1. Background
Chronic renal failure (CRF) is a health problem occurring worldwide and stands as a significant contributor to morbidity and mortality. It can occur secondary to other diseases at any age from infancy to old age depending on the cause (1, 2). The CRF growth rate in Iran is currently estimated at 114% and the number of patients in 2009 was estimated to be over 400,000 people (3). CRF treatment includes hemodialysis, peritoneal dialysis, and transplantation. Hemodialysis is the most common treatment used in end-stage renal disease. It is a practical life maintenance procedure, which has increased the life expectancy of thousands of patients with CRF. Before this treatment was developed, the diagnosis of CRF meant the definite death of the patient. However, the high cost of morbidity and complications of hemodialysis remain a problem (4-8). Hemodialysis is a treatment strategy for these patients. Hemodialysis requires a blood flow of 200 - 300 mL/min for 3 - 4 hours. Naturally, superficial vessels cannot provide this amount of blood. Therefore, vascular access methods are needed either temporary or permanent. Temporary vascular access includes arteriovenous shunt and central venous catheter. Permanent vascular access entails transplantation and arteriovenous fistula (AVF) (2, 9, 10).
A quarter of the care cost for hemodialysis patients is assigned to vascular access (11). Nurses’ attention to hemodialysis complications and prevention of complications such as inflammation and infection can increase the patients’ lifespan (12, 13). Sarani studied hemodialysis patients in some Iranian cities in 2001, reporting the prevalence of local infection as 85%, 36%, and 31% in hospitals of Tehran, Shahrekord, and Arak, respectively (14). Post-infection inflammation is a severe complication in hemodialysis patients. Souweine et al. showed that in the presence of inflammation, the risk of septicemia increases by 18 times, making infection as the second cause of mortality in hemodialysis patients (15).
Biological agents are the most important factors that predispose CRF patients to inflammation or phlebitis in the vascular access site. Contamination of the injection solution during infusion or preparation for injection, the transfer of bacteria from the skin to the catheter, and bacterial cloning at the end of the catheter are important biological factors that can cause phlebitis. Failure to comply with antiseptics at the time of catheter insertion is an essential biological factor that causes inflammation in the vascular access site (13, 16). Healthcare providers, and more importantly, nurses of hemodialysis wards are in charge of choosing a suitable antiseptic before inserting vascular access. A suitable antiseptic solution is characterized by a reduced number of microorganisms, broad-spectrum, rapid performance, and resistance to bacterial re-growth (17, 18).
In 2011, the Center for Disease Control and Prevention suggested the use of chlorhexidine, povidone-iodine, iodine, and alcohol antiseptic solutions to minimize the risk of infection in the catheter insertion site. Moreover, the center suggested the use of a combination of povidone-iodine and alcohol to reduce inflammation and infection in the catheter insertion site (19). Essential factors in the selection of a suitable antiseptic by nurses include the patient’s condition, immediate effect, stability, and low risk of bacterial resistance against it (9, 20, 21). Administration of a combination of alcohol and povidone-iodine disinfectant (betadine; generic name: alcoholic povidone), approved by the Food and Drug Administration, reduces the incidence of inflammation and bacterial colonization, hence reducing infections. This combination affects Gram-positive and Gram-negative bacteria. If alcohol is combined with betadine, its antiseptic power increases as the number of carbon chains increases. The solution destroys the bacterial cell wall, damages proteins, and destroys bacterial DNA; thus, it is considered a suitable antiseptic to use in vascular access of hemodialysis patients. Rapid onset and 96 h durability are among other advantages of this antiseptic (21-23).
Alcohol-idiophone effectiveness against gram-positive and gram-negative bacteria, rapid onset, and durability of 48 - 96 h with three minutes of scrubbing introduce it as a suitable antiseptic solution (24). A type of the solution is called DuraPrep. Findings confirm its efficacy in catheter insertion. The Nursing Journal of Injections (2005) reported a clinical trial where a combination of 70% alcohol and 10% betadine was more effective than separate applications of either of them. In the 2007 protocol, this method was proposed for vascular access of hemodialysis patients, as it destroyed the cell wall and damaged intracellular components (25).
2. Objectives
There is a lack of specific protocols for disinfection before vascular access in hemodialysis patients. Taking this into consideration and the specific conditions of these patients, we aimed to compare the effects of using alcohol after betadine and concurrently applying alcohol and betadine on the inflammation severity of vascular access sites of patients undergoing hemodialysis. Hope is to obtain a suitable method for disinfection before vascular access in hemodialysis patients.
3. Methods
This study was a randomized clinical trial with three groups. The population of the study included patients undergoing hemodialysis at Imam Reza and Montaserie hospitals, Mashhad, Iran. Sampling was done by the non-probability convenience method. The inclusion criteria were the absence of inflammation in the vascular access site, having three dialysis sessions per week, having normal HCT (hematocrit), and a history of at least six months of dialysis. The exclusion criteria were the absence of specific diseases such as leukemia, infectious diseases, and immune deficiency and non-use of antibiotics or immunosuppressive drugs. Patients receiving antiseptic solutions for only one session were also excluded. Patients meeting the inclusion criteria were randomly allocated to three groups by using the roll of the dice. The research procedure and possible complications were briefly described to the study sample and written informed consent was obtained from them.
The vascular access site was washed in the elbow or wrist depending on the location of vascular access insertion. A nurse performed the disinfection of the vascular access site and a checklist was prepared for antiseptic considerations. In group 1, the vascular access site was disinfected with a combination of 70% alcohol and 10% povidone (green betadine). The surgical drapes were placed on the patient’s hand. Then, from a 15 cm distance, we dumped 2 mL of povidone-iodine 10% solution (10% betadine green) and 1 mL of alcohol 70% (ethanol 70%) to galipad. In group 2, first alcohol and then betadine were used separately. In the control group, the routine method of disinfection was performed using betadine in due observance of antiseptic precautions.
Based on a pilot study (with 15 patients) and according to the Pocock formula with 95% confidence interval, α = 5%, and 1-β = 80%, the sample size was determined as 90 patients (n = 30 patients per group). However, given the anticipated attrition, 111 patients undergoing hemodialysis were included in the study (n = 31 patients in the control group and n = 40 patients in each intervention group). The attritions were three and seven patients in group 1 and group 2, respectively. In case the patients were not checked for more than one session or had not used the solution for more than two sessions, they were excluded.
The use of a scale is recommended for assessing and documenting the grade of inflammation. In this study, we used the inflammation criteria set by the International organizations (Infusion Nurses Society, 2006; Royal College of Nursing, 2010) to assess the severity of inflammation in the vascular access site in patients of the three groups in the hemodialysis sessions. The validation of this scale was done by content validity and its reliability was assessed by Spearman correlation coefficient (r = 0.91).
The severity of the inflammation was assessed by a person outside the research team. Hemodialysis was performed three sessions per week for 12 sessions in a period of four successive weeks. The assessment tool was based on a five-point rating scale, comprising no clinical sign (score 0), painless erythema (score 1), pain, edema, or both (score 2), palpable venous cord (score 3), and severe inflammation of more than 2.5 cm (score 4). The research assistant assessed the severity of inflammation using this instrument at the end of each dialysis session.
Data were analyzed using SPSS software (version 16, SPSS Inc., Chicago, IL, USA). Normal distribution of data was determined using the Shapiro-Wilk test. The three groups were evaluated using one-way analysis of variance (ANOVA) for homogeneous quantitative variables and chi-square test for qualitative variables. One-way ANOVA was used to compare the severity of inflammation in the three groups given the normal distribution of the data, while Tukey’s LSD post hoc test was used for paired comparisons. To investigate the impact on dependent variables, two-way ANOVA was used. To compare the severity of the inflammation, repeated-measures ANOVA was used. For all tests, a 95% confidence interval and a significance level of P < 0.05 were considered.
4. Results
The majority of participants were female (55%). The mean age of the participants was 46.3 ± 1.4 years and the majority of them were over 50-years-old. Most of the participants had fistula vascular access in the wrist (77%). This vascular access was mostly applied in patients’ recessive hand (73%). Medical records showed that 69% of hemodialysis patients had hypertension and 28% had diabetes (Table 1). The Kolmogorov-Smirnov test results showed that age was normal in the three groups (P = 0.29).
| Variable | Groups | P Value | ||
|---|---|---|---|---|
| Group 1 (N = 37) | Group 2 (N = 33) | Control group (N = 31) | ||
| Age, mean ± SD | 46.8 ± 16.6 | 44.7 ± 17.7 | 54.4 ± 1.6 | 0.06a |
| Sex, No. % | 0.6b | |||
| Male | 25 (68) | 16 (50) | 14 (45) | |
| Female | 12 (32) | 16 (50) | 17 (55) | |
| Vascular access site, No. % | 0.35b | |||
| Wrist | 29 (78) | 19 (59) | 23 (74) | |
| Elbow | 8 (22) | 13 (41) | 8 (26) | |
| Hand with vascular access, No. % | 0.27b | |||
| Dominant | 7 (19) | 12 (37.5) | 7 (23) | |
| Recessive | 30 (81) | 20 (62.5) | 24 (77) | |
| Vascular access type, No. % | 0.25b | |||
| Shunt | 11 (30) | 6 (19) | 6 (19) | |
| Fistula | 26 (70) | 26 (81) | 25 (81) | |
| Medical history, No. % | ||||
| Hypertension | 26 (70) | 25 (78) | 20 (64) | 0.44b |
| Diabetes | 9 (24) | 9 (27) | 9 (29) | 0.56b |
aResult of ANOVA test.
bResult of χ2 test.
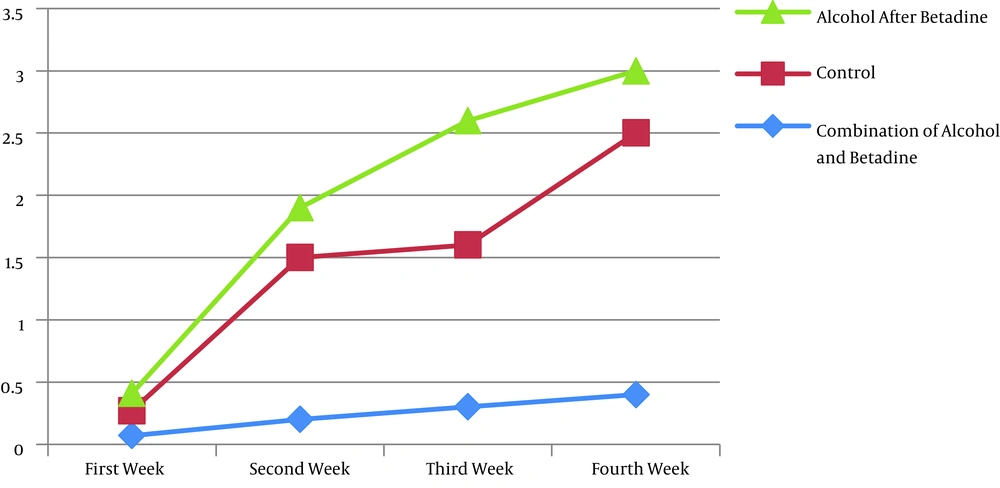
As shown in Table 2, the 12 hemodialysis sessions were divided into four weeks with each including three hemodialysis sessions. The Kolmogorov-Smirnov test results showed that the total score of inflammation severity in the four weeks was normal (P = 0.911). One-way ANOVA results showed no significant difference between the three groups in the first week (P = 0.089) although there were significant differences in other weeks. The Tukey’s LSD post hoc test results revealed no significant differences between group 1 (P = 0.06), group 2 (P = 0.498), and the control group (P = 0.223) in terms of inflammation severity in the first week. This test showed statistically significant differences between group 1 P = 0.06), group 2, and the control group (P = 0.037) in the inflammation severity in the second week. Nevertheless, no significant differences were found between the control group and group 2 (P = 0.518) in terms of inflammation severity. In the fourth week, all the differences between the three groups were significant. There was a significant difference in inflammation severity between group 1 and control group (P < 0.001), group 1 and group 2 (P = 0.03), and control group and group 2 (P < 0.001).
| Sessions | Groups | P Valuea | ||
|---|---|---|---|---|
| Group 1, Mean ± SD | Group 2, Mean ± SD | Control Group, Mean ± SD | ||
| First week | 0.07 ±0.1 | 0.14 ± 0.23 | 0.2 ± 0.3 | 0.08 |
| Second week | 0.2 ± 0.3 | 0.4 ± 0.4 | 1.3 ± 0.4 | 0.001 |
| Third week | 0.3 ± 0.4 | 0.5 ± 0.6 | 1.3± 0.7 | < 0.001 |
| Fourth week | 0.4 ± 0.6 | 1 ± 0.9 | 2.1 ± 0.7 | < 0.001 |
| Total mean ± SD | 0.2 ± 0.2 | 0.5 ± 0.3 | 1.1 ± 0.4 | < 0.001 |
aOne-way ANOVA results.
The mean and standard deviation of the total score of inflammation severity in the 12 sessions was 7.4 ± 6.4 (out of 48). Based on ANOVA, there was a significant difference in inflammation severity between the three groups (P < 0.001) in the four weeks. Repeated measures ANOVA showed that there was a significant difference in inflammation severity between the three groups and that the phase of measurement affected inflammation severity. Group and phase of measurement explained 48% and 49% of inflammation severity variances, respectively. As shown in Table 3 and Figure 1, the effect of group was significant on inflammation in the various phases of measurement (P < 0.001) and all of the effects (total, group, phase, and interaction) were significant (Table 3).
| ANOVA for Comparing Groups | P Value | df | F |
|---|---|---|---|
| Total effect | < 0.001 | 1 | 1.101 |
| Group effect | < 0.001 | 1 | 0.32 |
| Phase effect | < 0.001 | 96 | 3.101 |
| Interaction effect | < 0.001 | 6 | 6.20 |
Furthermore, the Bonferroni post hoc test showed that the most significant difference in inflammation severity was between the first and fourth weeks in the control group (P < 0.001). Two-way ANOVA results showed that the mean inflammation severity in the three groups was not significant in the first week but was significant in other weeks. This test also showed that the variables of age (P = 0.016), sex (P = 0.014), and vascular access type (P = 0.029) had significant independent effects on inflammation severity of vascular access, while the variables of diabetes (P = 0.031) and vascular access type (P = 0.036) had a significant interaction effect on inflammation severity of vascular access.
5. Discussion
According to the results of this study, as time passed, the difference in mean inflammation severity between the three groups increased, with the most significant difference found in the last week.
In the entire study period, there was no inflammation degree of 4, which was perhaps due to the short duration of the study. Application of alcohol after betadine was not significantly different from the routine procedure employed in the hemodialysis ward; however, the two procedures showed a significant difference in the prevention of inflammation. The study by Goudet et al. showed that using a combination of alcohol and betadine, compared to chlorhexidine used alone, reduced bacterial colonization at the time of vascular access (26). Inflammation is the initial stage of infection and if this solution can reduce infection, it may also reduce inflammation (5). The study by Brunicardi and Sangsuksawang (27) showed that a combination of alcohol and betadine could significantly reduce the inflammation of vascular access.
In similar studies, Frasca et al. stated that using a combination of alcohol and betadine in surgical scrubs was useful (27, 28). O’Grady et al. concluded that there was no significant difference between scrubbing the surgical area with alcohol and with the combination of alcohol and betadine (13). However, in the studies mentioned above, surgical scrubs were performed using brown betadine, while we disinfected the vascular access site with green betadine.
A reason for the difference between the present study and the reported research studies lies with the participants. Hemodialysis patients are susceptible to infection and inflammation of the vascular access site because of their weakened immune system, reduced glomerular filtration, and increased inflammatory factors. Given the limited timeframe (12 sessions of hemodialysis), patient follow-up, and weekly visits, there is a little chance of infection occurring during this period. At any rate, however, inflammation is an essential precursor to infection (25-28), which was studied here.
One limitation of the study is that the one-month evaluation of inflammation may not be long enough for infection occurrence. Therefore, it is suggested that future studies adopt prolonged periods and other indices to evaluate inflammation and phlebitis. Moreover, this study suggests the use of alternative self-care methods by patients and increasing patients’ self-efficacy for the irrigation and reduction of inflammation of the vascular access site.
5.1. Conclusions
In most studies, especially those conducted on temporary vascular access, the use of chlorhexidine is suggested and attention is directed to the importance of duration of effect and survival of antiseptic solutions in dialysis patients (20). The combination of alcohol and betadine has a lasting effect for up to 96 hours, which is equal to the time interval between two dialysis sessions (three times a week) for dialysis patients. An important point in these patients is that the vascular access site is affected by the natural flora of the patient’s skin. However, most studies show that the tip of the catheter is responsible for the infection and inflammation of the vascular access site (12-15). The strength of the present study lies with using the international organizations’ criteria (Infusion Nurses Society, 2006; Royal College of Nursing, 2010), and more importantly, incorporating hemodialysis patients who were susceptible to infection and inflammation.
Hemodialysis is a treatment strategy for these patients, and although it cannot eliminate the disease, it can increase patients’ lifespan; hence, it is necessary to perform hemodialysis with the fewest complications. The vascular access site is a patient’s vital path to survival, while inflammation of the vascular access site can change this path. Using a suitable antiseptic helps reduce this inflammation. In this study, the combination of alcohol and betadine is recommended as an inexpensive, accessible, and efficient solution. The tool used in this study was an observational measure, which highlights the role of nurses, and thus, nurses can consider this index as a daily protocol to assess patients.