1. Introduction
Bronchogenic cysts are congenital cystic lesions that arise from a developmental anomaly during the embryonic stage of bronchial budding. These cysts are typically located in the mediastinum and, when situated adjacent to the trachea or major airways, may cause clinical symptoms due to airway compression. Common presenting symptoms include dyspnea, inspiratory stridor, and recurrent respiratory tract infections (1). In symptomatic patients or in lesions with a potential risk of complications, surgical excision is recommended for both definitive diagnosis and curative treatment (2).
In recent years, open surgical techniques such as thoracotomy have increasingly been replaced by less invasive surgical approaches that improve patient comfort. In this context, uniportal video-assisted thoracoscopic surgery (u-VATS) has emerged as a favorable option due to its minimal tissue trauma, reduced postoperative pain, shorter hospital stays, and superior cosmetic outcomes (2).
However, the risk of tracheal injury increases during the resection of bronchogenic cysts located adjacent to the trachea, particularly in the presence of inflammation or adhesions (3, 4). Although such complications are rare, they can be successfully managed using a u-VATS approach when performed by experienced surgical teams (5). The feasibility of minimally invasive surgery in complex scenarios such as these highlights the dual diagnostic and therapeutic value of the u-VATS technique (5). In this report, we present a rare case of a tracheal injury secondary to a bronchogenic cyst adjacent to the trachea, which was successfully repaired using the u-VATS approach.
2. Case Presentation
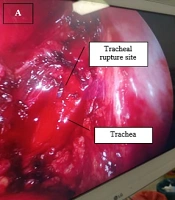
A 21-year-old female patient with no significant past medical history presented to our outpatient clinic with a six-month history of persistent coughing episodes and intermittent dyspnea. No abnormal findings were detected in the biochemical blood tests. Physical examination revealed no notable pathological findings. However, a posteroanterior chest radiograph showed a homogeneous, radio-opaque shadow in the upper mediastinum (Figure 1A). Non-contrast thoracic computed tomography (CT) was performed for further evaluation, which revealed a well-defined, soft tissue density lesion measuring approximately 3.8 × 5.8 × 4.4 cm in the upper mediastinum, adjacent to the trachea (Figure 1B). To assess the degree of invasion and the relationship to adjacent structures, contrast-enhanced thoracic magnetic resonance imaging (MRI) was performed. The MRI confirmed a non-enhancing, well-circumscribed lesion located in the right paratracheal area, exerting mild lateral compression on the trachea (Figure 1C).
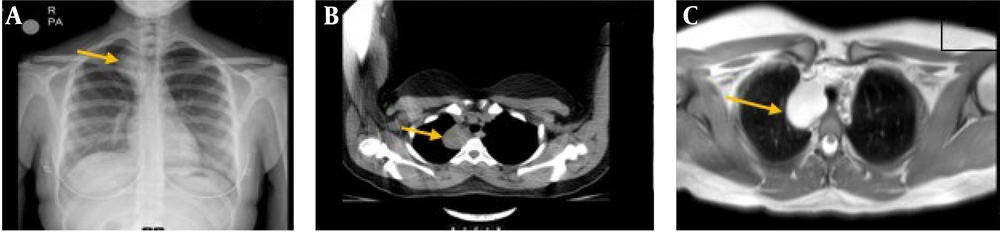
Due to the lesion’s benign radiologic appearance and the presence of symptoms, u-VATS was planned for both diagnostic and therapeutic purposes. During thoracoscopic surgery performed via a single incision, the lesion was found to be tightly adherent to the trachea (Figure 2A - C).
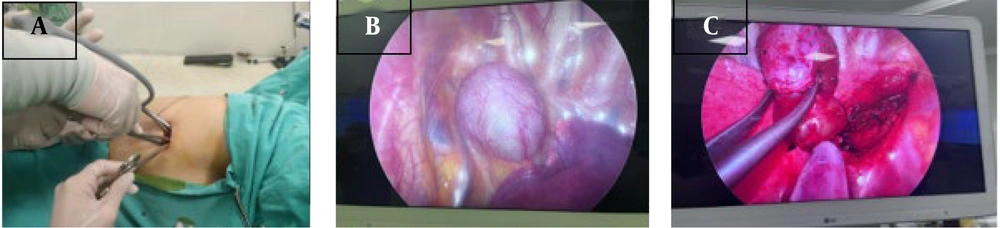
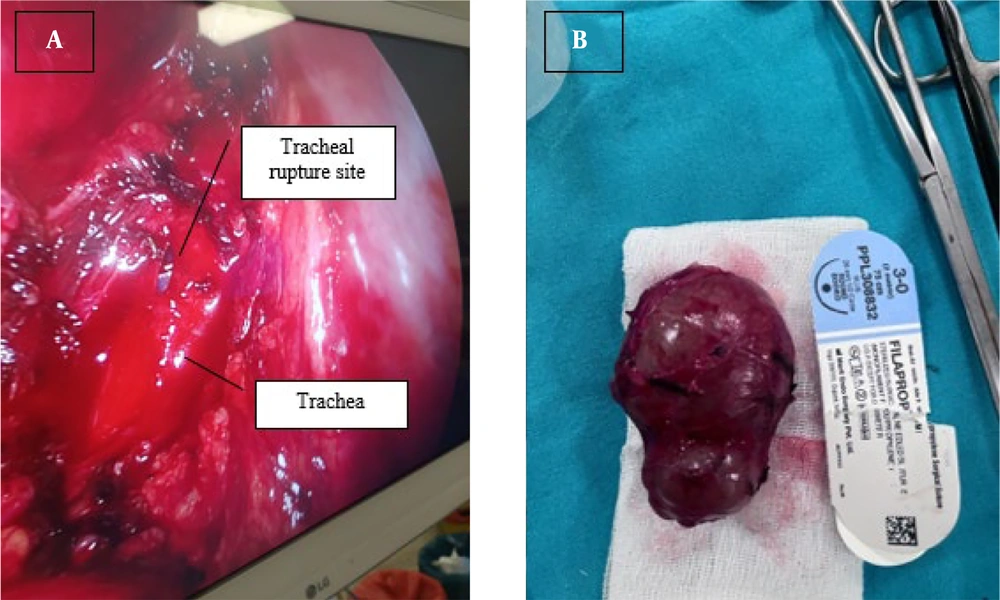
During careful dissection of these adhesions, an approximately 1 cm tracheal rupture occurred. Without converting to open surgery, the rupture site was successfully repaired with primary suturing via the same u-VATS access (Figure 3A). A primary repair was performed using interrupted 3/0 polypropylene (Prolene®) sutures. The location of the injury allowed for adequate visualization and access without the need for advanced airway manipulation. As the lesion was situated proximally, no difficulties were encountered in terms of endotracheal tube placement or intraoperative anesthetic management. Following tracheal repair, the cyst was completely excised, and the procedure was concluded thoracoscopically (Figure 3B).
In the postoperative period, the patient experienced no complications. She tolerated oral intake, exhibited no respiratory distress, and maintained stable vital signs. She was discharged uneventfully on postoperative day three. Histopathological examination confirmed the lesion as a bronchogenic cyst.
3. Discussion
Bronchogenic cysts are congenital cystic lesions that arise due to anomalies in the development of the tracheobronchial tree during the embryonic period, and they are most commonly located in the mediastinal region. Although these cysts are often asymptomatic, they may become clinically apparent when located near critical anatomical structures such as the airway or esophagus (4). Bronchogenic cysts adjacent to the trachea can cause symptoms such as dyspnea, stridor, recurrent pulmonary infections, and, in rare cases, tracheal deformation due to airway compression. Because of their anatomical proximity and frequent adhesion to surrounding tissues, cysts in this region pose technical challenges during surgical excision (3).
Surgical excision remains the gold standard for the treatment of bronchogenic cysts, and in recent years, there has been an increasing preference for minimally invasive techniques (5). Among these, u-VATS offers several advantages over traditional thoracotomy and multi-port VATS approaches, including reduced postoperative pain, lower complication rates, shorter hospital stays, better cosmetic outcomes, and earlier mobilization. Moreover, u-VATS has also been shown to be a safe and reliable technique even in complex surgical scenarios (6, 7).
Studies have demonstrated that u-VATS is both a safe and effective approach for the excision of bronchogenic cysts. When applied to mediastinal lesions, u-VATS has been associated with low morbidity rates, and the majority of resulting complications have been successfully managed using conservative methods (8). The same studies have also reported significantly shorter operative times and drainage durations. Moreover, even in cases where bronchogenic cysts are located in close proximity to high-risk anatomical structures such as the trachea, successful excision using the u-VATS technique has been documented when performed by experienced surgeons (9).
The primary surgical risk in bronchogenic cysts located adjacent to the trachea is the development of tracheal injury during dissection. This complication becomes particularly inevitable when dense adhesions secondary to inflammation are present. However, cases in the literature have shown that tracheal injuries occurring during u-VATS can be successfully repaired with primary suturing, without the need to convert to open thoracotomy (10, 11). Several studies have confirmed that tracheal ruptures can be safely managed within the scope of minimally invasive surgery. This demonstrates that u-VATS is not only an excision technique but also a reliable and effective method for managing intraoperative complications.
The present case is noteworthy as it illustrates the successful excision of a bronchogenic cyst adjacent to the trachea using the u-VATS technique, along with the primary repair of an intraoperative tracheal rupture through the same minimally invasive approach. This highlights the fact that minimally invasive surgery, beyond offering cosmetic and comfort-related advantages, also serves as a robust option for addressing complex surgical complications.
3.1. Conclusions
Bronchogenic cysts can pose significant diagnostic and therapeutic challenges, particularly when located adjacent to critical structures such as the trachea. With advancements in minimally invasive surgical techniques, u-VATS has emerged as an effective and safe alternative for both diagnostic and therapeutic interventions. Proper patient selection, meticulous dissection, and techniques performed by experienced surgeons have contributed to minimizing complication rates associated with u-VATS.
This case contributes to the literature by demonstrating the successful excision of a bronchogenic cyst located adjacent to the trachea using the u-VATS technique, along with the primary repair of an intraoperative tracheal injury through the same approach. Beyond its well-recognized advantages in terms of postoperative comfort, u-VATS proves to be a robust tool in managing complex intraoperative complications. Cases such as this underscore that, in appropriately selected patients, u-VATS can achieve high success rates without the need for conversion to open surgery.