1. Background
Cardiopulmonary resuscitation (CPR) is the initial response to a patient experiencing cardiopulmonary arrest (a sudden cessation of breathing and blood circulation). When performed correctly, it can reduce mortality rates by up to 50% (1). Chest compression (CC) at a rate of at least 100 beats per minute is a critical component of CPR that helps maintain blood circulation to vital organs, including the brain (2).
The outcome of resuscitation efforts is heavily influenced by the rescuers' skill level (3). Despite its inclusion in the early stages of nursing education, the scientific and practical knowledge of nursing students in CPR remains inadequate (4). In Iran, fewer than 10% of CCU nurses have sufficient knowledge of CPR (5). Evaluating learners' performance using various methods is essential to ensure they acquire the necessary CPR skills (6). Audio-visual feedback devices have been developed to improve the quality of CC and enhance CPR outcomes (7). Previous studies have demonstrated that using visual-auditory feedback and pressure sensors effectively improves CC depth and overall CPR quality (8, 9). There are two types of CPR feedback devices: Those that provide corrective actions for the resuscitator and those that merely announce the resuscitator's errors visually or audibly without suggesting corrective measures (10).
Nurses are the first responders in approximately half of all in-hospital cardiopulmonary arrests. As such, they must possess the requisite knowledge and skills to perform CPR and stay updated on the latest techniques (11). Additionally, Iran, as the 17th most populous country globally (12), requires a population with proficiency in performing quality CPR. However, no study has compared the effects of different feedback methods on CPR performance among health workers in Iran. Notably, in Iran, the one-hour survival rate after cardiac arrest was reported at 10.6%, with a hospital discharge survival rate of only 0.4% following in-hospital CPR (13).
2. Objectives
This study aimed to compare visual, direct, and combined feedback in improving the quality of CC among nurses.
3. Methods
3.1. Design Study
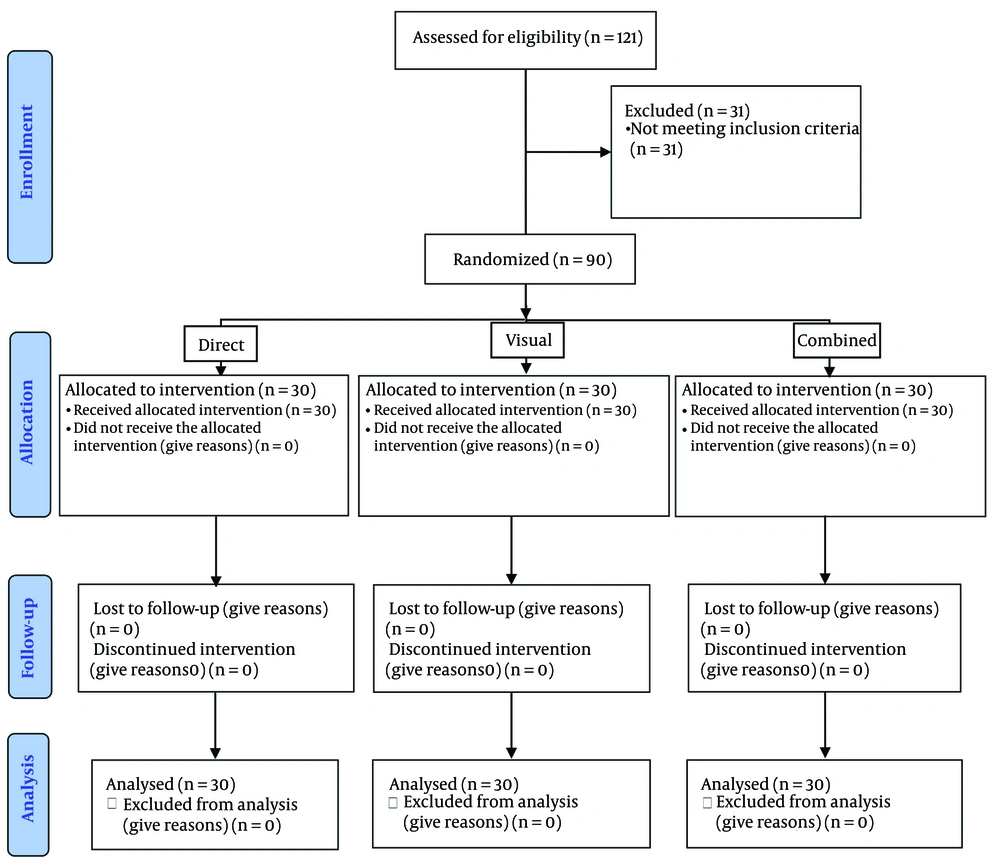
This field trial study was conducted in accordance with the CONSORT checklist (Figure 1).
3.2. Participants
All nurses from CCU, ICU, emergency departments, and the personnel involved in 99 resuscitation codes (essential personnel in resuscitation) in Birjand hospitals were eligible to participate in this study. Based on the study by Sadeghzadeh et al. (14) (µ1 = 2.72, µ2 = 3.02, S1 = 0.958, and S2 = 0.674) and with a significance level of 0.05 and a power of 90%, the minimum sample size was calculated as 30 nurses per group using the formula for comparing two means.
After extracting the names of the nurses from the management system, the desired nurses were randomly selected using a table of random numbers generated by the computer (site: https://www.random.org).
Nurses working in CCU, ICU, emergency departments, and personnel involved in 99 resuscitation codes, with at least one year of clinical experience, were included in the study if they worked a 7-hour daily shift, had no musculoskeletal problems, and provided consent to participate. Nurses on sick or maternity leave within the last six months and those who did not complete the study plan were excluded.
The selected nurses were randomly assigned to one of three study groups using a randomized block method to ensure balanced sample allocation. Fifteen blocks of six participants were created with random combinations of the letters A (direct feedback), B (visual feedback), and C (combined feedback) in different sequences. At each stage, a block was randomly chosen using the table of random numbers, and participants were assigned to one of the three groups based on the selected block. This process was repeated until the required sample size was achieved.
3.3. Scales
Data was collected using a two-part checklist that included demographic information and the quality of CC. The demographic section included sex, age, work experience, number of previous resuscitation workshops attended, number of previous patient resuscitations, education level, and workplace department. The quality of CC was recorded using the adult CPR and AED skills testing checklist, which assigns scores from 0 to 100 for each of its components (compression rate, depth, release, and time) and for the total score.
To evaluate CC quality, the Philips QCPR™ CPRmeter and CPR manikin instruments were used. The QCPR™ CPRmeter employs Laerdal's QCPR technology to measure CPR quality, providing real-time feedback on compression rate, depth, release, and action time. These parameters represent critical components of high-quality CPR as defined by the American Heart Association and are reported as percentages. In this CPRmeter (Q-CPR) device, only the correct measurements within the standard range are indicated; values outside the normal range (e.g., excessive or insufficient depth, incorrect rate, incomplete chest recoil, or pauses in compressions) are not separately detailed. For instance, if the device reports a depth score of 5%, it indicates that only 5% of the CCs met the normal depth range, while the remaining 95% were either too shallow or too deep.
In this study, the reported values were treated as absolute numbers without explicitly noting percentages. For example, a value of 82 indicates that 82% of the CCs were correct. The means include decimal points due to the consideration of four variables.
3.4. Data Collection
After explaining the research objectives and obtaining written consent, the pre-test was conducted using the QCPR™ CPRmeter and CPR manikin instruments.
In all study groups, under the supervision of a member of the medical emergency department, participants performed CPR for 2 minutes on the simulator using the Q-CPR, with an emphasis on CC.
In the direct feedback group, the professor identified and explained the problems or potential issues observed during the participants' CC performance and demonstrated the correct technique for performing CC.
In the visual feedback group, after completing the CC session, the professor provided explanations about the device and demonstrated how to interpret and use its feedback to improve performance.
In the combined feedback group, both direct and visual feedback were utilized. After the CC session, the professor explained the participants' problems and demonstrated proper CC technique. In addition, participants used the visual messages from the device to further refine the quality of their CC.
For all three groups, the sessions were conducted individually, without the presence of other participants. Each participant completed the CC session with feedback and underwent re-testing within the same session. The training duration for all groups was standardized at 3 hours, with each nurse's active practice lasting approximately 2 hours.
Two months after the intervention, participants were called back, and their CC quality was re-assessed using the Q-CPR.
3.5. Data Analysis
Data were analyzed using SPSS version 19 and described using numbers, percentages, means, and standard deviations. The normality of the data was assessed using the Kolmogorov-Smirnov test. Data analysis included one-way ANOVA, one-way repeated measures ANOVA, paired samples t-test, and chi-square test, with a significance level set at 0.05. The assumptions for one-way repeated measures ANOVA were evaluated using the sphericity test.
3.6. Ethical Consideration
This study was approved by Birjand University of Medical Sciences Ethics Committee (IR.BUMS.REC.1398.308) and complied with the Declaration of Helsinki; informed consent has been obtained from the subjects. The study purpose and importance were explained to participants, who met the inclusion criteria, and they signed the written informed consent form.
4. Results
The mean age of participants in the direct feedback group was 34.26 ± 5.4 years, in the visual feedback group was 35.0 ± 6.4 years, and in the combined feedback group was 36.1 ± 6.5 years, with no statistically significant difference (P = 0.488). Regarding other baseline characteristics, no significant differences were observed between the three study groups (Table 1).
| Groups | Patient Resuscitation Experiences | Work Experience | Participation in CPR Workshop | Age (y) | Education Level | |
|---|---|---|---|---|---|---|
| Bachelor's Degree | Master's Degree | |||||
| Direct feedback | 10 ± 31 | 5.5 ± 9.47 | 4.17 ± 2.2 | 34.26 ± 5.4 | 28 (93) | 2 (7) |
| Visual feedback | 11 ± 32 | 6.2 ± 9.43 | 3.77 ± 2.3 | 35.0 ± 6.4 | 26 (87) | 4 (13) |
| Combined feedback | 11 ± 30 | 11.7 ± 6.5 | 4.7 ± 2.3 | 36.1 ± 6.5 | 26 (87) | 4 (13) |
| P-value | 0.896 b | 0.249 b | 0.718 b | 0.488 b | 0.763 c | |
Comparison of Basic Characteristics in Study Groups a
There was no significant difference in the mean quality score of CC among the nurses in the three groups before the intervention (P < 0.05). Immediately after the intervention, the average quality score of CC increased in all three study groups, with the combined feedback group showing the highest increase (P < 0.0001). Two months later, compared to immediately after the intervention, the average quality score of CC decreased in all three groups, with the combined feedback group showing the smallest decrease (P < 0.0001). In all three groups, the average score of CC remained significantly higher than before the intervention (P < 0.05) (Table 2).
| Measuring Time | Direct Feedback | Visual Feedback | Combined Feedback | P-Value b |
|---|---|---|---|---|
| Before intervention (0) | 31.05 ± 15.35 | 30.56 ± 13.04 | 31.12 ± 17.02 | 0.98 |
| After intervention (1) | 74.45 ± 8.17 | 85.14 ± 5.15 | 96.57 ± 6.32 | < 0.0001 |
| Two months after intervention (2) | 66.29 ± 8.40 | 78.13 ± 6.18 | 91.26 ± 7.29 | < 0.0001 |
| P-value c | < 0.0001 | < 0.0001 | < 0.0001 | - |
| Average change times 0 and 1 | 43.30 ± 13.5 | 54.6 ± 13.1 | 64.6 ± 16.2 | - |
| P-value d | < 0.001 | < 0.001 | < 0.001 | - |
| Average change times 0 and 2 | 35.2 ± 13.8 | 47.6 ± 13 | 60.1 ± 15.7 | - |
| P-value d | < 0.001 | < 0.001 | < 0.001 | - |
| Average change times 1 and 2 | -8.16 ± 3.6 | -7.0 ± 3.8 | -4.4 ± 2.5 | - |
| P-value d | < 0.001 | < 0.001 | < 0.001 | - |
Comparison of the Mean Quality Scores of Chest Compressions in the Three Studied Groups Before, Immediately After and Two Months After the Intervention a
The average score changes over time among the three study groups showed a statistically significant difference (P < 0.001), and this difference was significant at all time points between the three groups according to Tukey's test (P < 0.001) (Table 2).
5. Discussion
The results of this study demonstrated that the quality of CC in nurses across all three investigated groups significantly improved immediately after the intervention and remained improved two months later. Nurses who received visual and combined feedback achieved greater improvements and maintained better stability in performance. The distinctive features of this study include the comparison of three types of feedback (visual, direct, and combined), the use of the Q-CPR device, and the assessment of long-term intervention effects.
According to Aghajani et al., basic CPR training with video feedback positively impacts nursing students' performance. In their study, the target group (non-professional lifeguards) and the type of intervention (video feedback) differed from the present study (5). Similarly, Wutzler et al. found that visual-auditory feedback devices play a significant role in resuscitating CC and enhancing its quality (15). Their study involved nurses but only used audiovisual feedback. Bobrow et al.'s study revealed that scenario-based CPR training for out-of-hospital cardiac arrest (OHCA) patients using audio and visual feedback improves the quality of resuscitation (16).
Parikh et al. (17) demonstrated that the debriefing technique decreases ventilation, increases compression depth, and improves chest recoil in NICU nurses using an infant manikin. Like the present study, their research was conducted in a workshop setting using manikins. The debriefing technique involves operators sharing their practical, emotional, and psychological experiences with other members of the resuscitation team after each CPR operation (17).
The results of a systematic review (18) indicated that CPR using real-time audiovisual feedback (RTAVF) devices improves the quality of CPR in cases of in-hospital cardiac arrest (IHCA) and enhances CC depth. However, it does not significantly affect the return of spontaneous circulation in OHCA, survival to hospital discharge, or CC rate (18). This difference may be because, during IHCA, a dedicated nurse can focus exclusively on performing high-quality CPR, whereas in OHCA, paramedics often face multiple tasks, including performing CPR while ensuring the patient is safely transported to the hospital (2).
Generally, feedback is a vital component of medical education. By continuously improving feedback practices, healthcare professionals can be equipped with the necessary skills and competencies (19). The success of the CC process largely depends on proper timing and the skill level of those involved in the resuscitation process (20). According to the 2017 AHA guidelines, audio-visual feedback is essential for all CPR training (21). Nurses and medical staff employed in hospitals are at the forefront of caring for patients requiring CPR (22). Therefore, providing standard training to nurses using appropriate equipment is of paramount importance (23). Moreover, further studies are needed to evaluate the optimal frequency of CPR training, the duration of practical sessions, and the comparison of real-life CPR performance on patients with training conducted on manikins (24).
This study has some limitations: Focusing solely on nurses limits the generalizability of the results to other groups, and since the study was conducted in an educational environment, the results might differ when repeated under psychological pressure in real-life scenarios. Given the significant decrease in nurses' CPR quality scores during the two-month follow-up assessment, it is recommended to repeat training sessions at least once every three months to enhance retention.
5.1. Conclusions
The use of direct feedback, visual feedback, and combined feedback can significantly improve the quality of CC in nurses. Notably, the combined approach of using both direct and visual feedback achieves higher quality improvements and ensures better continuity, underscoring its potential value in resuscitation training.