1. Background
Congenital heart diseases (CHD) constitute the majority of chronic diseases in children. The prevalence of CHD remains geographically variable, with a global estimate of 80 - 90 per 10,000 live births (1). Although CHD is one of the most common significant diseases, there is limited knowledge about its causes. It is associated with a certain portion of neonatal deaths (2). About 30% of infants with congenital heart anomalies die within one month of birth without any treatment (3). However, it is possible to detect these diseases very quickly with pulse oximetry. Screening newborns with pulse oximetry after the 24th hour is more effective in diagnosing critical CHD than physical examination alone, emphasizing the importance of screening, especially in cases of increased risk for CHD (4, 5).
Due to rapid scientific and technological developments in medicine, the life expectancy of newborns and children with CHD has increased. However, this has brought challenges as children face the symptoms of the disease throughout their lives (6). The disease process introduces significant changes and restrictions to the child's life, leading to an increase in emotional and social problems (2, 5, 6). Additionally, congenital and lifelong chronic diseases reduce the quality of life for children and families, having very negative effects on their lives (7, 8).
Alexithymia is defined as emotional deprivation, limited perception of emotional messages, and problems in self-expression (9, 10). A child diagnosed with a chronic disease is at risk for alexithymia, characterized by limited imaginative thinking ability, inability to classify physiological reactions, and inability to explain emotions. Alexithymic children are often withdrawn, exhibit shy behaviors, and have lower self-confidence than other individuals (7, 8).
Attitudes are defined as acquired orientations that direct individuals towards certain people, objects, and phenomena, leading them to form distinctive behaviors (9). Attitudes begin to emerge in childhood, and it is very difficult to change behaviors that appear in childhood during adulthood. Changing people's attitudes is an effective method to facilitate changes in their situations that are reflected in their behaviors (2, 7). The emotions felt and the attitude towards the diagnosis of a chronic disease affect coping methods and adaptation to the disease. In the literature, the attitude of a child diagnosed with a chronic disease towards their illness, how they cope with related problems, and how they adapt to the disease is an important factor (2).
Secondary alexithymia can occur after a stressful situation, major illness, surgical procedure, or trauma. Congenital heart disease is a problem that strains children and causes stressful situations. Therefore, alexithymia may develop in these children, affecting their attitudes towards their own illness (8, 10).
2. Objectives
In this context, the aim of this study was to examine the relationship between the alexithymic characteristics of children diagnosed with CHD and their attitudes towards their illness.
3. Methods
3.1. Study Design
The study is cross-sectional and descriptive.
3.2. Participants
No specific sample selection was made; 135 children aged 11 - 14 years who were diagnosed with CHD and attended the pediatric cardiology polyclinic during the study period were initially included. However, since some children and their families did not wish to participate, the study was completed with 104 children and their families. Sample calculation was performed using power analysis. The scale mean and standard deviation (SD) obtained from a sample study (11, 12) were found to be 0.41. With the power of the test set at 0.90 (α = 0.05, 1-β = 0.90), the minimal sample size was calculated to be 102 children.
3.3. Scales
3.3.1. Information Form for Child and Family
The Information Form for Child and Family, consisting of 22 questions, was created by the researcher through a review of the literature. It includes questions designed to determine sociodemographic characteristics (questions 1 - 8).
3.3.2. Alexithymia Scale for Children
The scale was developed by Rieffe et al. in 2006 to measure the level of alexithymia in children (13). It consists of 20 items, with each item receiving a value between 0 and 2. Scale scoring is obtained by summing these values and dividing by 20 (11). The Cronbach's alpha internal consistency coefficient of the Turkish version of the scale was reported as 0.78. In our study, the Cronbach's alpha coefficient of the scale was determined to be 0.79.
3.3.3. The Child Attitude Toward Illness Scale
The Child Attitude Toward Illness Scale was developed by Austin and Huberty in 1993 to examine the attitudes of children with chronic diseases in relation to their conditions (14). The scale includes 13 items with a five-point Likert-type rating, and 4 of the 13 items consist of bipolar adjectives (very good, slightly good, not sure, slightly bad, very bad). The ninth item on the scale evaluates how often children experience positive or negative feelings about having a chronic disease (very often, often, sometimes, not often, never) (12). In our study, the Cronbach's alpha coefficient of the scale was found to be 0.83, indicating high reliability.
3.4. Data Collection
Research data were obtained through face-to-face interviews. Parents were interviewed solely to obtain permission. Family members were consulted on questions that the children were unable to answer, such as the family's economic situation and the mother's education level.
3.5. Data Analysis
In the statistical analysis, the conformity of numerical variables to a normal distribution was examined using the Kolmogorov-Smirnov test and histogram graphs. Linear regression analysis was also utilized. Parametric tests (t-test, one-way ANOVA) were used for normally distributed data, while nonparametric tests (Kruskal-Wallis, Mann-Whitney U) were used for non-normally distributed data. The results were evaluated at a significance level of P < 0.05 within a 95% confidence interval.
3.6. Ethical Consideration
Before commencing the research, the necessary ethical approval was obtained from the Non-Interventional Research Ethics Committee (decision no: 2020/066).
4. Results
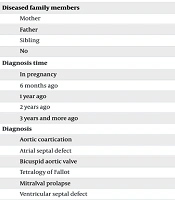
Information regarding the participants' diseases is provided in Table 1. It was determined that there was significance in terms of the duration of diagnosis, types of diagnosis, emotional expression, and school attendance of the children. Alexithymia Scale for Children (ASC) scores were found to be high in children who were newly diagnosed, had complex diagnoses, expressed that they could not express their emotions, and could not attend school. The type of diagnosis, hospitalization, additional chronic disease status, continuous drug use, state of expressing emotions, and school attendance status of the children were found to be statistically significant in terms of Child Attitude Toward Illness Scale (CATIS) mean scores. Children who had an atrial septal defect, had little or no hospitalization, did not use continuous medication, could not express their emotions, and could attend school regularly were found to have high CATIS mean scores (Table 1).
| Data on the Disease | Values | ASC | Significance | CATIS | Significance |
|---|---|---|---|---|---|
| Disease status in family members other than the child | P = 0.21; t = 1.26 | P = 0.33; t = 0.97 | |||
| Yes | 25 (24.0) | 21.96 ± 4.14 | 2.77 ± 0.44 | ||
| No | 79 (76.0) | 20.83 ± 3.78 | 2.87 ± 0.42 | ||
| Diseased family members | P = 0.78; F = 0.24 | P = 0.30; F = 1.30 | |||
| Mother | 5 (4.8) | 21.00 ± 2.12 | 2.95 ± 0.41 | ||
| Father | 4 (3.8) | 23.00 ± 3.74 | 2.48 ± 0.26 | ||
| Sibling | 16 (15.4) | 22.00 ± 4.78 | 2.79 ± 0.47 | ||
| No | 79 (76.0) | 20.83 ± 3.78 | 2.87 ± 0.42 | ||
| Diagnosis time | P = 0.007; χ2 = 13.93 | P = 0.11; χ2 = 7.59 | |||
| In pregnancy | 25 (24.0) | 19.52 ± 3.98 | 2.94 ± 0.42 | ||
| 6 months ago | 15 (14.4) | 20.20 ± 4.81 | 3.06 ± 0.51 | ||
| 1 year ago | 17 (16.3) | 23.11 ± 3.27 | 2.70 ± 0.44 | ||
| 2 years ago | 12 (11.5) | 23.00 ± 2.29 | 2.62 ± 0.35 | ||
| 3 years and more ago | 35 (33.7) | 21.10 ± 3.88 | 2.84 ± 0.38 | ||
| Diagnosis | P = 0.02; F = 2.81 | P = 0.001; F = 5.88 | |||
| Aortic coartication | 17 (16.4) | 21.88 ± 3.98 | 2.61 ± 0.34 | ||
| Atrial septal defect | 46 (44.3) | 19.69 ± 3.55 | 3.03 ± 0.54 | ||
| Bicuspid aortic valve | 11 (10.6) | 21.09 ± 3.70 | 2.86 ± 0.53 | ||
| Tetralogy of Fallot | 6 (5.8) | 23.33 ± 5.75 | 2.30 ± 0.34 | ||
| Mitralval prolapse | 13 (12.5) | 23.00 ± 2.48 | 2.79 ± 0.24 | ||
| Ventricular septal defect | 11 (10.6) | 22.36 ± 4.00 | 2.79 ± 0.51 | ||
| Hospitalization | P = 0.32; F = 1.14 | P = 0.01; F = 4.59 | |||
| None | 70 (67.3) | 20.80 ± 3.62 | 2.91 ± 0.41 | ||
| 1 time | 19 (18.3) | 21.15 ± 4.16 | 2.83 ± 0.36 | ||
| 2 time and more | 15 (14.4) | 22.46 ± 4.64 | 2.55 ± 0.49 | ||
| Additional chronic disease status | P = 0.23; U = 831.00 | P = 0.03; U = 291.50 | |||
| Yes | 13 (12.5) | 22.76 ± 4.30 | 2.53 ± 0.33 | ||
| No | 91 (87.5) | 20.86 ± 3.78 | 2.89 ± 0.42 | ||
| Continuous drug use | P = 0.11; t = 1.59 | P = 0.0001; t = 4.09 | |||
| Yes | 41 (39.4) | 21.85 ± 4.28 | 2.65 ± 0.41 | ||
| No | 63 (60.6) | 20.61 ± 3.55 | 2.98 ± 0.40 | ||
| State of expressing emotions | P = 0.001; t = 6.86 | P = 0.001; t = 4.54 | |||
| Is having difficulty | 72 (69.2) | 22.55 ± 2.99 | 2.73 ± 0.35 | ||
| Isn’t having difficulty | 32 (30.8) | 17.84 ± 3.71 | 3.11 ± 0.47 | ||
| School attendance status | P = 0.04; F = 3.31 | P = 0.01; F = 7.42 | |||
| Regular | 92 (88.5) | 20.84 ± 3.68 | 2.91 ± 0.42 | ||
| Irregular | 8 (7.7) | 21.75 ± 4.39 | 2.50 ± 0.22 | ||
| None | 4 (3.8) | 25.75 ± 5.50 | 2.28 ± 0.39 | ||
| Loss of years in education | P = 0.51; t = 0.65 | P = 0.25; t = 1.15 | |||
| Yes | 24 (23.1) | 20.84 ± 3.68 | 2.76 ± 0.44 | ||
| No | 80 (76.9) | 21.75 ± 4.39 | 2.87 ± 0.42 |
Abbreviations: ASC, Alexithymia Scale for Children; CATIS, Child Attitude Toward Illness Scale.
a Values are expressed as No. (%) or mean ± SD.
The mean total ASC score of the participants was 21.10 ± 3.88, and the CATIS score mean was 2.85 ± 0.43 (Table 2). In the regression analysis, it was determined that there was a moderate negative relationship between the total mean score of ASC and the mean total score of CATIS (R = -0.48, R² = 0.23, P < 0.05). Accordingly, alexithymia explains 23% of children's attitudes towards their diseases. Additionally, a moderately negative relationship was found between the ASC sub-dimensions and CATIS, specifically between the ASC sub-dimensions of difficulty in identifying emotions and difficulty in expressing emotions, and CATIS (R = -0.50, R² = 0.25, P < 0.05; r = -0.53, R² = 0.29, P < 0.05) (Table 2).
| Independent Variables | Mean ± SD | F/P | R | R2 | r/P | t /P | Durbin-Watson | B | Beta |
|---|---|---|---|---|---|---|---|---|---|
| ASC | 21.10 ± 3.88 | 31.04/0.01 | 0.48 | 0.23 | -0.48/0.01 | 19.21/0.01 | 1.61 | -0.05 | -0.48 |
| Difficulty identifying emotions | 4.89 ± 1.81 | 34.70/0.01 | 0.50 | 0.25 | -0.50/0.01 | 32.21/0.01 | 1.75 | -0.12 | -0.50 |
| Difficulty expressing feelings | 5.18 ± 1.57 | 41.10/0.01 | 0.54 | 0.29 | -0.53/0.01 | 29.01/0.01 | 1.56 | -0.15 | -0.54 |
| Extrinsic oriented Thinking | 18.08 ± 1.59 | 0.24/0.87 | 0.02 | 0.01 | -0.02/0.43 | 5.67/0.01 | 1.73 | 0.004 | 0.02 |
| CATIS | 2.85 ± 0.43 | - | - | - | - | - | - | - | - |
Abbreviations: ASC, Alexithymia Scale for Children; CATIS, Child Attitude Toward Illness Scale.
5. Discussion
The aim of this study was to examine the relationship between the alexithymic characteristics of children diagnosed with CHD and their attitudes towards their illness. Although various socio-cultural factors are reported to affect alexithymia, it is particularly noted that mother-infant interaction and the environment in which the child grows up are much more influential in the formation of alexithymia (15). It has also been reported that secondary alexithymia occurs in children after serious illnesses that create a stressful situation (16). In a study conducted with children with chronic diseases, it was found that the total ASC score was quite high (17). The mean alexithymia scale scores of the participants in this study were also found to be quite high.
Attitudes can affect children's adaptation to chronic diseases and the course of the disease. Studies conducted with children with chronic diseases have reported that children's attitudes towards their diseases are negative and that their diseases progress more seriously (18). The general CATIS score averages of the participants in the study were found to be negative, with a mean of 2.85 ± 0.43. Additionally, the majority of children had negative attitudes.
The mean ASC score of participants diagnosed with atrial septal defect was found to be statistically significantly lower than the mean ASC scores of participants diagnosed with mitral valve prolapse and tetralogy of Fallot. The diagnosis of atrial septal defect is much simpler and less problematic for the patient than other cardiovascular diseases (19). Therefore, considering that these patients experience fewer problems and are hospitalized less, these findings were considered expected.
It was determined that participants who had difficulty expressing their feelings about their illness had high ASC scores. The definition of alexithymia includes difficulty expressing feelings and experiencing emotional deprivation (17).
It was found that the average ASC score of participants who attended school regularly was statistically significantly lower. In a study conducted with children referred to the child development unit in the hospital, it was found that these children had issues such as language and speech problems, sleep disorders, behavioral problems, sibling jealousy, parental attitudes, excessive television watching, excessive computer use, thumb sucking, masturbation, period-specific developmental difficulties, feeding problems, bedwetting, attention problems, nail biting, and fecal incontinence. Additionally, 56.3% (250) of these children scored below the mean on the developmental screening test (19).
It was determined that children with complex diagnoses had more negative attitudes towards their illnesses. This result suggests that the complex and difficult nature of the children's illnesses is related to their attitudes towards their illnesses. A study reported that children with more severe CHD had more behavioral and emotional problems than children with less severe CHD (12).
Participants who used medication regularly had a lower CATIS score average. In a study, it was determined that data such as children's medication use, severity of their illness, and frequency of epileptic seizures negatively affected children's attitudes towards their illnesses (13). Participants who stated that they had difficulty expressing their feelings about their illness were found to have lower CATIS score averages. A study reported that children's self-efficacy was related to their attitudes towards their illness (18). It is a known fact that individuals who lack self-efficacy have difficulty expressing themselves (17). Therefore, it is appropriate to reach this conclusion.
Participants who were able to attend school regularly had higher CATIS score averages. This result may be due to the fact that children who could not attend school regularly had disease diagnoses that involved a more problematic process.
In the study, we concluded that alexithymic behaviors in children are high and that these behaviors negatively affect children's attitudes towards their own diseases. Additionally, it was observed that the dimensions of defining and expressing emotions on the ASC had a negative effect on children's attitudes towards their own diseases. According to these results, alexithymia can be considered a significant predictor of children's attitudes towards their diseases. Attitudes can affect children's adaptation to chronic disease and the course of the disease. Studies conducted with children with chronic diseases have reported that children's attitudes towards their diseases are negative and that their diseases are more serious (10-18).
When we examined the general CATIS score averages of the participants in our study, they were found to be negative. Accordingly, we can conclude that children with alexithymic behavior have negative attitudes towards their own illnesses, and this negative situation may adversely affect the course of the children's illnesses.
The data used in this study are based on the statements of the children, so they cannot be evaluated as concrete results. Additionally, the sample is a limited group, and the evaluation was made based on a specific disease. Therefore, the results cannot be interpreted or generalized for all children with CHD. Furthermore, generalizations cannot be made for all children with or without disease.
5.1. Conclusions
Alexithymic individuals have difficulty coping with stress and anxiety because they are unable to understand and regulate their emotional states. This can lead to mental disorders such as depression, anxiety disorders, and post-traumatic stress disorder (PTSD) in the long term. The association between the illness attitudes of children diagnosed with CHD and alexithymic behaviors suggests that these behaviors affect the illness attitudes of children and that these children may experience mental health problems in the future. This poses a significant risk to children's health, considering the inadequacy of their coping methods.