1. Background
Pain is a multidimensional phenomenon and a difficult-to-define concept. The International Association for the Study of Pain defines the pain as “an unpleasant sensory and emotional experience associated with actual or potential tissue damage” (1). Pain is a subjective experience and the main cause of seeking preventive or therapeutic medical services (2).
Infants receive several vaccines through injection. Vaccination is an iterative painful experience (3) and is considered the most common cause of iatrogenic pain and stress (4). Previous experience of vaccination pain causes children to anticipate vaccination pain and show physiological, hormonal, and behavioral responses to vaccination such as physiologic instability, crying, irritability, poor collaboration, stress, anxiety (5), apnea, cardiac dysrhythmia, increased blood and intracranial pressures, tachypnea, altered immunity, delayed wound healing, and altered development of the nervous system (6). Vaccination pain also affects parents and healthcare providers. Nonetheless, healthcare providers consider it an inevitable experience, which does not need any serious intervention (7).
The World Health Organization (WHO) considers pain alleviation to be a component of vaccination programs (8). Massage therapy (including both touch therapy and manual pressure) is one of the simplest pain alleviation methods (9). Different techniques of massage, such as friction, vibration, and pressure can provide muscular and mental relaxation and raise pain threshold (10). According to the Gate Control Theory, massage facilitates the inhibition of pain transmission in C fibers by A fibers in the dorsal horn of the spinal cord. Massage can also alleviate pain by facilitating the release of beta-endorphins in the blood (11).
A study on 98 adult patients reported that manual pressure on the muscular injection site significantly alleviated the injection pain (12). Another study on students reported that manual pressure on the injection site before the injection of Hepatitis B vaccine was effective in alleviating the injection pain (13). Manual pressure of the injection site before benzathine penicillin injection was also found to significantly alleviate the injection pain among patients with rheumatic heart disease who aged 7 - 20 years (14). On the contrary, a study on adult people reported that manual pressure on the injection site had no significant effects on the pain associated with the subcutaneous injection of influenza vaccine (15).
Previous studies provided no reliable information about the effects of manual pressure on vaccination pain among children. In this regard, the contradictory results of previous studies regarding the effects of manual pressure on the injection pain highlight the necessity of further studies in this area.
2. Objectives
Thus the present study was conducted to fill these gaps. The aim of the study was to assess the effects of manual pressure on the injection site on vaccination pain among infants.
3. Methods
3.1. Design and Participants
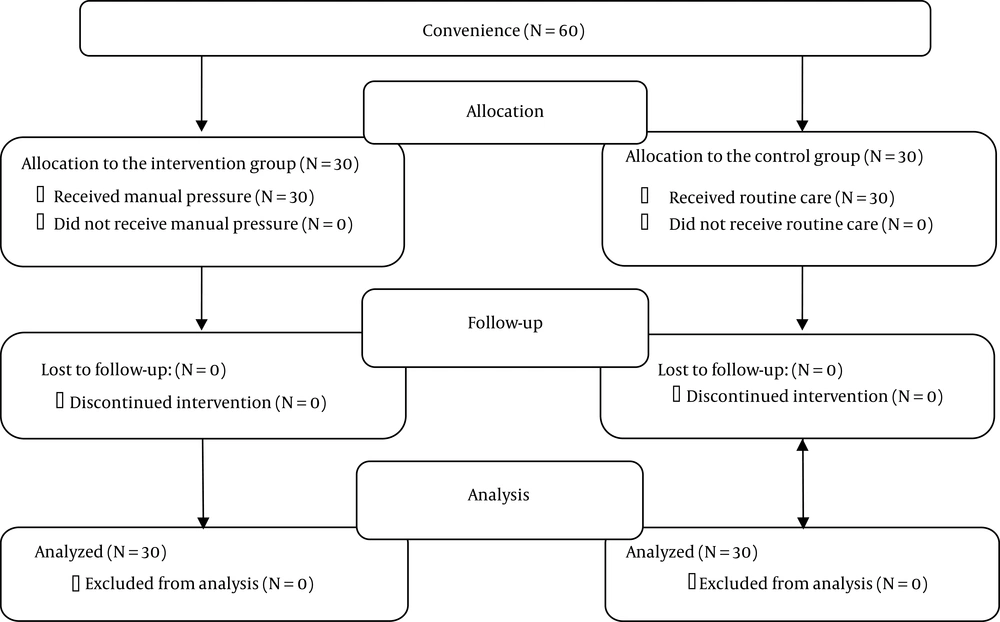
This two-group clinical trial was conducted in 2017 - 2018. The study population consisted of four-months-old infants who referred to a primary healthcare center in Birjand, Iran to receive the pentavalent (diphtheria, pertussis, tetanus, hepatitis B, and haemophilus influenzae type B (DPT-HepB-HiB) vaccine). Participants were sixty infants who were conveniently recruited from the study setting. Inclusion criteria were parental consent, wakefulness and calmness at the time of vaccination, dry diaper, no history of hospitalization, no affliction by cold or diarrhea at the time of vaccination, full-term birth, age four months, no pain medication use by mother or infant since 48 hours before vaccination, normal growth curve, no affliction by cerebral paralysis or developmental disorder, and no specific finger/pacifier sucking habit. Mother’s reluctance to stay in the study was the only exclusion criterion. The participants were randomly allocated to the control and intervention groups by block randomization (Figure 1).
The sample size was calculated using the results of a previous study and the following sample size calculation Equation 1:
With a power of 80%, confidence interval of 95%, µ1 of 8, µ2 of 6.9, S1 of 0.81, and S2 of 1.2; then sample size was determined to be eighteen per group. In order to increase the precision of the study, the sample size was increased to thirty (16).
3.2. Instruments
Study instruments were a demographic form and the face, legs, activity, cry, and consolability (FLACC) scale (17). The demographic questionnaire included items on gender, weight, crying length, time interval between the last sleep and vaccination, time interval between the last feeding and vaccination, and previous experience of painful procedures. The FLACC scale was developed and validated in 1997 by Merkel et al. in the University of Michigan (17). It assesses facial expression, leg posture, activities, crying, and consolability in response to the pain. The score of each domain can range from zero (“no response”) to 2 (“maximum response”), resulting in a total score of 0 - 10. Scores 0 - 3, 4-7, and 7 - 10 represent mild, moderate, and severe pain, respectively. Two previous studies reported that the inter-rater correlation coefficient and the Kappa agreement coefficient of the scale were 0.94 and 0.82, respectively, confirming its acceptable reliability (18, 19). A study in Iran also found a significant correlation between the scores of the FLACC scale and the Faces Pain Scale, with a correlation coefficient of 0.707 (16). For reliability assessment in the present study, two raters simultaneously applied the FLACC scale to fifteen infants. The inter-rater correlation coefficient was 0.73. For pain assessment using the FLACC, participants were filmed from the beginning of the injection to three minutes afterward. Then assistant researchers who were blind to the study aims used the FLACC scale to assess the movies and rate pain intensity. The length of crying was also measured using a digital stopwatch (HS34, Q&Q), the reliability of which had been confirmed using a similar stopwatch.
3.3. Intervention
In the intervention group, the participants were placed on the vaccination table and provided with manual pressure on the injection site for ten seconds immediately before vaccination until the injection. Manual pressure was applied using the thumb and was as firm as feeling tissue resistance. All injections were given to the vastus lateralis muscle, by an identical vaccinator, using identical injection devices (2 cc syringe, 23-gauge, equal series), and in identical conditions (respecting disinfectant solution and environmental temperature, lighting, and noise). Before the intervention, the vaccinator was trained about the vaccination and the manual pressure procedures. Infants in the control group did not receive any pain alleviation method.
3.4. Ethical Considerations
The paper is extracted from an MSc thesis approved by the Deputy of Research at Birjand University of Medical Sciences (approval No., 455442; ethical approval IR.BUMS.REC.1397.50 and registered in the Iranian Registry of Clinical Trials (code: IRCT20140519017756N46). Also, the study was conducted in accordance with the principles of the Declaration of Helsinki.
3.5. Data Analysis
Data were analyzed by the SPSS software (version 16.0). The measures of descriptive statistics (including mean, standard deviation, and frequency) were used to describe the data. Between-group comparisons with respect to the participants’ gender, weight, crying length, and feeding-vaccination time interval were performed by the chi-square and the independent-sample t-tests. As the distributions of the sleep-vaccination time interval and the pain intensity variables were not normal, between-group comparisons respecting these two variables were performed using the Mann-Whitney U test. All statistical analyses were conducted at a significance level of 0.05.
4. Results
In total, sixty infants participated in the study. Most participants in both groups were male (60%). There were no significant differences between-group respecting the participants’ gender, weight, feeding-vaccination time interval, sleep-vaccination time interval, and previous experience of painful procedures (P > 0.05; Table 1).
| Characteristics | Groups | Test Result | |
|---|---|---|---|
| Intervention | Control | ||
| Weight, g | 6794 ± 706.33 | 6515.33 ± 614.18 | t = 1.063, P = 0.1 |
| Feeding-vaccination time interval, min | 45.06 ± 36.16 | 34.70 ± 29.14 | t = 1.2, P = 0.22 |
| Sleep-vaccination time interval, min | 67.00 ± 23.06 | 86.50 ± 36.51 | Z = -1.82, P = 0.068 |
| Experience of painful procedures | χ2 = 0.635, P = 0.42 | ||
| Yes | 20 (66) | 17 (56.7) | |
| No | 10 (33.3) | 13 (33.3) | |
| Gender | χ2 = 0.001, P = 1 | ||
| Female | 12 (40) | 12 (40) | |
| Male | 18 (60) | 18 (60) | |
Description of Characteristic of the Studied Groupsa
The results of the independent-sample t-test illustrated that the mean of pain score in the intervention group was significantly less than the control group (P = 0.012). However, the Mann-Whitney U test showed no significant difference between the groups respecting the length of crying (P = 0.61; Table 2).
| Variables | Groups | Test Results | |
|---|---|---|---|
| Intervention | Control | ||
| Pain intensity | 7.93 ± 1.08 | 8.66 ± 0.96 | Z = -2.49, P = 0.012 |
| Crying length, s | 47.03 ± 18.27 | 50.56 ± 32.21 | t = -0.51, P = 0.61 |
Comparisons of Mean Pain Severity and Duration of Crying in Intervention and Control Groupsa
5. Discussion
This study aimed to assess the effects of manual pressure on vaccination pain among infants. Findings revealed that the mean of pain intensity in the intervention group was significantly less than the control group. Previous studies also reported the effectiveness of manual pressure and flick application on the injection site in significantly alleviating the injection pain (13, 14, 20). The Gate Control Theory asserts that like a gate, the gelatin-like portion of the dorsal horn of the spinal cord controls pain transmission to the brain. Naturally, this gate is closed, but when the severity of pain stimulation reaches pain threshold, this gate is opened to allow pain signal transmission to the central nervous system. The stimulation of Aβ fibers (for example through manual pressure) blocks pain transmission and perception because these fibers transmit sensory signals to the gelatin-like portion much faster than the other fibers and hence, close the gates and block pain transmission to the central nervous system by the other fibers. The terminals of most Aβ fibers are located under the skin; therefore, skin stimulation can stimulate these fibers, block pain transmission, and reduce pain perception (17). In contrast to our findings, a study reported the insignificant effects of manual pressure on the injection pain. The authors of that study attributed the ineffectiveness of their intervention to the effects of psychological factors and age on pain perception among their participants (15). Because of the contradictory results of previous studies regarding the effects of manual pressure on the injection pain, the WHO reported that this intervention may not be appropriate for pain alleviation until further studies confirm its effectiveness (21).
Our findings showed that manual pressure had no significant effects on crying length. In line with our findings, several earlier studies reported the insignificant effects of flick application, EMLA cream, and Vapocoolant spray on crying length after the injection of the trivalent (DPT) vaccine (20, 22, 23). On the contrary, some studies on infants found that the injection pain significantly was alleviated in response to foot massage (24), breastfeeding and mother-infant skin contact (25, 26), and distraction (21). Factors such as age, cognitive status, and emotions can affect the injection pain intensity and crying length among infants (4, 24).
5.1. Limitations
This study was conducted on infants and hence, its findings may not be generalizable to people of older ages. As recommended by the WHO (21), further studies are still needed to produce firm evidence concerning the effects of manual pressure on the injection pain among children of different ages.
5.2. Conclusions
This study concludes that manual pressure on the injection site significantly alleviates vaccination pain among infants. As a safe and simple technique, manual pressure can be used for pain alleviation among infants and thereby, enhancing parental satisfaction and collaboration in vaccination. Continuing education programs are recommended to familiarize healthcare providers with non-pharmacological pain management strategies.