guilan University of Medical Sciences (IR.GUMS.REC.1402.164), and all patients' data were anonymized prior to analysis.
4. Results
A total of 246 cesarean section cases were investigated, with an average maternal age of 31.59 ± 5.72 years (range 17 - 45). Most of them (72%) were in the age range of 20 - 35 years. The most common gestational age was 37 - 42 weeks (68.7%), and 61.8% were urban residents (Table 1).
| Variables | No. (%) |
|---|---|
| Age (y) | |
| ≤ 19 | 3 (1.2) |
| 20 - 35 | 177 (72) |
| ≥ 35 | 66 (26.8) |
| Gestational age (w) | |
| ≤ 37 | 77 (31.3) |
| 37 - 42 | 169 (68.7) |
| Gravidity | |
| 1 | 88 (35.8) |
| 2 | 73 (29.7) |
| 3 | 45 (18.3) |
| > 3 | 40 (16.3) |
| Residency | |
| Urban | 152 (61.8) |
| Rural | 94 (38.2) |
Maternal Demographic Data
Among the maternal co-morbidities, gestational diabetes mellitus (36.2%) was the most common, followed by hypertensive disorders (28.5%), hypothyroidism (21.1%), anemia (12.2%), and one case of cardiac disease (moderate mitral and tricuspid valve regurgitation). More than 90% of neonates had an Apgar score of 7 - 10. Regarding the relationship between maternal co-morbidities and unwanted outcomes, no statistically significant association was found except for hypertensive disorders (P = 0.003) (Table 2). Furthermore, maternal co-morbidities had no significant effect on the recorded Apgar scores (Table 3). No cases of mortality were reported. In terms of the relationship between the number of maternal co-morbidities and outcomes, no significant association was found (Table 4).
| Co-morbidity | Complications (+) | Complications (-) | P-Value b |
|---|---|---|---|
| Gestational diabetes mellitus | 0.726 | ||
| Yes | 4 (3.3) | 85 (85.7) | |
| No | 5 (3.2) | 152 (96.8) | |
| Hypertensive disorders | 0.003 | ||
| Yes | 7 (10) | 63 (90) | |
| No | 2 (1.1) | 174 (98.9) | |
| Cardiac disease | 1 | ||
| Yes | 0 (0) | 1 (100) | |
| No | 9 (3.7) | 236 (96.3) | |
| Hypothyroidism | 0.689 | ||
| Yes | 1 (1.9) | 51 (98.1) | |
| No | 8 (4.1) | 186(95.9) | |
| Anemia | 0.302 | ||
| Yes | 2 (6.7) | 28 (93.3) | |
| No | 7 (3.2) | 209 (96.8) |
The Association of Caesarean Section Outcomes According with Maternal Co-morbidities a
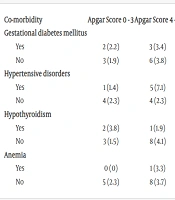
| Co-morbidity | Apgar Score 0 - 3 | Apgar Score 4 - 6 | Apgar Score 7 - 10 | P-Value b |
|---|---|---|---|---|
| Gestational diabetes mellitus | 1 | |||
| Yes | 2 (2.2) | 3 (3.4) | 84 (94.4) | |
| No | 3 (1.9) | 6 (3.8) | 148 (94.3) | |
| Hypertensive disorders | 0.183 | |||
| Yes | 1 (1.4) | 5 (7.1) | 64 (91.4) | |
| No | 4 (2.3) | 4 (2.3) | 168 (95.5) | |
| Hypothyroidism | 0.428 | |||
| Yes | 2 (3.8) | 1 (1.9) | 49 (94.2) | |
| No | 3 (1.5) | 8 (4.1) | 183 (94.3) | |
| Anemia | 1 | |||
| Yes | 0 (0) | 1 (3.3) | 29 (96.7) | |
| No | 5 (2.3) | 8 (3.7) | 203 (94) |
The Association of Apgar Score with Maternal Co-morbidities a
| Risk Factor Status | Complications (+) | Complications (-) | P-Value b |
|---|---|---|---|
| No | 1 (1.3) | 74 (98.7) | 0.277 |
| One | 4 (3.5) | 110 (96.5) | |
| Two | 4 (7) | 53 (93) |
The Association of Caesarean Section Outcomes with the Number of Maternal Co-morbidities a
5. Discussion
No statistically significant relationship was found between maternal co-morbidities, including thyroid problems, anemia, diabetes, and heart diseases, and cesarean section outcomes, except for hypertensive disorders. Additionally, no significant relationship was found between the number of diseases and complications. These findings indicate appropriate interaction between the obstetrics and anesthesiology teams. This suggests that, in addition to proper prenatal care, cesarean sections were scheduled following pre-operative anesthesia visits and necessary consultations, ensuring the procedures were performed timely and under ideal conditions. Gestational diabetes, defined as glucose intolerance first diagnosed during pregnancy, is the most prevalent endocrine disorder in pregnancy and is influenced by various underlying factors (15, 16).
In line with the literature, gestational diabetes was reported as the most common co-morbidity in this study. Studies have demonstrated that diabetes is an important risk factor for cesarean section. In pregnant women with gestational diabetes mellitus, compared to non-diabetic women, the overall cesarean section rate was reported to be 1.52 times higher (17). In a racially low-risk population, the prevalence of diabetes during pregnancy has been reported as 2 - 5% (18). Contrary to Basirat et al.'s 2010 research, which showed that gestational diabetes was associated with adverse outcomes, our study did not find it to lead to serious complications, indicating proper prenatal care and timely consultations (19). Hypertensive disorders were the second most common co-morbidity, with the highest percentage related to first pregnancies. This may be due to complications such as severe headaches and visual impairments requiring various medical interventions and, in some cases, ICU transfer. Overall, these complications could make pregnancy a difficult experience, potentially discouraging plans for subsequent pregnancies. Meng et al.'s 2023 study found that patients with preeclampsia had a higher rate of maternal cardiovascular complications (20).
In contrast to our study, Eslamimoghadam et al.'s 2018 study showed that gestational diabetes mellitus was associated with poor maternal and neonatal outcomes, with mothers experiencing early readmission and neonates showing more malformations. However, similar to our findings, gestational diabetes mellitus was the most common co-morbidity (21).
Faraji 2022 study evaluated the effect of high serum Inhibin-A levels in the first and second trimesters on adverse pregnancy outcomes. They concluded that high serum Inhibin-A levels increase the odds of preeclampsia, preterm birth, fetal growth retardation, and low birth weight (22).
One of the most important findings of this study was the management of critical cardiac cases in the absence of a general hospital. During the study period, only one case with a mild cardiac problem underwent cesarean section at Al-Zahra Hospital. However, more than ten severe cardiac cases were transferred to the main specialized heart surgery center of the province, benefiting from specialized services including CCU care and cardiac anesthesiologists, and all survived. Although cardiovascular disease is a well-known risk factor for maternal mortality, no mortality occurred in this process. This study revealed that despite limited facilities, proper communication and cooperation can be effective. Considering the lack of CCU wards and specialized cardiac services in many public academic hospitals in our country, this study provides an easy, affordable, and accessible guide for maternal health. Transferring the mother to the private sector or performing cesarean sections without the required equipment are not ethically or legally acceptable options.
In this study, no significant association was found between maternal co-morbidities and Apgar scores. More than 90% of the babies were born with an Apgar score of 7 - 10, indicating accurate fetal monitoring, timely cesarean sections, and appropriate anesthesia techniques. Since this center is an academic and referral hospital, it is crucial to minimize the number of deliveries with low Apgar scores. The results of this study contrast with Knosgaard et al.'s 2023 study, which showed higher cesarean section outcome frequencies in mothers with hypothyroidism (23). It also contrasts with Chu et al.'s 2020 study, which reported that maternal anemia was associated with adverse outcomes (24). In line with the current study, Ramos Filho and Antunes's 2020 study showed that hypertensive disorders were associated with a higher proportion of cesarean section complications but not related to Apgar scores (9).
The differences in study results across centers can be attributed to variations in research methods and populations studied. For example, a retrospective study in a center with an inadequate data recording system will yield different quality findings compared to a prospective study with close supervision. The commitment to accurately recording and reporting medical errors and documentation also varies. Additionally, the characteristics of each hospital—whether general or specialized, academic or private—along with the experience of the treatment team and the available equipment, can affect cesarean section outcomes. Socio-economic status differences among studied populations and the quality of communication between obstetricians and anesthesiologists at each center also play crucial roles in delivery outcomes. Some aspects are specific to each region and cannot be generalized.
Given the importance of maternal and newborn health, it is recommended to conduct this research prospectively to obtain more complete and reliable results by examining additional risk factors. Due to the nature of a retrospective study, the investigated co-morbidities were limited to those recorded in the files. Other risk factors, such as high BMI or maternal addiction, were not assessed. Given the importance of the issue, a well-planned prospective study is strongly suggested.
5.1. Conclusions
It was concluded that despite a notable number of maternal co-morbidities and risk factors, no significant adverse outcomes were reported. This indicates appropriate interaction between the obstetrics and anesthesiology teams, as well as standard and careful maternal and fetal monitoring in this center. Special attention should be paid to the treatment and care of maternal hypertensive disorders. Another valuable finding was the successful teamwork in managing severe cardiac cases, with no mortality or morbidity among them. Despite the acceptable results, as this hospital is an academic and referral center, efforts should be made to minimize complicated cases and restrict them to super-emergency situations that do not allow enough time for evaluation. This study strongly emphasizes the importance of teamwork and appropriate participation of different specialized fields.