1. Background
The COVID-19 pandemic, originating in China in 2019, rapidly became a global crisis, profoundly disrupting life and posing significant challenges (1). The most common psychological responses included stress, anxiety, fear, anger, and social withdrawal, with healthcare workers facing additional burdens due to increased responsibilities (2). The nursing profession, in particular, encountered substantial challenges throughout the pandemic. Evolving protocols, high transmissibility, and uncertainties increased nurse stress, affecting care quality (3). Research indicates that nurses experienced considerable psychosocial effects due to prolonged hours in protective gear, isolation, disease transmission risk, and the loss of colleagues (4). These factors underscore the importance of assessing anxiety among nurses. Moreover, mass quarantine measures further exacerbated stress and anxiety levels among healthcare professionals (5). High contagion rates were closely linked to increased stress, particularly among nurses (6). The fear of contracting COVID-19 and transmitting it to loved ones, coupled with traumatic experiences such as patient suffering, intensified anxiety (5, 6). During the pandemic, nurses frequently experienced insomnia, anxiety, depression, burnout, and feelings of helplessness and hopelessness (7). In critical situations such as the COVID-19 pandemic, nurses faced challenging working conditions and resource limitations, further increasing their stress levels. A meta-analysis by Al Maqbali et al. revealed that one-third of nurses exhibited psychological symptoms (8). Research suggests that cognitive-behavioral and relaxation techniques effectively mitigate stress among nurses. Studies have demonstrated that progressive muscle relaxation (PMR) significantly reduces stress and fatigue while aiding in the management of compassion fatigue and burnout (8, 9). Progressive muscle relaxation, an integrative approach developed by Edmund Jacobson in 1934, enhances mental well-being by reducing stress and anxiety through sequential muscle contraction and relaxation (10-12). Jacobson emphasized the importance of recognizing muscle tension and its role in stress regulation. A study by Ganjeali et al. demonstrated that nurses caring for COVID-19 patients who practiced PMR for 20 minutes daily over two weeks experienced significant reductions in anxiety and stress scores (10). Similarly, Liu et al. reported PMR’s effectiveness in alleviating anxiety among COVID-19 patients (11), while Toqan et al. found that it reduced anxiety in nursing students entering clinical practice (12). Despite extensive research on PMR’s effects in patients, few studies have explored its impact on stress and anxiety among nurses during the COVID-19 pandemic. Therefore, this study aimed to assess the effects of web-based progressive relaxation on stress and anxiety levels among nurses working in corona epidemic hospital.
2. Objectives
This study aimed to assess the impact of web-based progressive relaxation exercises (PRE) on stress and anxiety in nurses at a corona epidemic hospital.
3. Methods
3.1. Design Study
This randomized controlled intervention study determined the effect of web-based PRE on stress and anxiety in nurses at a corona epidemic hospital.
3.2. Participants
The study population consisted of 1078 nurses from a corona epidemic hospital in eastern Turkey, with 64 nurses agreeing to participate between March and April 2021. Nurses who met the inclusion criteria were invited via Google survey WhatsApp groups. The sample size per group was calculated as 22 with 80% power and 0.05 error, so 64 nurses (32 experimental, 32 control) were included to account for potential 40% data loss. Nurses were randomly assigned sequence numbers and randomized using randomizer. Inclusion criteria were nurses aged 18 - 55, not using anxiolytics or psychoactive drugs, not trained in Jacobson's PMR, and not experiencing a critical event in the last six months.
3.3. Scales
The study data were collected using the personal information form, the Perceived Stress Scale (PSS), and the State-Trait Anxiety Inventory (STAI).
3.3.1. Personal Information Form
The study examined nurses’ socio-demographics, work conditions, and COVID-19's impact on family life and concerns (10-12).
3.3.2. The Perceived Stress Scale
The PSS, developed by Cohen et al. (1983) to assess stress levels, was adapted to Turkish by Eskin, including self-efficacy and stress perception factors (13). It is a 14-item, five-point Likert-type scale, with participants rating each item from "Never (0)" to "Very often (4)." Seven of the items with positive statements are scored in reverse. The PSS-14 scores range from 0 to 56, with higher scores indicating increased stress, where 0 - 35 represents normal stress and 35 - 56 indicates stress. The original scale's Cronbach's alpha was 0.84, with a test-retest reliability of 0.85, and in Eskin, it was 0.84 with a reliability of 0.87 (13). In our study, Cronbach's alpha was 0.865 for the PSS pre-test and 0.847 for the post-test.
3.3.3. State-Trait Anxiety Inventory
The STAI, developed by Spielberger et al. in 1970 to measure state anxiety, is widely used, with its validity and reliability in Turkey established by Öner and LeCompte (14). The 20-item, 4-point Likert-type scale measures anxiety at a given time, with responses ranging from "not at all" to "totally." Ten items (1, 2, 5, 8, 10, 11, 15, 16, 19, 20) are reversed, where the scoring is inverted (1 to 4, 4 to 1), with a higher score indicating higher anxiety in the direct items and lower anxiety in the reversed items. The final score is calculated by subtracting the reverse statement score from the direct statement score and adding 50. The STAI reliability was reported by Öner and LeCompte as 0.94 - 0.96, with scores of 0 - 30 indicating low, 30 - 44 moderate, and above 45 high anxiety (14). In our study, Cronbach's alpha was 0.918 for the pre-test and 0.924 for the post-test.
3.3.4. Progressive Muscle Relaxation Exercise
Jacobson’s progressive relaxation technique involves contracting and relaxing large muscle groups in a controlled manner, performed while sitting or lying down with slow breathing and optional music (15).
3.4. Data Collection
The 64 nurses who accepted participation were informed via Zoom. Data collection tools were shared online and applied to both groups at the pre-test stage. In the intervention group, PRE were taught in two sessions, covering its definition, purpose, benefits, and steps. The PRE video and guide were shared on WhatsApp groups to ensure that all participants had clear instructions on how to perform the exercises correctly. One month later, post-test measurements for the PSS and the STAI were conducted to assess the effectiveness of the intervention. To prevent information transfer to the control group, separate communication channels were used, with the intervention group having exclusive access to the WhatsApp group. The control group received no PRE information during the study, and materials were provided only after the study concluded to maintain study integrity. Participants were instructed to maintain anonymity and confidentiality by not disclosing their group allocation or intervention details, ensuring the trial’s credibility and preventing bias.
3.5. Practicing Progressive Relaxation Exercises
In the first session, the nurses were informed about the study and procedure. The 60-minute Zoom training on PRE explained the technique’s definition, purpose, benefits, and application. In the second session, the researcher demonstrated and practiced PRE with the nurses. PRE videos were shared via WhatsApp, and nurses were instructed to practice daily for 25 - 30 minutes for a month, with daily reminders. Nurses shared information on WhatsApp for four weeks. After the intervention group’s final tests, the control group received PRE training via CD and documents. The study reduced stress and anxiety through this structured approach.
3.6. Data Analysis
The SPSS 23.0 (statistical program for social sciences) package program was used to evaluate the data obtained from the research. The normality of variables was assessed using visual (histograms, probability plots) and analytical (Shapiro-Wilk test) methods. The Independent samples t-test compared normally distributed continuous variables between the control and intervention groups, while the chi-square test analyzed categorical variables. A paired samples t-test was used to compare pre- and post-intervention scale scores in the intervention group. Statistical significance was set at P < 0.05.
3.7. Ethical Considerations
Ethical approval (approval no: 2021-03-25) was obtained from Fırat University Non-interventional Research Ethics Committee before starting the research. Institutional permission and nurses' electronic informed consent were obtained from the City Hospital.
4. Results
A total of 64 participants, comprising 33 in the intervention group and 31 in the control group, participated in this randomized controlled clinical trial. Nurses in the intervention and control groups were similar in terms of age, gender, length of employment, marital status, and graduation status. There was no difference between the groups in terms of these descriptive features (P > 0.05). The socio-demographic data of the participants, such as age, length of employment, gender, number of children, and information on working conditions, are shown in Table 1.
| Variables | Intervention (n = 33) | Control (n = 31) | Statistics | P-Value |
|---|---|---|---|---|
| Age; mean ± SD | 28.6 ± 5.0 | 30.5 ± 5.5 | t = -1.465 | 0.148 b |
| Working time in the profession (mon); median (IR) | 60.0 (93) | 96.0 (84) | Z = -0.937 | 0.349 c |
| Number of children; median (IR) | 0 (1) | 1 (2) | Z = -2.174 | 0.030 c |
| Gender | 0.083 d | |||
| Female | 25 (75.8) | 29 (93.5) | ||
| Male | 8 (24.2) | 2 (6.5) | ||
| Marital status | χ2 = 2.202 | 0.138 e | ||
| Married | 12 (36.4) | 17 (54.8) | ||
| Single | 21 (63.6) | 14 (45.2) | ||
| Graduation status | 0.142 d | |||
| Associate degree | 2 (6.1) | 6 (19.4) | ||
| Bachelor's degree | 31 (93.9) | 25 (80.6) | ||
| Working time in the profession | χ2 = 0.636 | 0.728 e | ||
| Up to 10 years | 21 (63.6) | 18 (58.1) | ||
| 11 – 20 years | 8 (24.2) | 7 (22.6) | ||
| 21 years and more | 4 (12.1) | 6 (19.4) | ||
| Worked service | χ2 = 1.558 | 0.459 e | ||
| Surgical clinic | 8 (24.2) | 6 (19.4) | ||
| Emergency | 12 (36.4) | 8 (25.8) | ||
| Intensive care | 13 (39.4) | 17 (54.8) | ||
| Weekly working time (h) | 1.000 d | |||
| 40 - 48 | 29 (87.9) | 27 (87.1) | ||
| 49 - 56 | 4 (12.1) | 4 (12.9) | ||
| Manner of work | 0.041 d | |||
| Night | 2 (6.1) | 8 (25.8) | ||
| Day and night | 31 (93.9) | 23 (74.2) |
Abbreviations: n, number of participants; SD, standard deviation; IR, interquartile range.
a Values are expressed as No. (%) unless otherwise indicated.
b Independent samples t-test
c Mann Whitney U-test.
d Fisher's Exact test.
e Chi-square.
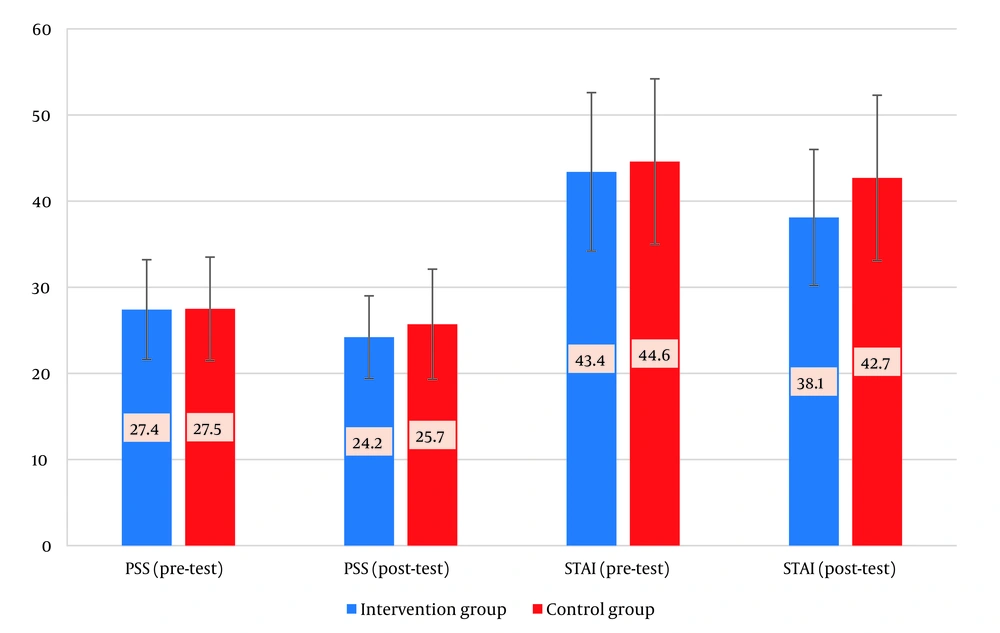
The PSS and STAI levels were found to be similar in the pre-application evaluation in the intervention and control groups (P = 0.918, P = 0.589, respectively). A statistically significant decrease was found in PSS and STAI levels after the progressive relaxation exercise applied to the intervention group (P = 0.006, P = 0.002, respectively) (Table 2 and Figure 1). There was no significant difference in PSS and STAI scores between the first and second evaluations in the control group. While STAI scores before the application were at similar levels in the intervention and control groups (P = 0.589), they were found to be significantly lower in the intervention group than in the control group after the application (P = 0.037) (Table 2 and Figure 1).
| Variables | Intervention (n = 33) | Control (n = 31) | t | P-Value b |
|---|---|---|---|---|
| PSS | t = 2.974; P = 0.006 c | t = 1.719; P = 0.096 c | ||
| Pre-intervention | 27.4 ± 5.8 | 27.5 ± 6.0 | -0.103 | 0.918 |
| Post-intervention | 24.2 ± 4.8 | 25.7 ± 6.4 | -1.059 | 0.294 |
| STAI | t = 3.392; P = 0.002 c | t = 1.180; P = 0.247 c | ||
| Pre-intervention | 43.4 ± 9.2 | 44.6 ± 8.7 | -0.543 | 0.589 |
| Post-intervention | 38.1 ± 7.9 | 42.7 ± 9.6 | -2.128 | 0.037 |
Abbreviations: n, number of participants; SD, standard deviation; PSS, Perceived Stress Scale; STAI, State-Trait Anxiety Inventory.
a Values are expressed as mean ± SD.
b Independent samples t-test.
c Paired samples t-test.
5. Discussion
This randomized controlled study assessed the effects of Web-Based PRE on stress and anxiety in nurses during the COVID-19 pandemic. Caring for patients with COVID-19 challenges nurses, leading to stress and anxiety. Effective intervention strategies are crucial for preventing complications because PRE reduces stress and anxiety in nurses caring for patients with COVID-19. Stress, which is commonly experienced by nurses during the COVID-19 pandemic, negatively affects their physical and mental health. Studies have shown that nonpharmacological methods, such as massage, yoga, and music therapy, can reduce stress in nurses (16).
In our study, PSS scores significantly decreased in the intervention group with PRE, whereas no significant change occurred in the control group (P < 0.05, Table 1 and Figure 1). The literature suggests the use of various methods to help nurses manage stress and anxiety (17). Kim et al.’s used PRE as an intervention because of its effectiveness in treating psychosomatic disorders, such as anxiety and stress (17).
Studies have shown that PRE effectively reduces nurses’ anxiety levels. Akyurek et al. applied progressive relaxation, posture, and breathing exercises for five weeks to nurses in the intervention group under the Workplace Health Promotion Program. Pre- and post-intervention measurements showed reduced pain, fatigue, and stress, along with improved coping skills and quality of life (18). Veiga et al. applied PRE to nurses for 20 minutes a day for eight weeks and found significant reductions in emotional exhaustion, depression, and salivary cortisol levels in the intervention group compared with the control group (19). In another study, Ozgundondu and Gok Metin reported that 20-min PMR exercises with music reduced stress and fatigue levels and improved stress coping skills in Intensive Care Unit nurses. The study revealed a significant reduction in stress scores in the intervention group, highlighting PRE as an effective, cost-free method to reduce anxiety among nurses during challenging times (20).
In addition to studies combining relaxation exercises with music therapy, other studies have examined the effects of mindfulness-based meditation and yoga on stress reduction among nurses. Lin et al. reported that their eight-week mindfulness-based program reduced stress and negative emotions while increasing positive emotions and resilience in nurses. Protecting nurses’ mental health is crucial for effective patient care because the impact of stress depends on coping behavior adequacy (21).
This study found a significant reduction in anxiety levels among the intervention group nurses (P < 0.05, Table 1, Figure 1). In this context, the study showed that PMR effectively reduces anxiety. Nurses' anxiety reduces efficiency, raises health risks, and lowers healthcare satisfaction (11). Effective interventions such as PMR can reduce the negative impact of stress and anxiety on mental health and care quality. Liu et al. found that PMR positively reduces anxiety in patients with COVID-19 (11). Ozlu et al. stated that PMR is a nonpharmacological method to reduce anxiety in patients with COVID-19 (22). Similarly, Ozgundondu and Gok Metin found that PMR and the intensive care they attended reduced stress (20).
Studies have shown that PRE reduces nurses' anxiety, with Ganjeali et al. finding a significant decrease in the intervention group (10). Carver and O'Malley found that pretreatment significantly reduced anxiety in student nurses compared to the control group. Controlling emotions in tense situations can be achieved by learning how to relax the muscles (23).The consistency between this study and previous studies stems from the complementary medicine approach, which considers relaxation techniques necessary for reducing stress and anxiety (20-23).
5.1. Limitations
This study is limited to one hospital, self-reported data, and uncontrolled stressors, underscoring the need for larger, diverse samples.