1. Background
After abdominal surgery, patients may experience nausea, vomiting, decreased bowel movements, delayed gas and stool excretion (1), and ileus (2). Early mobilization accelerates the healing process by mitigating the negative effects of surgical stress and immobility (3). It plays a crucial role in enhancing intestinal motility, ensuring the return of normal intestinal function (4), and preventing the development of ileus (5). Other obstacles to mobilization include the excessive workload of nurses, lack of knowledge, severity of the disease, developing complications, and the presence of catheters and drains (6). The enhanced recovery after surgery (ERAS) protocol, developed by the ERAS society, is one of the evidence-based practices (7). Mobilization is a key component of the ERAS protocol (6) and is effective in facilitating early discharge, restoring activities of daily living (8), and reducing pain (9). The ERAS protocol recommends that patients spend at least 2 hours out of bed on the day of surgery and 6 hours on subsequent days (10). To achieve this, it is advised that patients be informed about early mobilization during the preoperative period, a patient-specific care plan be developed, daily mobilization goals be set, and a patient diary be maintained for out-of-bed activities (11). In a study conducted by Abdo and Mamdouh, it was reported that patients who adhered to the ERAS protocol and were more mobilized developed fewer complications, experienced less pain, and required less analgesia (12).
2. Objectives
Based on this information, this study aimed to evaluate the effects of mobilization time and duration after laparoscopic cholecystectomy on patient pain and bowel motility, and to highlight the importance of this issue.
3. Methods
3.1. Study Design
The study is descriptive and cross-sectional.
3.2. Participants
The study population comprised all patients (n = 131) who underwent elective laparoscopic cholecystectomy at the general surgery clinic between November 2022 and March 2023. Patients who met the exclusion criteria, including those with inflammatory bowel disease, irritable bowel syndrome, or chronic constipation, were excluded from the study (n = 3). The sample consisted of patients who met the specified criteria: Over 18 years of age, able to communicate verbally, with no defined psychiatric problems, and no history of substance use, who also agreed to participate in the study (n = 94).
3.3. Scales
Data were collected by the researcher in the surgical clinic where the study was conducted, using a personal information form and a Visual Analog Scale (VAS) through face-to-face interviews. The VAS typically consists of a 10 cm long horizontal line, with the left end labeled "no pain" (0) and the right end labeled "unbearable pain" (10). The distance from the marked point to the left baseline is measured, yielding a numerical value between 0 and 10.
3.4. Data Collection
The concept of early mobilization is defined as getting up and walking as soon as possible after illness and surgery (13). No interventions were made regarding the initial mobilization times in the study. Patients' pain levels were assessed using the VAS at 8, 24, and 48 hours post-surgery (14). Patients were also asked about the timing of their first gas evacuation and first defecation, which were recorded. The personal information form consists of 15 questions designed to gather the patient's demographic data (15). The VAS was developed to determine patients' pain levels (16). The validity and reliability of the VAS were established by Kumar et al. (14).
3.5. Data Analysis
Statistical analyses were conducted using the SPSS version 25.0 software. The suitability of the variables for normal distribution was assessed using the Kolmogorov-Smirnov test. Descriptive statistics, including percentages, arithmetic mean, and standard deviation, were utilized to analyze sociodemographic characteristics. Relationships between quantitative variables were examined using Pearson correlation analysis. The correlation coefficient was interpreted as follows: A very strong correlation between 0.80 and 1.0; a strong correlation between 0.60 and 0.79; a moderate correlation between 0.40 and 0.59; a weak correlation between 0.20 and 0.39; and a very weak correlation between 0 and 0.19 (17). The results were evaluated with a 95% confidence interval, and significance was determined at P < 0.05.
3.6. Ethical Considerations
The study protocol was approved by the Institutional Non-interventional Clinical Research Ethics Committee (No. 07.10.2022/126). The study was conducted in accordance with the principles of the Declaration of Helsinki and complies with the STROBE guidelines. Verbal and written consent was obtained from patients undergoing elective laparoscopic cholecystectomy to ensure their participation in the study.
4. Results
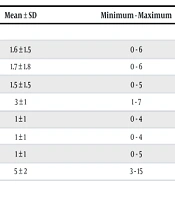
It was found that 62.8% of the participants were female, with a mean age of 47.4 ± 14.1 years. Of the participants, 53.2% had previous surgical experience, 63.9% had a chronic disease, and 48.9% used opioids during the perioperative period. The mean time to first liquid intake was 13.2 ± 9.1 hours, while the mean time to first solid food intake was 24.1 ± 12.4 hours. The mean time to first mobilization was 9.4 ± 5.3 hours, with mean mobilization times of 5.3 ± 3.4 minutes on day 0 and 29.4 ± 22.3 minutes on day 1. The mean time to first flatus was 15.3 ± 9.2 hours, the mean time to first defecation was 20.4 ± 16.3 hours, and the mean hospital stay was 2.1 ± 2.2 days (Table 1). The mean VAS score was 1.6 ± 1.5 at the 8th hour and 1.5 ± 1.5 at the 24th hour. The mean number of paracetamol vials used was 3 ± 1, diclofenac ampoules 1 ± 1, opioid ampoules 1 ± 1, hyoscine-N-butylbromide ampoules 1 ± 1, and the mean total number of analgesics used was 5 ± 2 (Table 2). There was a moderate, positive, and significant correlation between the time of first mobilization and the time of first passing gas (r = 0.521, P < 0.05). Similarly, a moderate, positive, and significant relationship was observed between the time of first mobilization and the time of first defecation (r = 0.503, P < 0.05). There was also a moderate, positive, and significant correlation between the time of first mobilization and pain levels at the 8th and 24th hours (r = 0.510, P < 0.05; r = 0.504, P < 0.05, respectively). Furthermore, a moderate, positive, and significant correlation was found between the time of first mobilization and the number of analgesics used (r = 0.574, P < 0.05) (Table 3).
| Variables | Values a |
|---|---|
| Gender | |
| Female | 59 (62.8) |
| Male | 35 (37.2) |
| Previous surgical experience | |
| Yes | 50 (53.2) |
| No | 44 (46.8) |
| Concomitant disease | |
| Yes | 60 (63.8) |
| No | 34 (36.2) |
| Opioid Use | |
| Yes | 46 (48.9) |
| No | 48 (51.1) |
| Age | 46.4 ± 13.6 (21 - 79) |
| Duration of surgery (min) | 104.2 ± 33.3 (45 - 210) |
| Post-op first fluid intake time (h) | 13.2 ± 9.1 (5 - 72) |
| Post-op first solid intake time (h) | 24.1 ± 12.4 (10 - 84) |
| Time to first mobilization (h) | 9,4 ± 5.3 (5 - 24) |
| Postoperative day 0 total mobilization time (min) | 5.3 ± 3.4 (2 - 30) |
| Total mobilization time on the first postoperative day (min) | 29.4 ± 22.3 (2 - 120) |
| Time to first gas release (h) | 15.3 ± 9.2 (1 - 70) |
| Time to first defecation (h) | 20.4 ± 16.3 (1 - 70) |
| Time until discharge (d) | 2.1 ± 2.2 (1 - 9) |
Analysis of Demographic Data of Participants (n = 94)
| Variables | Mean ± SD | Minimum - Maximum |
|---|---|---|
| VAS score average (h) | ||
| 4 | 1.6 ± 1.5 | 0 - 6 |
| 8 | 1.7 ± 1.8 | 0 - 6 |
| 24 | 1.5 ± 1.5 | 0 - 5 |
| Paracetamol vial (1000 mg) | 3 ± 1 | 1 - 7 |
| Diclofenac ampoule (75 mg) | 1 ± 1 | 0 - 4 |
| Opioid ampoule (10 mg) | 1 ± 1 | 0 - 4 |
| Hyoscine-N-butyl bromide ampoule (20 mg) | 1 ± 1 | 0 - 5 |
| Total number of analgesics used | 5 ± 2 | 3 - 15 |
Analysis of Participants' Postoperative Pain Levels and Analgesic Consumption
| Variables | Pearson r | P-Value a |
|---|---|---|
| Time for first flatus | 0.521 | 0.01 |
| Time of first defecation | 0.503 | 0.01 |
| VAS | ||
| 8th hour | 0.510 | 0.01 |
| 24th hour | 0.504 | 0.01 |
| Number of analgesics used | 0.574 | 0.01 |
Analysis of the Relationship Between Participants' First Mobilization Times and First Flatulence Times, First Defecation Times, Pain Levels, and Number of Analgesics Used
5. Discussion
Early mobilization may shorten the length of hospital stay by enabling patients to regain normal function shortly after surgery (18). Mobilization interventions following abdominal surgery support the normalization of bowel function and reduce the severity of abdominal distension (19). While the timing of early mobilization is uncertain, recommendations suggest taking a few steps at the edge of the bed within the first 6 to 8 hours post-surgery (20). Postoperative mobilization should be initiated as soon as possible, taking into account the patient's sensory, mental, physical, and functional performance, as well as vital signs (21). In this study, the average time to postoperative mobilization was consistent with the literature, although it was observed that mobilization could be delayed up to 24 hours in some patients. Despite the ERAS protocol's recommendation of staying out of bed for 2 hours on the day of surgery and 6 hours on subsequent days (10), compliance with mobilization goals may be low (22). In this study, patients' mobilization times on postoperative days 0 and 1 were shorter than recommended, indicating low compliance. It was hypothesized that the administration of opioids to 48.9% of patients during the perioperative period negatively impacted their mobilization. Literature reports suggest that opioid-related adverse events, such as nausea, vomiting, dizziness, and excessive sedation, may reduce postoperative mobilization (23, 24).
One of the most critical indicators that gastrointestinal motility is not at the desired level after abdominal surgery is the absence of postoperative gas output (25). Mobilization interventions after abdominal surgeries accelerate gastrointestinal motility, support the normalization of bowel functions, and reduce the severity of abdominal distension (19). Studies have reported that patients who are mobilized early and in a planned manner have significantly shorter times to first gas output and defecation compared to control groups (18, 26). In this study, the mean postoperative times for first gas output and defecation were longer than those reported in the literature, suggesting that high opioid use and delayed initial mobilization may have affected the results. It is believed that early planning of the first postoperative mobilization period could influence the times for first gas output and defecation. If postoperative pain management is not successful, the mobilization and recovery process may be prolonged, increasing opioid use and related side effects, and potentially delaying discharge (27). It is recommended that analgesics be administered at regular intervals, especially during the first 48 hours when pain is acute, and as needed thereafter (28).
Early mobilization plays a crucial role in pain management as a nonpharmacological practice (29). Studies indicate that early mobilization reduces patient pain after laparoscopic cholecystectomy (30). Early mobilization accelerates the healing process by increasing blood circulation, reducing inflammation (31), and encouraging the release of endorphins, which are natural painkillers. It prevents muscle stiffness caused by inactivity and the associated pain (13). This approach protects against drug side effects and accelerates the recovery process, reducing the risk of opioid addiction (11). In this study, due to early discharge, 48-hour pain assessment data could not be recorded. It was concluded that as the initial mobilization time decreased, pain levels and analgesic consumption also decreased. It is believed that providing early mobilization according to the patient's clinical condition will positively affect the recovery process by reducing analgesic consumption.
5.1. Conclusions
The study found that early mobilization after laparoscopic cholecystectomy surgery positively impacts patient outcomes by reducing the time for gas and bowel movements, decreasing pain levels, and minimizing the need for analgesics. These findings underscore the importance of early and planned mobilization to prevent factors that may negatively affect patient comfort and to reduce the risk of complications in the postoperative period. In this context, organizing planned educational programs for nurses and conducting more comprehensive studies that thoroughly examine the effects of early mobilization on patient outcomes could contribute to enriching the literature and improving clinical practices. Encouraging multidisciplinary approaches to validate the benefits of early and planned mobilization across a broader patient group may further enhance its positive impact on both individual patient care and general health systems.
5.2. Limitations
The most significant limitation of this study is that it was conducted in a single center, and potential confounding factors such as age, gender, comorbidities, and medication use were not considered. Additionally, since the patients were discharged on the first day, the planned 48-hour pain assessments could not be conducted.