1. Background
Obsessive-compulsive disorder (OCD) has been introduced as an independent category in the fifth edition of the diagnostic and statistical manual of mental disorders (DSM-5). OCD is characterized by obsessive thoughts and unwanted repetitive behaviors (i.e. compulsions). Its global prevalence is 1.8% (1). Untreated OCD is associated with significant educational, familial, and social dysfunctions and increased risk for other psychological and psychiatric disorders (2, 3).
After medication therapy, the most common OCD treatment is exposure and response prevention. However, 15% - 40% of patients do not respond to it, 25% reject it, and 3% - 12% discontinue it. Therefore, cognitive therapy and cognitive-behavioral therapy (CBT) were introduced (4). Despite the known effects of cognition in OCD, cognitive interventions, either alone or in combination with exposure therapy, are not more effective than single exposure therapy (5). This is probably due to the fact that besides cognitions, emotions can also contribute to the formation of mental disorders. Accordingly, the third-generation CBTs, such as schema therapy, were developed to incorporate different views into comprehensive therapies, which aim to manage and modify cognition, emotion, and behaviors.
As an extension of CBTs, schema therapy was developed for the management of refractory chronic mental disorders. This therapy focuses on early life experiences, which form memories and schemas that are re-activated in different situations. These schemas are formed due to the unfulfillment of basic childhood emotional needs such as the needs for safety, free need expression, recreation, spontaneity, and realistic limits. These schemas are persistent and include abnormal patterns that significantly contribute to symptom development. Schema therapy deals with creating psychological awareness about these schemas and modifying them through cognitive and experiential techniques. The main focus of schema therapy is on therapist-patient relationship as well as the use of those cognitive and experiential techniques that magnify the effects of CBTs (6).
One of the main differences between schema therapy and CBT is the role of therapy relationship in these two methods (7). In fact, due to OCD patients’ great resistance against exposing to obsessive thoughts and behaviors during CBT as well as their poor insight about symptoms and symptom recurrence, they need more effective treatments, which not only modify cognitions and behaviors, but also restructure and correct emotions. These patients are too hostile and cannot collaborate with their therapists and follow treatment protocols. Therefore, therapy relationship is among the most important strategies for the assessment and management of these patients (6).
There are 18 schemas, the prevalence of which differs according to the underlying mental disorder (6). For instance, OCD patients mainly have the emotional inhibition, emotional deprivation, and vulnerability schemas, while the most common maladaptive schema among patients with depression, anxiety, and eating disorders is abandonment, which is indicative of unfulfilled needs such as safety, trust, and empathy (8, 9). In addition, patients with obsessional neurosis mainly have the social isolation, emotional inhibition, vulnerability, and mistrust schemas (10, 11).
Schemas can be used to predict treatment outcomes with varying degrees of confidence. For instance, a study on patients who received exposure and response prevention therapy showed that the abandonment schema was a negative predictor of treatment outcomes while the self-sacrifice schema was a positive one (11). Another study into early maladaptive schemas among 70 OCD patients also indicated that patients obtained high scores for the failure and the emotional inhibition schemas and these two schemas together with depression symptoms were associated with poorer treatment outcomes (12). The most important limitation of these studies was that they dealt solely with the relationships of early maladaptive schemas (such as vulnerability, emotional deprivation, emotional inhibition, and failure) with the severity of obsessive symptoms. In other words, there is limited information, if any, about the effects of schema therapy on OCD-related outcomes. Therefore, this study was conducted to assess the effects of schema therapy on the four maladaptive schemas of emotional deprivation, emotional inhibition (both are related to emotional self-awareness), vulnerability, and failure. These four schemas are among the most common schemas among OCD patients.
Emotional self-awareness is the ability to be aware, understand one’s own feelings, and recognize physiological states and the feeling-related aspect of emotions. Therefore, emotional self-awareness deficit, characterized by inability to correctly recognize and express emotions, can significantly contribute to the development of mental disorders (10-12). The most severe type of emotional self-awareness deficit is alexithymia (or emotional silence). Patients with alexithymia are unable to recognize their emotional states or have limited recognition of them. According to Lan and Schwartz, these patients have been trapped in the preoperational stage of the Piaget model of emotional development due to the fact that they lack necessary words for expressing their feelings (13). Therefore, they have limited cognition and recognition of their feelings and are unable to explain their complex emotional states and to experience others’ multidimensional emotions. Alexithymia is prevalent among OCD patients (10, 11).
Young Schema Theory holds that emotional self-awareness deficit is associated with the emotional deprivation and the emotional inhibition schemas. OCD patients have cognitive biases in processing external stimuli and therefore, have extreme fear about the occurrence of catastrophes and their inability to prevent them. This fear is characterized by serious concern, magical thinking, compulsive rituals, and repetitive questions to gain assurance (6). In magical thinking, a person feels that he/she can affect an event solely through thinking about it without taking mediating action. This feeling, in turn, requires the person to take some actions to prevent damages to self or others. Examples of such damage prevention behaviors are obsessive behaviors such as checking, washing, avoidance, and even symmetry (1). According to Young, this thinking style and these cognitive biases among OCD patients are associated with the vulnerability and the failure schemas.
To the best of our knowledge, no study had yet used schema therapy to modify emotional self-awareness and vulnerability. Thus, studies in this area are needed. The present study was done to fill this gap.
2. Methods
This was a clinical trial. Study population consisted of all OCD patients who, in a six-month period in 2016, referred to psychology clinics located in Birjand, Iran. Patients were included if they had been diagnosed with OCD based on DSM-5 criteria, obtained a score greater than four for questions about three schemas (namely the emotional inhibition, emotional deprivation, and vulnerability), obtained a score greater than 10 for Yale-Brown obsessive-compulsive scale, lack of acute psychiatric disorder (include severe depression), psychotic symptoms or drug abuse in the diagnosis of a psychiatrist and were willing to participate in the study.
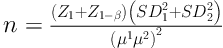
Based on the results of a study by Narimani (14). The total statistical population in this study was 210 people, of whom, 80 had a criteria for entry into the study. Based on the formula of Cochran sample size and its corrected form with 95% confidence level and 80% probability, the sample size was determined for each group of 16 people. Among 80, 32 individuals were randomly selected and assigned to intervention and control groups. One patient from the intervention group voluntarily withdrew from the study.
2.1. Instruments
Data collection was performed before and after the intervention using the following instruments.
2.1.1. A Researcher-Made Demographic Questionnaire
This questionnaire included items on age, gender, and educational and employment status.
2.1.2. Young Schema Questionnaire (YSQ)
We used the latest version of young,s schema model, which includes 18 proposed ESM, which are theorized to represent five broader schema domains (Young et al., 2003). Each of the items is rated on a six-point scale (1 = completely untrue of me, 6 = describes me perfectly). Higher scores indicate higher levels of EMS (early maladaptive schemas (EMSs). In this study, we used self-awareness assessment, the emotional inhibition, and emotional deprivation schemas, while items on the vulnerability schemas were used for vulnerability assessment. Young and Brown used YSQ in non-clinical populations and found that the Cronbach’s alpha and the test-retest correlation coefficients of its domains were 0.83% - 0.96% and 0.50 - 80, respectively. The score of YSQ was found to have high correlation with the scores of psychological distress, cognitive vulnerability, and symptoms of personality disorder, confirming its acceptable divergent and convergent validity. Factor analysis also supported its strong factor structure (6). Ghiyasi et al., validated the Iranian version of YSQ and reported Cronbach’s alpha values of 0.50 - 0.65 for its different domains (15).
2.1.3. Yale-Brown Obsessive-Compulsive Scale (Y-BOCS)
This scale is a symptom checklist and includes 35 questions regarding the symptoms of OCD such as aggressive, contamination, sexual, hoarding/saving, religious, symmetry, and somatic obsessions as well as miscellaneous obsessions such as memorizing unimportant things, fear over saying certain things, superstitious fears, intrusive images, and nonsense sounds or words in the mind. Besides obsessions, Y-BOCS also includes items on compulsions such as cleaning and washing, checking, counting, ordering/arranging, hoarding/collecting, and miscellaneous compulsions. Scoring is performed on a five-point 0 - 4 Likert-type scale. Scores 10 and higher reflect affliction by OCD (16). Khalaj found that the Persian version of Y-BOCS has an inter-rate correlation coefficient of 0.98, a Cronbach’s alpha of 0.89, and a test-retest correlation coefficient of 0.84 (17). In this study, the questionnaire was completed in full.
Study intervention was a 20-session schema therapy implemented by a PhD student in psychology in the research center of Birjand University of Medical Sciences, Birjand, Iran. Each schema therapy session lasted around two hours. The content of the sessions were the following.
Session 1: Introducing patients to each other; explaining the philosophy of forming the group; and framing the problem or disorder in schema therapy format.
Session 2: Selecting the emotional inhibition and the emotional deprivation schemas and tracing them in interpersonal relationships; understanding fundamental beliefs.
Session 3: Exploring the developmental origins of the schemas in childhood through experiential techniques and then, relating them with currently-used coping strategies.
Session 4: Assessing reasons behind the formation of schemas, particularly in the interactions with parents, based on the assumptions of schema therapy.
Sessions 5 - 8: Schema testing through collecting schema supporting and refuting evidence in childhood, adolescence, and adulthood; analyzing them through Socratic dialogue; reframing the schemas.
Sessions 9 - 1: Targeting the schema; implementing limited reparenting in order to recognize participants’ needs.
Sessions 12 - 13: Exploring the origins of the vulnerability schema through experiential techniques; understanding the developmental origins of the schema and relating it with obsessive symptoms.
Sessions 14 - 16: Assessing the reasons behind the formation of the schema based on needed fulfillment in childhood; testing the schema through collecting schema supporting and refuting evidence in childhood, adolescence, and adulthood; analyzing the schema through Socratic dialogue; and reframing the schema.
Sessions 17 - 19: Using the advantage-disadvantage technique to decide on whether or not to keep a schema; implementation of limited reparenting; imagination of phobic situations, particularly of obsessive avoidance; and teaching emotion regulation techniques.
Session 20: Assessing treatment outcomes and the methods for maintaining them through flash cards.
The collected data were entered into the SPSS software (v. 22.0) and analyzed using the multivariate analysis of covariance and the independent-sample t-test.
This study has the ethical approval of the ethics committee of Birjand University of Medical Sciences, Birjand, Iran. Patients were given information about the aim of the study and their consents were secured.
3. Results
One patient from the intervention group voluntarily withdrew from the study. Therefore, the number of patients in the control and the intervention groups were 16 and 15, respectively. The majority of participants were female (61.3%), held a bachelor or higher degree (51.6%), and half of them were employees (50%). Age means in the control and the intervention groups were 29.5 ± 11.00 and 30.13 ± 6.38, respectively. No significant differences were found between the groups regarding patients’ demographic characteristics.
Data analysis was done using the analysis of covariance. Due to the normality of the residuals (P = 0.70), there were significant correlations between the emotional inhibition, emotional deprivation, vulnerability, and failure schemas (r = 0.61) (P < 0.001). The results of multivariate analysis of covariance showed a significant difference between the groups respecting the posttest mean score of at least one of the subscales of emotional self-awareness, i.e. emotional deprivation and emotional inhibition. Based on results of multivariate analysis, the mean scores of the emotional deprivation and the emotional inhibition schemas in the intervention group significantly reduced from 24.00 and 22.87 at pretest to respectively 19.73 and 18.27 at posttest (P < 0.001). The posttest mean scores of these two schemas in the control group were 24.00 and 24.00, respectively (Table 2).
| Characteristics | Schema Therapy | Control | Result of Fisher Test |
|---|---|---|---|
| Gender | χ2, 0.39; df, 1; P 0.82 | ||
| Male | 5 (33.3) | 7 (43.8) | |
| Female | 10 (66.7) | 9 (56.3) | |
| Educational status | χ2, 4.26; P, 0.68 | ||
| Diploma | 3 (20) | 6 (37.5) | |
| Associate | 0 (0) | 1 (6.3) | |
| Bachelor’ s | 10 (66.7) | 6 (37.5) | |
| Employment status | χ2, 2.68; P, 0.93 | ||
| Employee | 8 (57.1) | 6 (42.9) | |
| Housewife | 3 (21.4) | 5 (35.7) | |
| Student | 1 (7.1) | 1 (7.1) | |
| Self- employed | 2 (14.3) | 2 (14.3) | |
| Age | 30.13 ± 6.38 | 29.5 ± 8.1 | F, 0.21; df, 1.42; P, 0.81 |
Participants’ Demographic Characteristics
| Outcomes | Group | P Value | |
|---|---|---|---|
| Schema therapy | Control | ||
| Emotional deprivation | ≤ 0.001 | ||
| Pretest | 24 ± 2.70 | 24.87 ± 2.19 | |
| Posttest | 19.73 ± 2.37 | 24 ± 2.71 | |
| Emotional inhibition | ≤ 0.001 | ||
| Pretest | 22.87 ± 2.80 | 24.75 ± 2.05 | |
| Posttest | 18.27 ± 2.49 | 24.81 ± 2.17 | |
| Failure | ≤ 0.001 | ||
| Pretest | 17.67 ± 4.65 | 21.50 ± 2.92 | |
| Posttest | 14.8 ± 3.21 | 20.81 ± 2.83 | |
| Vulnerability | ≤ 0.001 | ||
| Pretest | 22 ± 2.83 | 22.81 ± 2.66 | |
| Posttest | 16.87 ± 1.88 | 2.29±22.81 | |
| Obsessive symptoms | ≤ 0.001 | ||
| Pretest | 21.4 ± 6.62 | 2.78± 16.37 | |
| Posttest | 11.13 ± 4.66 | 2.08± 15.57 | |
Between-Group Comparisons Using Multivariate Analysis of Covariance
Moreover, at least one significant between-group difference was found respecting the posttest mean scores of the vulnerability and the failure schemas. The mean scores of these schemas in the intervention group significantly reduced from 22.00 and 17.67 at pretest to respectively 16.87 and 14.80 at posttest (P < 0.001). The posttest mean scores of these two schemas in the control group were 22.81 and 20.81, respectively (Table 2). The significant reductions and the insignificant changes in the mean scores of these two schemas in respectively the intervention and the control groups denote the significant effects of schema therapy.
Finally, we found that the mean score of obsessive symptoms in the intervention group reduced significantly from 21.4 at pretest to 11.13 at posttest (P < 0.001). However, this mean score did not change significantly in the control group. Therefore, between-group difference regarding the posttest mean score of obsessive symptoms was statistically significant (P < 0.0001). These findings imply that the significant reduction in the mean score of obsessive symptoms in the intervention group was due to schema therapy.
4. Discussion
This study aimed to assess the effects of schema therapy on emotional self-awareness, vulnerability, and obsessive symptoms among OCD patients. None of the between-group differences regarding the pretest mean scores of emotional self-awareness, vulnerability, and obsessive symptoms were statistically significant. Therefore, significant between-group differences at posttest can be attributed to the effects of schema therapy.
Study findings indicated that schema therapy significantly improved emotional self-awareness through reducing the mean scores of the emotional inhibition and the emotional deprivation schemas and thereby, regulating emotions. These findings were in agreement with the findings reported by Dadomo et al., and Fassbinder et al., (18, 19). According to Young, these two schemas are related to the fulfillment of basic human needs such as the needs for being loved by others, worthiness, attention, intimacy, care, self-expression, and emotion expression without any fear over punishment (7).
High scores in these two subscales reflect the inability to identify and express basic needs, ask from others, and speak less frequently about self. Patients with these two schemas usually refer to therapists due to senses of loneliness and sadness and do not expect to be understood and supported by therapists. Schema therapists use techniques such as imagery to help patients recognize their emotional needs. Then, they use the two-chair, the schema re-writing, and the schema dialogue techniques to help patients get angry at individuals who had roles in the formation of their schemas, talk with them, and emphasize on their own rights as a child. Thereby, therapy relationship has the most significant role in schema therapy (6).
In the present study, the mean scores of the emotional deprivation and the emotional inhibition schemas reduced from 24.00 and 22.87 at pretest to respectively 19.73 and 18.27 at posttest. According to Dadomo et al., and Fassbinder et al., emotional regulation is a multidimensional concept, which includes awareness and acceptance of emotions, goal-oriented behavioral skills, and flexibility in using appropriate strategies for reducing the severity and the length of emotional response. Any problem in each of these dimensions plays a significant role in the development of mental disorders. Schema therapy holds that cognitive therapy cannot regulate emotions and hence, experiential techniques are used to help patients express and manage their emotions as healthy and mature humans (18, 19). In line with our findings, Halford et al., and Saffari et al., also reported the effectiveness of schema therapy in alleviating emotional inhibition, emotional deprivation, and symptoms among patients with social anxiety disorder (20, 21).
Saffarinia et al., noted that early maladaptive schemas are strongly correlated with patients’ cognitive biases and inaccurate assessments of environmental stimuli. This correlation can in turn result in avoidance or exaggerated behaviors. They attributed the effects of schema therapy to its focus on individual differences in planning and using cognitive and experiential techniques (21).
In addition, Halford et al., justified their findings by noting that therapeutic alliance is a significant factor behind therapeutic changes in that a positive therapeutic alliance with a therapist provides patients with a correcting emotional experience and hence, can significantly contribute to treatment. Positive therapeutic alliance creates a safe environment in which patients feel adequate safety to approach phobic affects and emotions (20).
Our findings also showed the effectiveness of schema therapy in significantly reducing the scores of the vulnerability and the failure schemas from 22.00 and 17.67 to respectively 16.87 and 14.8. These reductions are clinically significant. These two schemas are associated with incompetence and uncertainty in decision-making, extreme negligence or perfectionism, and exaggerated fear over an imminent catastrophe or violation of one’s own or others’ rights. Patients with these two schemas have unfulfilled safety, approval, and positive attention needs. In schema therapy, therapists use cognitive, skill-training, and reality-testing techniques to help patients obtain an accurate understanding of their own abilities and encounter phobic situations instead of exaggerated avoidance from them (6). Therefore, schema therapy can change patients’ thinking about catastrophizing and behavioral avoidance, which they use to prevent catastrophes and damages. The vulnerability and the failure schemas are strictly related to obsessive symptoms and therefore, we used techniques related to these schemas to increase the effects of exposure and response prevention therapy.
In line with our findings, Halford et al., Saffarinia et al., and Hamzeh et al., reported the positive effects of schema therapy on the vulnerability and the failure schemas among patients with depression, anxiety and social anxiety disorder. To justify their findings, they noted that through cognitive and behavioral techniques, such as role playing and also through subjective and realistic exposure to anxiety-provoking situations, schema therapy helps patients obtain a realistic estimate of a given danger, revise their estimate of the probability of catastrophe occurrence in social situations, and improve their capacity for effective coping with anxiety. Moreover, using behavioral techniques to change schema-driven pattern causes the formation of healthier coping styles and thus, facilitates distancing from maladaptive schemas (20-22).
The other finding of the present study was that schema therapy reduced the mean score of obsessive symptoms from 21.40 at pretest to 16.37 at posttest.
Theil et al., also made a study into the effects of exposure and response prevention as well as schema therapy and found that experiential techniques of schema therapy (such as the two-chair, schema dialogue, and imagery writing techniques) reduced patients’ resistance to receive treatments and alleviated obsessive symptoms among OCD patients. According to Thiel et al., exposure and response prevention is effective for patients who do not obtain high maladaptive schema scores. Thus, when schema scores are high, experiential techniques can facilitate the process of exposure (23).
In OCD patients, behavioral avoidance and repetitive rituals prevent the realistic processing of anxiety-provoking stimuli such as contamination and disorderliness. Cognitive techniques specifically assess and challenge deviations, which result in these behaviors. The therapist determines some tasks to expose patients to anxiety-provoking stimuli subjectively and then realistically, supports cognitive challenges, and hence, helps alleviate symptoms.
In fact, schema therapy helps patients become aware of their memories, cognitions, bodily sensations, emotions, coping strategies, and consciously manage their schemas (6).
4.1. Conclusion
Schema therapy alleviates obsessive symptoms through positively affecting maladaptive schemas such as emotional inhibition, emotional deprivation, vulnerability, and failure. These findings suggest that these schemas play significant roles in the development of obsessive symptoms. Conventional exposure of OCD patients to unpleasant stimuli is very anxiety provoking, while cognitive and experiential techniques of schema therapy help explore and modify the origins of these anxieties. Currently, schema therapy is not routinely used for OCD management; therefore, mental health specialists are recommended to use it as an effective treatment for OCD outpatients.
One limitation of the study was its small population and sample. Therefore, the generalizability of the findings should be done cautiously. Further studies are needed to produce more convincing evidence.
