1. Background
Aging rate and elderly population are progressively increasing worldwide (1). Statistics show that after United Arab Emirates and Bahrain, Iran is the third country with respect to aging rate and 22% of the Iranian population are expected to be over 60 by 2050, while it is currently about 8% (2). As nations age, elderly people’s problems increase significantly (3).
Aging causes different physiological changes. An age-related problem is sleep disorders. Elderly people have a wide range of sleep disorders, particularly sleep onset insomnia, sleep maintenance insomnia, nighttime awakening, difficulty in returning to sleep, and early morning awakening (4). Despite the high prevalence of sleep disorders among elderly people, they are usually undiagnosed or poorly treated. Insomnia can cause different complications such as concentration and memory impairments, depression, fatigue, and dissatisfaction with quality of life (5). Poor sleep quality is the third commonest problem among elderly people, only after headache and gastrointestinal problems, and a leading cause of seeking medical advice (6).
More than 57% of elderly people report sleep disorders, while only 12% of them do not complain about such disorders (7). Sleep disorders such as sleep onset and maintenance difficulties as well as the use of sleeping medications are more common among elderly people than the youth (8). Willingness to sleep in the afternoon is common even among healthy elderly people. Daytime sleep time and subsequent nighttime sleep problems increase with age. In other words, aging causes disturbances in sleep order and pattern (9).
Inadequate sleep is a risk factor for different disorders such as obesity, type 2 diabetes mellitus, cardiovascular disease, and depression (10, 11). Sleep disorders undermine health and functioning, cause physical and psychological pains (12, 13), bring about daytime sleepiness (14), and increase the risk for drug abuse (15). Studies show that sleep quality is affected by many factors including age (12), gender (16), emotions (13), and marital status (17). Sleep alleviates fatigue and prepares individuals for daily activities (18).
The most common treatment for sleep disorders is medication therapy. However, despite their rapid-onset effects, sleeping medications are associated with different side effects and complications. Consequently, non-pharmacological therapies are increasingly used to manage sleep disorders. Although the onset of the effects of these therapies is slower than that of medications, they are safer. One of these therapies is physical exercise. Regular physical exercise brings about calmness, increases body core temperature, and thereby, can improve sleep quality (6, 19). Different mechanisms were reported for the effects of exercise on sleep. A mechanism is that exercise increases the secretion of melatonin by the pineal gland (2). Melatonin exerts its hypnotic effects through changing body core temperature (20). The amount of melatonin secretion greatly depends on gender, age, as well as exercise type, intensity, and time. Besides improving sleep quality, exercise can also reduce body weight, prevent pain, and elevate mood (21).
Walking is an appropriate physical exercise for all people. It requires no certain equipment and thus, all people from different age and gender groups can do it everywhere and every time. Studies show the significant effects of walking on people from all age groups (5, 22). For instance, a study showed that physical exercise was significantly correlated with different sleep-related parameters (23). Another study reported that walking improved sleep quality and duration by 31% and 45%, respectively. However, the results of studies into the effects of exercise on sleep among elderly people are contradictory. For instance, a study showed that both morning and evening exercises improved psychosocial functioning and sleep quality (24), while another study indicated that late nighttime exercise was more effective than other time of exercise in improving sleep quality (25). Contrarily, Passos et al. reported no significant difference between the effects of morning and evening exercises on chronic insomnia. Therefore, further studies are needed to determine the effectiveness of walking on elderly people’s sleep quality. The current study aimed at comparing the effects of morning and evening walks on nighttime sleep quality among elderly people.
2. Methods
The current 2-group randomized, crossover trial was conducted on elderly people referred to healthcare centers in Rafsanjan, Iran. Based on the results of an earlier study (26) and the formula to calculate sample sizes to compare 2 means, 18 cases were needed for each study group. Yet, the sample size was increased to 25 for each group to enhance the rigor of the study and prevent the effects of probable dropouts on the study results.
Inclusion criteria were the age of 60 or above, adequate physical strength and fitness to walk, no affliction by cardiopulmonary or mental disorders; no history of drug addiction, cigarette smoking, hypertension, and arthralgia; no history of regular physical exercise during the past 2 months; no use of sleeping medications; and a score of 5 or more for the Pittsburg sleep quality index (PSQI). Participants were excluded if they developed physical problems during the study, were unable to go walking, or had 2 consecutive or 4 intermittent absentees from the walking sessions.
A demographic questionnaire and PSQI were used to gather data. As a valid and reliable self-report tool, PSQI was developed by Buysse et al. to assess sleep quality and diagnose sleep disorders during the past 4 weeks (10). PSQI contains 9 items in 7 components as follows: subjective sleep quality: item 9; sleep latency: item 2 and part “a” of item 5; sleep duration: item 4; habitual sleep efficiency: the score of this item is calculated through dividing the hours spent asleep by the time spent in bed and multiplying the result by 100; sleep disturbances: the mean score of all parts of item 5; sleeping medication: item 6; and daytime dysfunction: items 7 and 8. Each item is scored by a 4-option Likert scale for normal, mild, moderate, and severe sleep problems. The total score of PSQI is calculated through summing up the item scores and can range from 0 to 21 (6). According to PSQI developers, PSQI scores greater than 5 are interpreted as poor sleep quality, while scores 5 and lower show good sleep quality. The Cronbach’s alpha of PSQI is 0.83 (10).
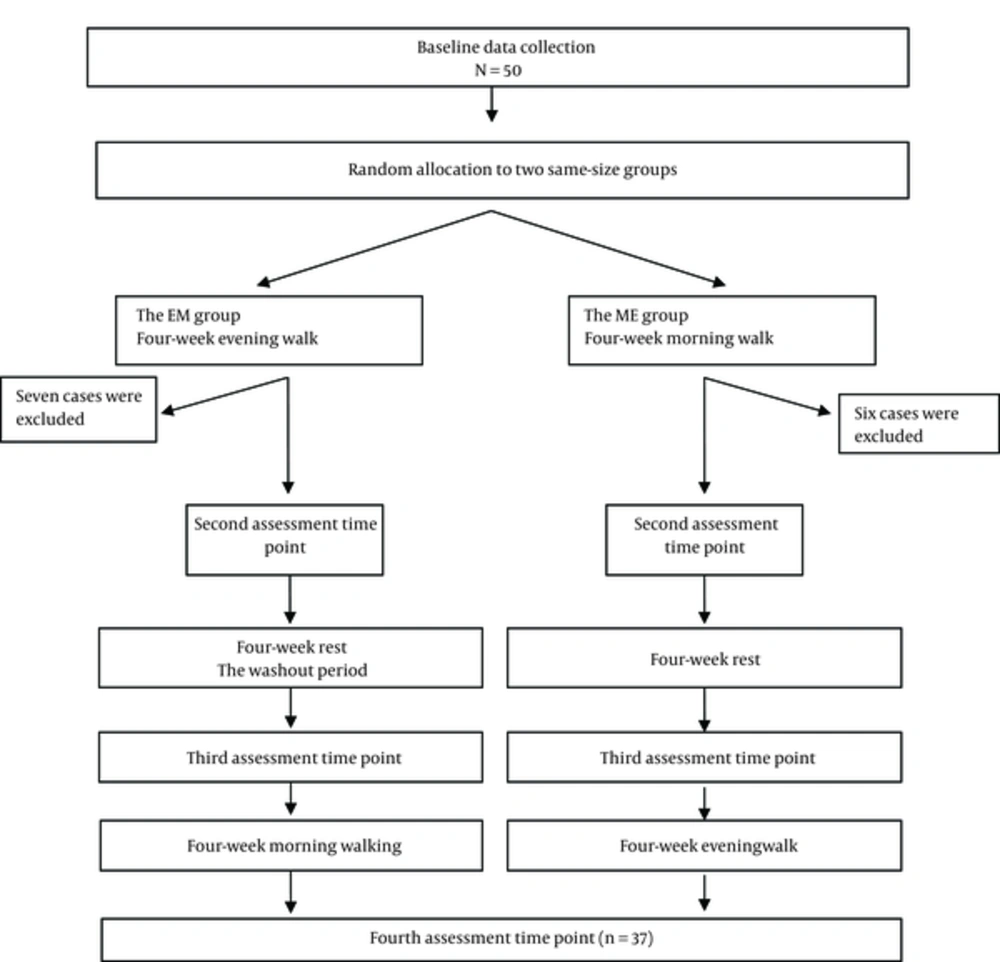
In total, there were 276 eligible elderly people in the study setting; 50 were selected and randomly allocated into morning-evening (ME) and evening-morning (EM) groups. In the first phase of the study, participants in the ME and the EM groups, respectively, went on morning and evening walks for 4 consecutive weeks. Thereafter, they were asked to avoid any sort of regular walking for 4 consecutive weeks. This 4-week rest was considered as the washout period. In the second phase, i e, after the washout period, the intervention was reversed and participants in the ME and the EM groups, respectively, went on evening and morning walks for 4 weeks. This crossover design helped to minimize the effects of confounders and do the study with smaller sample size. Walking sessions were held 3 times a week. Each session consisted of warm up exercise (3 to 5 minutes), walking (30 minutes), and cool-down exercise (3 to 5 minutes). Morning and evening walk sessions were held at 08:00 - 09:00 AM and 04:00 - 05:00 PM, respectively. All sessions were held in a city park and were managed and coached by the first author and a fitness coach. PSQI was completed for participants by a research assistant at 4 assessment time points, namely before the intervention, immediately after the first intervention, immediately after the washout period (i e, before the second intervention), and immediately after the second intervention.
Before the intervention, informed consent was obtained from all participants based on the requirements of the ethics committee and the institutional review board of Rafsanjan University of Medical Sciences, Rafsanjan, Iran. Moreover, participants were adequately informed about the objectives of the study and the confidential management of the study data. The current study was registered in the Iranian registry of clinical trials (No. IRCT2016030826965N1) and approved by the ethics committee of Rafsanjan University of Medical Sciences, Rafsanjan, Iran (No. IR.RUMS.REC.1394.185).
In total, 6 participants from the ME group and 7 from the EM group were excluded due to their irregular attendance at walking sessions. Therefore, final data analysis was carried out on the collected data from 37 participants (19 in the ME and 18 in the EM groups) (Figure 1). Participants were 23 females and 14 males. Collected data were transferred into the SPSS software version 18.0 and described using the measures of descriptive statistics (such as mean and standard deviation (SD). The Chi-square and the independent-samples t tests were used for intergroup comparisons while the paired-samples t test and the repeated-measures analysis of variance (ANOVA) were performed for intergroup comparisons. Moreover, crossover analysis was performed to compare sleep quality scores in the 2 groups (27), and carry-over effect was calculated to evaluate the residual effects of the first intervention on the results of the second intervention. Significance level for all statistical tests was 0.05.
3. Findings
At both baseline assessments (I e, before the first and the second interventions), groups did not differ significantly regarding the mean score of sleep quality (P > 0.05).However, the mean scores of PSQI after both morning and evening walks were significantly lower than those of the corresponding baseline mean scores (P < 0.05; Tables 1 and 2). Crossover analysis showed that the effects of morning walk on sleep quality did not significantly differ from the effects of evening walk (P = 0.873; Table 3). Moreover, carry-over effects of morning and evening walks on the sleep quality were not statistically significant (t = 1.293; df = 35; P = 0.123). This finding denotes that the first intervention had no significant residual effects on the results of the second intervention. In other words, washout period was long enough to remove the effects of the first intervention.
| Variable | Groups | N | After the First 4-Week Walking | After the Second 4-Week Walking | t | df | P Value |
|---|---|---|---|---|---|---|---|
| Mean score of sleep quality | ME | 19 | 2.69 ± 7.84 | 1.54 ± 6.05 | 0.032 | 35 | 0.873 |
| EM | 18 | 1.69 ± 6.61 | 1.61 ± 5.56 |
The results of the repeated-measures ANOVA for the within-subject factor of time also illustrated a significant difference in the variations of sleep quality mean score across the study. Post hoc analysis revealed that baseline mean score of sleep quality was significantly higher than those of both posttest mean scores (P < 0.001). However, the difference between the 2 posttest mean scores was not statistically significant (P > 0.05; Table 4).
| Time | Mean ± Standard Deviation | F | df | P Value |
|---|---|---|---|---|
| At baseline | 13.65 ± 2.16 | 217.27 | 2 | < 0.001 |
| After 4-week morning walking | 6.73 ± 2.49 | |||
| After 4-week evening walking | 6.32 ± 1.62 |
4. Discussion
The current study aimed at comparing the effects of morning and evening walks on nighttime sleep quality among elderly people. Results illustrated that after the first and the second 4-week walks, sleep quality score significantly decreased in both groups, denoting significant improvement in sleep quality. Similarly, an earlier study showed the positive relationship between physical exercise and sleep quality (28).
Previous studies also reported that walking can improve sleep quality among elderly people. For example, Sardar et al. found that an 8-week aerobic exercise positively affected mental health, anxiety, and insomnia (29). Gebhart et al. also reported the relationship between physical exercise and sleep quality (30). Similarly, Dadashpoor et al. found that water exercise significantly improved sleep quality among male elderly people (6). Rahmaninia also indicated that an 8-week walking program positively affected sleep quality and duration as well as several sleep-related physiological parameters (31). Kalak et al. also reported significant improvements in sleep quality among elderly people after doing morning exercise (32).
Findings of the current study showed that despite significant improvements in sleep quality after both morning and evening walks, there was no significant difference between the effects of these 2 types of walking on sleep quality. Similarly, the results of a crossover trial conducted by Benloucif et al., showed that both morning and evening exercises (for 14 days) significantly improved psychosocial functioning and sleep quality among elderly people (24). Passos et al. also showed that moderate anaerobic exercise either in the morning or evening improved subjective and objective sleep quality, mood, and quality of life among patients with chronic primary insomnia. However, their findings showed no significant correlation between exercise time and sleep quality (33). Contrarily, Yoshida et al. found that late night exercise (performed at 08:30 - 09:30 PM) was more effective than other time of exercise in improving sleep quality among male students who had no regular exercise habits. They reported that evening exercise affected sleep positively, and reduced daytime napping (25). These findings may be an explanation for insignificant difference between the effects of morning and evening walks in the current study. It is noteworthy that in the current study, there was a wide time interval between evening walk and sleep time.
Different mechanisms are reported for the effects of exercise on sleep quality. Some scholars noted that fatigue and increased core body temperature brought about by exercise improve sleep quality through stimulating hypothalamus to secrete melatonin (9). Yamanaka et al. also reported that both morning and evening exercises markedly affected nighttime body temperature and cardiac activity during sleep. They also reported that morning exercise improved sleep quality through enhancing sympathetic activity and noted that evening exercise should be avoided (34). Another study also attributed the hypnotic effects of melatonin to the core body temperature. Some scholars also noted that chronic insomnia may be associated with low blood levels of serotonin (35).
Currently, physical exercise is considered as an effective non-pharmacological therapy to manage different health problems including sleep disorders. However, the mechanism of its action is still unknown. One of the study limitations was the limited access to participants and therefore, the inability to evaluate their lifestyles, dietary habits, and treatment regimens. Another limitation was the wide time interval between evening walking and sleep time. Further studies are needed to assess the effects of different types of walking (in terms of time, duration, and intensity) on different aspects of sleep.
Similar to a study conducted by Benloucif et al. the washout period in the current study was 4 weeks (24). In line with their findings, the findings of the current study also showed the elimination of the effects of the first 4-week walking after the washout period. All these findings denoted that a 4-week washout period was long enough to eliminate the effects of walking on sleep quality in crossover trials.
4.1. Conclusions
The findings of the current study showed that morning and evening walks similarly improved sleep quality. Thus, elderly people can be recommended to include walking exercise in their daily schedule to improve their sleep quality. Given the importance of sleep quality, exercise, and physical activity on elderly people’s health and well-being, they should be strongly supported and encouraged to actively engage in doing regular physical exercises.