1. Background
Trauma significantly impacts societal health, imposing substantial economic and social costs and leading to long-term impairments in young, productive individuals (1). It accounts for 10% of all deaths worldwide (2). The increase in motor vehicle usage has resulted in a rise in traumatic accidents (3), with 25% of these injuries affecting the chest (4). Emergency medical technicians (EMTs) are typically the first responders to trauma cases, and their skills are crucial for patient survival (5). Effective decision-making during emergencies is vital for patient care (6). A better understanding of clinical decision-making can enhance clinical and organizational interventions, thereby improving treatment outcomes (7). The EMTs must rapidly assess situations, diagnose issues, manage crises, and refer patients for appropriate treatment (8). Their awareness can be life-saving during the critical early "golden hour" (9).
Continuous training using the latest methods is essential to maintain EMTs' knowledge and skills (10). Unfortunately, the issue of clinical decision-making in training emergency technicians for pre-hospital settings has not received adequate attention (11), and current teaching methods are not as effective as they should be in developing this vital skill (12). Most workshops are conducted in face-to-face environments (13), which present challenges such as high costs, logistical difficulties, participant absence due to work or distance, low engagement, and limited capacity for larger groups (14). However, advancements in communication technologies now enable effective teaching and learning without the need for face-to-face interactions (13).
Electronic learning is a modern educational approach that utilizes communication and information technology, allowing for flexible content distribution and learning without a specific location or time (15). A key aspect of this method is the use of active teaching techniques, such as scenario-based education, which promotes student engagement through discussion, creativity, and problem-solving (16). Due to the limitations of in-person workshops for pre-hospital emergency personnel during crises like COVID-19, virtual workshops have gained importance. It is essential to enhance their quality by integrating active learning methods (17). Most virtual education still relies on lectures, and there is limited research on the effectiveness of active learning techniques, such as scenario-based webinars, for improving decision-making skills. Further research is needed to better understand and improve virtual education approaches.
2. Objectives
Given the limitations of previous studies in this area, this study was designed and conducted to examine the effect of webinar training on chest trauma management using two methods — lecture-based and scenario-based — on the clinical decision-making skills of EMTs.
3. Methods
3.1. Study Design
This interventional study involved EMTs employed at pre-hospital emergency centers in South Khorasan, 2022.
3.2. Participants
Emergency medical technicians with post-graduate degrees or bachelor's degrees and at least one year of work experience, who had access to the internet via a smartphone, laptop, or computer, were included in the study. Technicians who did not attend at least two-thirds of the training sessions or had incomplete questionnaires were excluded from the study. According to the results of Sadeghnezhad et al.'s study (18), and based on the formula for comparing two means with a mean difference of 6.59, s1 = 3.68, s2 = 2.98, α = 0.05, and β = 0.90, the minimum sample size was estimated to be 6 EMTs for each group. This study used a final sample size of 25 participants per group, considering that educational interventions require a minimum sample size of 25 participants for each intervention group (19).
Sampling was conducted using the available sampling method, where a sample is drawn from conveniently available subjects (20). To ensure equal distribution of samples, eligible participants were divided using randomized block sampling. Thirteen blocks of four letters each were created with random combinations of A (lecture-based) and B (scenario-based). At each stage, a block was randomly selected using a random number table, and participants were assigned to one of the two study groups until the desired sample size was reached.
3.3. Scales
Based on six chest trauma scenarios — compression pneumothorax, hemothorax, floating chest, cardiac tamponade, aortic dissection, and rib fracture — 15 questions were designed for both groups, with 5 options (decision cards) developed for each question. These questions were crafted using two books: Pre-hospital Emergency Medicine (21) and Trauma Case Studies for the Paramedic (22). To confirm the content validity of the questionnaire, consultations were held with 5 academic staff members, 5 emergency medicine specialists, and 5 trauma specialists, and the questionnaire was subsequently modified based on their feedback. To assess reliability, the questionnaire was completed by 10 pre-hospital emergency technicians who did not participate in the main study, resulting in a Cronbach's alpha of 0.86.
The Q-Sort method was employed to measure the quality of clinical decisions, consisting of four steps. The first step involves collecting relevant ideas, beliefs, and opinions concerning the research object, which can be based on various sources such as interviews, content analysis, or previous research. The second step involves selecting and formulating a set of meaningful statements, resulting in the Q-sample. These statements are randomly numbered and printed on separate cards. In the third step, respondents express their views on the research topic by placing all cards in the pre-structured Q-sort distribution. The fourth step is data analysis, where a correlation matrix is created from all Q-sorts, indicating the degree of correspondence between respondents. This matrix is submitted to a by-person factor analysis to explore attitudinal groupings. Factor scores are computed for each item in the resulting clusters of respondents, leading to one representative Q-sort per group. Additionally, confounding respondents (loading significantly on more than one factor) and non-significant respondents (not loading on any factors) are identified. The final task is to interpret and explain similarities and differences among the factors (18, 23).
The Williamson system was used to score the cards. If the option chosen by the technician met all the standard items, a score of 4 was given; if some items were not met, a lower score was assigned. Thus, a useful card received 4 points, a facilitator card but not the main card received 3 points, a card neither promoting nor hindering care received 2 points, an unnecessary or discomfort-causing card received 1 point, and an inappropriate card received 0 points. The score range was 0 - 60, with a higher score indicating greater clinical decision-making power (18).
3.4. Data Collection
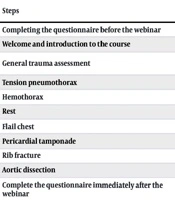
Participants in both groups were informed and provided with a pre-test questionnaire via WhatsApp. A 4-hour webinar training course, consisting of two 2-hour sessions, was conducted on the Adobe Connect platform by an assistant professor specializing in Health in Disasters and Emergencies, along with a master's degree student in nursing. The training, focusing on either webinar-based or scenario-based methods, included interactive scenarios and videos, followed by a test after each scenario. Upon completion of the course, the questionnaire was redistributed to both groups via WhatsApp (Table 1).
| Lecture-Based Webinar | Scenario-Based Webinar | ||
|---|---|---|---|
| Steps | Time (min) | Steps | Time (min) |
| Completing the questionnaire before the webinar | 30 | Completing the questionnaire before the webinar | 30 |
| Welcome and introduction to the course | 10 | Welcome and introduction to the course | 10 |
| General trauma assessment | 40 | General evaluation of trauma along with scenario planning and questions and answers | 40 |
| Tension pneumothorax | 40 | Pressure pneumothorax with scenario plan and questions and answers | 40 |
| Hemothorax | 30 | Hemothorax with a scenario plan and questions and answers | 30 |
| Rest | 15 | Rest | 15 |
| Flail chest | 30 | Flail chest with scenario plan and questions and answers | 30 |
| Pericardial tamponade | 30 | Pericardial tamponade with a scenario plan and questions and answers | 30 |
| Rib fracture | 30 | A rib fracture with scenario plan and questions and answers | 30 |
| Aortic dissection | 30 | Aortic dissection with a scenario plan and questions and answers | 30 |
| Complete the questionnaire immediately after the webinar | 30 | Complete the questionnaire immediately after the webinar | 30 |
Summarize of Study Implementation Educational Contents Based on Study Groups
3.5. Data Analysis
Data were analyzed using SPSS 22. Data normality was checked by the Kolmogorov-Smironov test. Fisher's exact test, independent samples t-test and paired t-test were used for analytical analysis at a significance level of 0.05.
3.6. Ethical Consideration
The Birjand University of Medical Sciences ethical committee approved this study (IR.BUMS.REC.1400.373). All participants filled out the informed consent form and were assured that their information would not be published individually.
4. Results
The mean age of participants in the lecture-based and scenario-based groups was 27.7 ± 3.8 and 27.2 ± 4.0, respectively, with no statistically significant difference (P = 0.67). Additionally, there were no significant differences in education level, employment type, or marital status between the two groups (P > 0.05) (Table 2).
| Variables | Lecture-Based | Scenario-Based | P-Value |
|---|---|---|---|
| Age | 27.7 ± 3.8 | 27.2 ± 4.0 | 0.67 b |
| Education | 0.51 c | ||
| Postgraduate | 20 (80) | 18 (72) | |
| Bachelor's degree | 5 (20) | 7 (28) | |
| Type of employment | 0.054 d | ||
| Designated recruitment | 3 (12) | 7 (28) | |
| Contract employment | 18 (72) | 18 (72) | |
| Official employment | 4 (16) | 0 (0) | |
| Marriage status | 1 c | ||
| Single | 11 (44) | 11 (44) | |
| Married | 14 (56) | 14 (56) |
Comparison of Frequency Distribution of Basic Features in Two Studied Groups a
The results of the independent samples t-test indicated that the mean score of decision-making skills before the intervention was not significantly different between the lecture and scenario groups (P = 0.76). However, after the intervention, the mean score of decision-making skills in both groups increased significantly (P = 0.017). The mean score increase in the scenario-based group (7.44 ± 5.8 points) was significantly higher than the increase in the lecture group (3.44 ± 3.9 points). This difference was statistically significant (P = 0.007) (Table 3).
5. Discussion
This study compared the effects of lecture-based and scenario-based webinar training on EMTs' decision-making skills in managing chest trauma. Both methods significantly improved scores, but the scenario-based group showed greater increases than the lecture-based group. This study is the first to compare two training methods for improving a clinical skill in a virtual environment. Prior research has mainly focused on comparing in-person training methods or contrasting them with virtual training. Hashemiparast et al. found that electronic education and lectures equally enhance the awareness of administrative staff in clinical departments about hospital infection control (24). Hosseinzadeh et al. found that a 4-week scenario-based training significantly improved students' critical thinking skills (25). A systematic review and meta-analysis also indicated that such simulation courses enhance nursing students' knowledge, clinical skills, and self-confidence (26). The current study found that the scenario-based learning group significantly outperformed the lecture-based group in improving clinical decision-making skills. Parvaresh et al. also demonstrated that both scenario and lecture methods positively affected awareness of chest trauma management, with the scenario group showing notably higher levels (16). Additionally, scenario-based training improved EMTs' clinical decision-making, satisfaction, and reduced stress (11, 27). Researchers regard scenario-based learning as an effective, dynamic approach that enhances analytical thinking, problem-solving, communication, and teamwork while boosting self-confidence, minimizing common errors in practical assessments, and facilitating knowledge retrieval (28-30).
In general, virtual education addresses the limitations of traditional learning and offers numerous opportunities for employees and students in low- and middle-income countries (31). It is accessible to anyone with a computer, tablet, or smartphone, regardless of time and location (32). Many qualified individuals cannot attend in-person workshops due to work schedules or distance (33), making virtual education an effective alternative that increases learner participation (34). Previous studies indicate that virtual education can be as effective as traditional education in theoretical learning (35, 36). However, some research suggests that face-to-face education is more effective for developing practical skills (33). In face-to-face workshops, direct interaction with instructors in a safe environment enhances skill acquisition (33). More research is needed to compare virtual education methods and improve quality in clinical skills training.
Furthermore, this study focused on individuals with degrees in emergency medicine. However, due to a manpower shortage in Iran, graduates from fields like nursing and anesthesia are also working in pre-hospital emergency services. Therefore, integrated training is essential to accommodate the diverse backgrounds of these professionals.
5.1. Conclusions
Considering that the clinical decision-making skills of emergency technicians improved more after the intervention using the scenario method compared to the lecture method, it can be concluded that scenario-based training, even in a virtual setting, is a more effective approach than traditional training methods. This teaching method allows learners to experience situations closer to reality, thereby reducing the gap between theoretical education and practical application by engaging them with real scenarios they may encounter. Therefore, educational planners should consider using this method to achieve better outcomes.