1. Background
Old age is a period characterized by a loss of status, increased risk of dependency and accidents, and a decline in physical abilities. Hip fractures remain a significant health issue, leading to mortality and disability, particularly in the older adult population. It is reported that approximately one-third of individuals over the age of 65 experience a fall at least once annually (1). Approximately one-third of women and one in twelve men will suffer a hip fracture in their lifetime. According to the World Health Organization, the number of hip fractures associated with osteoporosis is projected to triple over the next 50 years, increasing from 1.7 million cases in 1990 to 6.3 million in 2050 worldwide (2). Hip fractures result in a 12 - 20% decrease in life expectancy and a 5 - 20% increase in disability rate within one year post-fracture (3). Patients with hip fractures are at high risk for age-related and fracture-related complications, even under optimal conditions (4). It has been determined that older adults who undergo hip fracture surgery face significant challenges in meeting their bathing, dressing, and toileting needs, often feeling dependent on others (5). Studies have confirmed that hip fractures have a strong and persistent negative impact on patients' quality of life (5, 6). Nursing care is emphasized as playing a crucial role in the recovery and return to normal life for individuals in the postoperative period (7). Older adults with a high quality of life can maintain independence and meet their needs and daily living activities themselves (8). Therefore, nurses have the opportunity to evaluate the healthy lifestyle behaviors and quality of life of the patients they care for, and to plan and implement assistance and home care optimally according to the patient's needs (9).
2. Objectives
The present study aimed to investigate the effect of home-based nursing care, in addition to routine care, on the quality of life and other challenges faced by older adults undergoing hip fracture surgery.
3. Methods
3.1. Study Design
The study was conducted as a semi-experimental design.
3.2. Participants
The research population consisted of 300 patients who visited a health center and a state hospital within the borders of Istanbul in 2018. From this population, the sample comprised 60 patients who volunteered to participate in the study. Patients were selected using a simple random sampling method. The sample size was determined to be sufficient at a 90% confidence interval. The patients were divided into two groups: (1) Control (N = 30), and (2) experimental (N = 30). Both groups were composed of patients with similar sociodemographic characteristics. The research sample included patients aged 65 and over who had undergone hip fracture surgery, were literate, and were mentally competent. No exclusion criteria were applied. The experimental and control groups were formed with patients having similar sociodemographic characteristics.
3.3. Scales
Patients were asked to complete the patient information form, hip evaluation form, and Quality of Life Scale.
3.3.1. Patient Information Form
The patient information form included questions about age, gender, marital status, and other demographic details.
3.3.2. Short Form Health Survey
The Short Form Health Survey (SF-36) was developed by Ware and Sherbourne in 1992 (10). The reliability and validity of the Turkish version were evaluated by Kocyigit et al. The scale includes 8 sub-dimensions (physical function, physical role, vitality/fatigue, pain, general health perception, social function, emotional role, mental health) and 2 main dimensions (physical dimension and mental dimension) (11). The SF-36 is scored such that higher scores in each health domain indicate a higher health-related quality of life. Scores for health-related life domains range from 0 to 100, with higher scores representing better health status.
3.3.3. The Oxford Hip Score
The Oxford Hip Score (OHS) was developed by Dawson et al. (12), and its validity and reliability for the Turkish population were established by Sendir and Babadag (13). The OHS consists of 12 statements covering aspects such as pain, washing, transportation, wearing socks, shopping, walking time, climbing stairs, getting up from a chair, limping, type of hip pain, night pain, and the effect of pain on daily activities. Each statement is scored on a Likert scale ranging from 1 to 5. Lower scores indicate less impact from the disease, while higher scores indicate greater impact.
3.4. Data Collection
In the procedure, patients in the control group received a brief training session upon discharge and were subsequently called for a routine check-up in the first month. The control group received routine care services at the hospital or health center. In contrast, the experimental group received home care services, including educational topics prepared by a specialist nurse, at the 1st and 3rd months post-discharge. The purpose of the research was explained to both the experimental and control groups, and data were collected using a face-to-face interview technique. The research sample consisted of patients aged 65 and over who had undergone hip fracture surgery, were literate, and mentally competent. The specialist nurse visited the homes of the patients in the experimental group during the first and third months after discharge to provide home care services and training. The specialist nurse administered the questionnaire to both the control and experimental groups at months 1 and 3.
3.4.1. Postoperative Discharge Education for Individuals with Hip Fracture Surgery
The training content included pain management, wound care, daily living activities, exercise, self-care, nutrition, monitoring for signs of complications, medication use, safety precautions at home, physical limitations, considerations for social and sexual life, use of assistive devices while walking, physical therapy as recommended by the doctor, and the importance of adhering to outpatient clinic follow-ups. Education was provided to patients by a specialist nurse and was supported with visual diagrams.
3.5. Data Analysis
The SPSS 22.0 statistical package program was used for data analysis. The Pearson’s chi-square test and Fisher's exact test were employed to compare qualitative data. The Mann-Whitney U test and Wilcoxon signed-rank test were used to compare the parameters. Results were evaluated at a significance level of P < 0.05. The content validity ratio (CVR) for the items was above 0.76, and the Content Validity Index (CVI) was above 0.79 in the SF-36. The CVR for the items was above 0.81, and the CVI was above 0.74 in the OHS.
3.6. Ethical Consideration
Permission for the study was received from the Ministry of Health, Turkish Public Hospitals Institution (70794255-663.08/12.01.2018).
4. Results
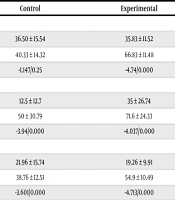
Descriptive characteristics of the groups are presented in Table 1. The distribution of the groups' responses to the OHS before (1st month) and after (3rd month) the training is shown in Table 2. Table 3 presents the distribution of the groups' OHS total score and question-based responses before (1st month) and after (3rd month) the training. After the training, the averages of physical function, pain, and mental role in the experimental group were higher than those in the control group (P < 0.05) (Table 4).
| Variables | Control (n = 30) | Experimental (n = 30) | P; χ2 |
|---|---|---|---|
| Age | χ2 = 4.273; P = 0.233 b | ||
| 65 - 69 | 6 (20.0) | 3 (10.0) | |
| 70 - 74 | 9 (30.0) | 5 (16.7) | |
| 75 - 79 | 8 (26.7) | 15 (50.0) | |
| 80 and over | 7 (23.3) | 7 (23.3) | |
| Gender | - | ||
| Female | 17 (56.7) | 17 (56.7) | |
| Male | 13 (43.3) | 13 (43.3) | |
| Education | χ2 = 0.128; P = 0.938 c | ||
| Illiterate | 11 (36.7) | 11 (36.7) | |
| literate | 14 (46.7) | 13 (43.3) | |
| Primary school | 5 (16.7) | 6 (20.0) | |
| Marital status | χ2 = 0.081; P = 0.961 b | ||
| Married | 11 (36.7) | 12 (40.0) | |
| Single | 5 (16.7) | 5 (16.7) | |
| Widow | 14 (46.7) | 13 (43.3) | |
| Working status | χ2 = 3.774; P = 0.047 b | ||
| Yes | 6 (20.0) | 13 (43.3) | |
| No | 24 (80.0) | 17 (56.7) | |
| Income status | χ2 = 3.826; P = 0.148 c | ||
| Income less than expenses | 11 (36.7) | 5 (16.7) | |
| Income equals expenditure | 13 (43.3) | 20 (66.7) | |
| Income more than expenditure | 6 (20.0) | 5 (16.7) | |
| Shared life person(s) | χ2 = 1.270; P = 0.199 b | ||
| Family | 19 (63.3) | 23 (76.7) | |
| Retirement home and single | 11 (36.7) | 7 (23.3) | |
| Additional disease | χ2 = 0.073; P = 0.50 b | ||
| Yes | 19 (63.3) | 20 (66.7) | |
| No | 11 (36.7) | 10 (33.3) | |
| Previous hip fracture surgery | χ2 = 1.763; P = 0.144 b | ||
| Yes | 14 (46.7) | 9 (30.0) | |
| No | 16 (53.3) | 21 (70.0) |
a Values are expressed as No (%).
b Pearson’s chi-square test.
c Fisher’s exact test.
| Variables | Control | Experimental | Text Values |
|---|---|---|---|
| Hip pain | |||
| 1st month | χ2 = 11.407; P = 0.003 | ||
| Mild | 0 (0.0) | 6 (20.0) | |
| Moderate | 11 (36.7) | 16 (53.3) | |
| Severe | 19 (63.3) | 8 (26.7) | |
| 3rd month | χ2=19.576; P = 0.000 | ||
| Very mild | 0 (0.0.) | 7 (23.3) | |
| Mild | 7 (23.3) | 15 (50.0) | |
| Moderate | 16 (53.3) | 8 (26.7) | |
| Severe | 7 (23.3) | 0 (0.0) | |
| Washing | |||
| 1st month | χ2 = 0.326; P = 0.850 | ||
| Moderate trouble | 4 (13.3) | 3 (10.0) | |
| Extreme difficulty | 13 (43.3) | 15 (50.0) | |
| Impossible to do | 13 (43.3.) | 12 (40.0) | |
| 3rd month | χ2 = 37.842; P = 0.000 | ||
| Very little trouble | 0 (0.0) | 13 (43.3) | |
| Moderate trouble | 5 (16.7) | 15 (50.0) | |
| Extreme difficulty | 17 (56.7) | 2 (6.7) | |
| Impossible to do | 8 (26.7) | 0 (0.0) | |
| Public transport | |||
| 1st month | χ2 = 0.601; P = 0.303 | ||
| Extreme difficulty | 14 (46.7) | 17 (56.7) | |
| Impossible to do | 16 (53.3) | 13 (43.3) | |
| 3rd month | χ2 = 39.636; P = 0.000 | ||
| With little trouble | 0 (0.0) | 16 (53.3) | |
| Moderate trouble | 8 (26.7) | 14 (46.7) | |
| Extreme difficulty | 16 (53.3) | 0 (0.0) | |
| Impossible to do | 6 (20.0) | 0 (0.0) | |
| Wearing socks | |||
| 1st month | χ2 = 1.792; P = 0.408 | ||
| With moderate difficulty | 1 (3.3) | 3 (10.0) | |
| With extreme difficulty | 15 (50.0) | 17 (56.7) | |
| Not impossible | 14 (46.7) | 10 (33.3) | |
| 3rd month | χ2 = 39.429; P = 0.000 | ||
| With little difficulty | 0 (0.0) | 8 (26.7) | |
| With moderate difficulty | 4 (13.3) | 20 (66.7) | |
| With extreme difficulty | 19 (63.3) | 2 (6.7) | |
| Not impossible | 7 (23.3) | 0 (0.0) | |
| Household shopping | |||
| 1st month | χ2 = 1.181; P = 0.554 | ||
| With moderate difficulty | 6 (20.0) | 3 (10.0) | |
| With extreme difficulty | 14 (46.7) | 16 (53.3) | |
| Not impossible | 10 (33.3) | 11 (36.7) | |
| 3rd month | χ2 = 38.222; P = 0.000 | ||
| With little difficulty | 0 (0.0) | 11 (36.7) | |
| With moderate difficulty | 6 (20.0) | 18 (60.0) | |
| With extreme difficulty | 17 (56.7) | 1 (3.3) | |
| Not impossible | 7 (23.3) | 0 (0.0) | |
| Walking | |||
| 1st month | χ2 = 9.291; P = 0.026 | ||
| 16 - 30 mins | 3 (10.0) | 4 (13.3) | |
| 5 - 15 mins | 8 (26.7) | 10 (33.3) | |
| Around the house only | 11 (36.7) | 16 (53.3) | |
| Not at all | 8 (26.7) | 0 (0.0) | |
| 3rd month | χ2 = 8.953; P = 0.030 | ||
| 16 - 30 mins | 3 (10.0) | 11 (36.7) | |
| 5 - 15 mins | 10 (33.3) | 12 (40.0) | |
| Around the house only | 14 (46.7) | 6 (20.0) | |
| Not at all | 3 (10.0) | 1 (3.3) | |
| Flat of stairs | |||
| 1st month | χ2 = 3.606; P = 0.165 | ||
| With moderate difficulty | 9 (30.0) | 7 (23.3) | |
| With extreme difficulty | 11 (36.7) | 18 (60.0) | |
| Not impossible | 10 (33.3) | 5 (16.7) | |
| 3rd month | χ2 = 41.800; P = 0.000 | ||
| Yes, easily | 0 (0.0) | 5 (16.7) | |
| With little difficulty | 0 (0.0) | 18 (60.0) | |
| With moderate difficulty | 13 (43.3) | 7 (23.3) | |
| With extreme difficulty | 17 (56.7) | 0 (0.0) | |
| Standup from a chair | |||
| 1st month | χ2 = 1.927; P = 0.382 | ||
| Moderately painful | 4 (13.3) | 5 (16.7) | |
| Very painful | 14 (46.7) | 18 (60.0) | |
| Unbearable | 12 (40.0) | 7 (23.3) | |
| 3rd month | χ2 = 29.032; P = 0.000 | ||
| Slightly painful | 0 (0.0) | 15 (50.0) | |
| Moderately painful | 16 (53.3) | 15 (50.0) | |
| Very painful | 14 (46.7) | 0 (0.0) | |
| Limping | |||
| 1st month | χ2 = 5.573; P = 0.062 | ||
| Often not just at first | 0 (0.0) | 5 (16.7) | |
| Most of the time | 17 (56.7) | 13 (43.3) | |
| All of the time | 13 (43.3) | 12 (40.0) | |
| 3rd month | χ2 = 43.579; P = 0.000 | ||
| Rarely/never | 0 (0.0) | 3 (10.0) | |
| Sometimes or just at first | 0 (0.0) | 14 (46.7) | |
| Often not just at first | 6 (20.0) | 13 (43.3) | |
| Most of the time | 15 (50.0) | 0 (0.0) | |
| All of the time | 9 (30.0) | 0 (0.0) | |
| Sudden, severe pain | |||
| 1st month | χ2 = 0.268; P = 0.398 | ||
| Most days | 13 (43.3) | 15 (50.0) | |
| Every day | 17 (56.7) | 15 (50.0) | |
| 3rd month | χ2 = 49.714; P = 0.000 | ||
| Only 1 or 2 days | 0 (0.0) | 10 (33.3) | |
| Some days | 0 (0.0) | 17 (56.7) | |
| Most days | 18 (60.0) | 3 (10.0) | |
| Every day | 12 (40.0) | 0 (0.0) | |
| Usual work | |||
| 1st month | χ2 = 9.333; P = 0.009 | ||
| Moderately | 0 (0.0) | 6 (20.0) | |
| Greatly | 12 (40.0) | 15 (50.0) | |
| Totally | 18 (60.0) | 9 (30.0) | |
| 3rd month | χ2 = 26.275; P = 0.000 | ||
| A little bit | 0 (0.0) | 1 (3.3) | |
| Moderately | 0 (0.0) | 15 (50.0) | |
| Greatly | 15 (50.0) | 12 (40.0) | |
| Totally | 15 (50.0) | 2 (6.7) | |
| Hip pain in bed | |||
| 1st month | χ2 = 10.982; P = 0.004 | ||
| Some nights | 0 (0.0) | 7 (23.3) | |
| Most nights | 15 (50.0) | 17 (56.7) | |
| Every night | 15 (50.0) | 6 (20.0) | |
| 3rd month | χ2 = 38.667; P = 0.000 | ||
| Only 1 or 2 nights | 0 (0.0) | 14 (46.7) | |
| Some nights | 8 (26.7) | 16 (53.3) |
a Values are expressed as No (%).
b Man Whitney U test.
| Variables | Control | Experimental | P-Value |
|---|---|---|---|
| Hip pain | |||
| 1st month | 4.63 ± 0.490 | 4.07 ± 0.69 | 0.001 |
| 3rd month | 4 ± 0.69 | 3.03 ± 0.71 | 0.000 |
| Wilcoxon Z/P | -3.64/0.000 | -3.77/0.000 | |
| Washing | |||
| 1st month | 4.30 ± 0.70 | 4.30 ± 0.65 | 0.942 |
| 3rd month | 4.10 ± 0.66 | 2.63 ± 0.61 | 0.000 |
| Wilcoxon Z/P | -1.269/0.20 | -4.62/0.000 | |
| Public transport | |||
| 1st month | 4.53 ± 0.50 | 4.43 ± 0.50 | 0.442 |
| 3rd month | 3.93 ± 0.69 | 2.47 ± 0.50 | 0.000 |
| Wilcoxon Z/P | -3.175/0.001 | -4.85/0.000 | |
| Wearing socks | |||
| 1st month | 4.43 ± 0.56 | 4.23 ± 0.62 | 0.217 |
| 3rd month | 4.10 ± 0.60 | 2.80 ± 0.55 | 0.000 |
| Wilcoxon Z/P | -2.23/0.025 | -4.65/0.000 | |
| Household shopping | |||
| 1st month | 4.13 ± 0.73 | 4.27 ± 0.64 | 0.495 |
| 3rd month | 4.03 ± 0.66 | 2.67 ± 0.54 | 0.000 |
| Wilcoxon Z/P | -0.60/0.54 | -4.82/0.000 | |
| Walking | |||
| 1st month | 3.80 ± 0.96 | 3.40 ± 0.72 | 0.083 |
| 3rd month | 3.57 ± 0.81 | 2.90 ± 0.84 | 0.003 |
| Wilcoxon Z/P | -1.09/0.27 | -2.41/0.016 | |
| Flat of stairs | |||
| 1st month | 4.03 ± 0.80 | 3.93 ± 0.64 | 0.603 |
| 3rd month | 3.57 ± 0.50 | 2.07 ± 0.64 | 0.000 |
| Wilcoxon Z/P | -2.562/0.010 | -4.769/0.000 | |
| Stand up from a chair | |||
| 1st month | 4.27 ± 0.691 | 4.07 ± 0.64 | 0.225 |
| 3rd month | 3.47 ± 0.507 | 2.50 ± 0.50 | 0.000 |
| Wilcoxon Z/P | -3.96/0.000 | -4.815/0.000 | |
| Limping | |||
| 1st month | 4.43 ± 0.504 | 4.23 ± 0.72 | 0.343 |
| 3rd month | 4.10 ± 0.71 | 2.33 ± 0.66 | 0.000 |
| Wilcoxon Z/P | -2.041/0.041 | -4.848/0.000 | |
| Sudden/severe pain | |||
| 1st month | 4.57 ± 0.50 | 4.5 ± 0.5 | 0.608 |
| 3rd month | 4.40 ± 0.49 | 2.77 ± 0.62 | 0.000 |
| Wilcoxon Z/P | -1.213/0.22 | -4.86/0.000 | |
| Usual work | |||
| 1st month | 4.6 ± 0.49 | 4.1 ± 0.71 | 0.005 |
| 3rd month | 4.5 ± 0.50 | 3.5 ± 0.68 | 0.000 |
| Wilcoxon Z/P | -0.77/0.43 | -2.99/0.003 | |
| Hip pain in bed | |||
| 1st month | 4.5 ± 0.50 | 3.97 ± 0.669 | 0.002 |
| 3rd month | 3.9 ± 0.66 | 2.53 ± 0.507 | 0.000 |
| Wilcoxon Z/P | -3.38/ 0.001 | -4.696/0.000 | |
| OHS toplam | |||
| 1st month | 52.23 ± 4.38 | 49.5 ± 3.17 | 0.014 |
| 3rd month | 47.56 ± 3.1 | 32.2 ± 2.52 | 0.000 |
| Wilcoxon Z/P | -4.23/0.000 | -4.786/0.000 |
Abbreviation: OHS, Oxford Hip Score.
a Values are expressed as mean ± SD.
| Variables | Control | Experimental | P-Value |
|---|---|---|---|
| Physical function | |||
| 1st month | 36.50 ± 15.54 | 35.83 ± 11.52 | 0.89 |
| 3rd month | 40.33 ± 14.32 | 66.83 ± 11.48 | 0.000 |
| Wilcoxon Z/P | -1.147/0.25 | -4.74/0.000 | |
| Physical role | |||
| 1st month | 12.5 ± 12.7 | 35 ± 26.74 | 0.000 |
| 3rd month | 50 ± 30.79 | 71.6 ± 24.33 | 0.004 |
| Wilcoxon Z/P | -3.94/0.000 | -4.037/0.000 | |
| Pain | |||
| 1st month | 21.96 ± 15.74 | 19.26 ± 9.91 | 0.471 |
| 3rd month | 38.76 ± 12.51 | 54.9 ± 10.49 | 0.000 |
| Wilcoxon Z/P | -3.601/0.000 | -4.713/0.000 | |
| General health | |||
| 1st month | 32.76 ± 6.64 | 36.16 ± 5.03 | 0.034 |
| 3rd month | 48.2 ± 7.08 | 65 ± 5.01 | 0.000 |
| Wilcoxon Z/P | -4.79/0.000 | -4.82/0.000 | |
| Vitality | |||
| 1st month | 25 ± 8.3 | 26.16 ± 7.15 | 0.67 |
| 3rd month | 47.83 ± 7.15 | 50.33 ± 6.94 | 0.26 |
| Wilcoxon Z/P | -4.72/0.000 | -4.81/0.000 | |
| Social function | |||
| 1st month | 26.66 ± 11.24 | 22.91 ± 12.74 | 0.20 |
| 3rd month | 50.41 ± 11.12 | 56.66 ± 10.24 | 0.06 |
| Wilcoxon Z/P | -4.475/0.000 | -4.820/0.000 | |
| Role emotional | |||
| 1st month | 33.33 ± 31.56 | 42.22 ± 38.09 | 0.38 |
| 3rd month | 40 ± 28.23 | 68.88 ± 23.05 | 0.000 |
| Wilcoxon Z/P | -1.06/0.28 | -3.12/0.002 | |
| Mental health | |||
| 1st month | 49.06 ± 8.39 | 44.8 ± 8.75 | 0.055 |
| 3rd month | 51.6 ± 8.36 | 49.73 ± 5.32 | 0.39 |
| Wilcoxon Z/P | -1.35/0.17 | -2.26/0.024 | |
| PCS | |||
| 1st month | 27.51 ± 4.82 | 29.82 ± 4.26 | 0.032 |
| 3rd month | 35.83 ± 4.35 | 45.8 ± 4.01 | 0.000 |
| Wilcoxon Z/P | -4.24/0.000 | -4.78/0.000 | |
| MCS | |||
| 1st month | 35.68 ± 5.26 | 34.71 ± 5.34 | 0.47 |
| 3rd month | 40.10 ± 4.3 | 40.18 ± 3.82 | 0.85 |
| Wilcoxon Z/P | -3.38/0.001 | -3.73/0.000 |
Abbreviations: PCS, physical component summary; MCS, mental component summary.
a Values are expressed as mean ± SD.
Before and after the training, patients in the experimental group had higher physical role, general health perception, and physical component summary (PCS) averages than those in the control group. The increase in physical role, pain, general health perception, vitality, social function, PCS, and mental component summary (MCS) levels in the control group after the training was statistically significant (P < 0.05) (Table 4). The increase in physical function, physical role, pain, general health perception, vitality, social function, mental role, mental health, PCS, and MCS levels in the experimental group after the training was statistically significant (P < 0.05) (Table 4).
5. Discussion
Hip fractures in the geriatric population represent a significant public health concern (14). This study observed a higher prevalence of female patients. Raichandani et al. reported osteoporosis in 65% of females and 50% of males with hip fractures. The higher prevalence in females is attributed to increased bone loss during peri-menopause and post-menopause (15). As hip fracture surgeries are often performed at older ages, it is common for individuals in this age group to be married, with many being widowed. Marriage is considered a factor that facilitates and supports home care for individuals undergoing hip fracture surgery (16). The study observed that most individuals had lost their spouses and generally lived with their children and family members. Acute and chronic diseases, which increase with advancing age, lead to long-term and multiple drug use (17).
In the third month, the proportion of those experiencing severe pain in the control group decreased to 23.3%, whereas no one in the experimental group reported severe pain. Analysis of the OHS revealed that mean scores in the third month decreased in both groups compared to the first month. A study on hip replacement indicated that pain began to decrease in the third month, with optimal results observed in the sixth month (18). In the third month, the rate of patients unable to walk at all in the control group was 10%, which decreased to 3.3% in the experimental group. The OHS analysis showed that mean night pain scores in both the control and experimental groups decreased in the third month compared to the first month. Data collected from patients admitted to four New York city hospitals with hip fractures suggest that improved pain control can reduce the length of stay and enhance long-term functional outcomes (19).
Hip fracture is a critical condition that adversely affects the quality of life, particularly in older patients, where lost functionality due to physiological disorders and related problems, including disorders related to physiological and mental qualities, are observed (20). Partial improvements have been demonstrated in the physical and psychosocial functions of patients three to four months post-fracture (21). The mean physical role scores of patients in the experimental group, both before and after training, were higher than those of the control group. Adachi et al. conducted similar studies and reported that hip fractures significantly decrease all dimensions of quality of life, particularly physical and social functions (22). The Functional Capacity Scale (FCS) averages of patients in the experimental group, both before and after training, were higher than those of the control group. A study indicated that the quality of life for older patients with hip fractures was severely impaired one month post-fracture, with partial improvement by the fourth month (23).
In this study, the mean post-training pain levels of patients in the experimental group were higher than those in the control group. Poorly managed postoperative pain is associated with delayed ambulation and pulmonary complications (24). The mean mental role scores of patients in the experimental group, both before and after training, were higher than those of the control group. The lack of significant differences, despite nursing care provided at home after an operation that caused more distress to patients, suggests that patients should receive mental support and nurses should be made aware of this issue (25). Su et al. demonstrated that a nurse-led care program improved health-related quality of life in older adults following hip fracture surgery (26). Similarly, Banappagoudar et al. showed that nursing intervention was beneficial in improving physical and psychosocial functioning in elderly patients with hip fractures (27).
When responses to the OHS were examined, a significant decrease was observed in scores for hip pain, bathing, transportation, wearing socks, shopping, walking distance, climbing stairs, pain when rising from a chair, limping while walking, sudden/serious pain, affecting general work, and pain in bed at night in the experimental group compared to the control group. Additionally, OHS analysis revealed that the mean scores for hip pain at the first month, the variable of general work being affected, and the total OHS score were higher in the control group than in the experimental group. In the experimental group, the mean total OHS score and responses to questions in the third month decreased significantly compared to the control group.
The small sample size is a limitation of this study. Furthermore, the number and duration of education provided to patients could not be monitored for at least six months.
5.1. Conclusions
These results indicate that the training program developed for patients made significant contributions to their healing process. Based on these findings, to reduce the frequency of hospitalization for patients undergoing hip fracture surgery, education programs for the patient and family should be initiated upon hospital admission, and discharge education should be comprehensively planned and implemented.