1. Background
One of the contemporary phenomena in societies is population aging, with its highest levels occurring in countries, such as Iran, Korea, China, and Cuba (1). According to the United Nations report, the elderly population in Iran will increase by five times within 2011 to 2050. By the mid-21st century, Iran, with a 33% ratio of the elderly population, will be ranked as third in the world, compared to 21% in other countries. As the rate of increasing population aging is higher in developing countries than in developed ones, they have less readiness to confront aging and its negative consequences (2).
Aging is a critical risk factor for many chronic diseases, physical disabilities, dependency of the elderly on others, and psychological disorders, such as loneliness, isolation, and depression (3, 4). According to estimates of the global burden of diseases, more than 46% of the elderly population suffers from a degree of disability; however, its prevalence is higher in women than in men and in developing countries than in developed countries (3, 4).
Social changes in Iran, such as the widespread employment of women, decline in household size, and increased urbanization, have reduced family support for the elderly. It is necessary to develop a variety of long-term care facilities to maintain the participation and presence of the elderly in society (1, 5). Nevertheless, insufficient attention has been paid to the provision of good services for the elderly in Iran, and the healthcare services at various levels were not properly adjusted to meet the numerous health needs of older individuals (6).
Residential care centers are the most common form of long-term care for the elderly, and the demand for residents in these centers is increasingly growing (1). Many Iranian studies revealed that the services provided in residential care centers do not meet the required standards, and the care plans of these centers have not been developed according to the care needs of the elderly and their specific conditions. As the aging phenomenon emerges, the demand for long-term care services is increased; therefore, it is imperative to take necessary actions to create a variety of care models to shortly meet the needs of the elderly (1, 6). Consequently, the development of a national care model in Iran which encompasses the main healthcare components to meet the elderly’s needs in residential long-term care facilities is crucial in order to observe the care centers and their objective evaluation. Such model and its standards were developed based on the best practices, paying enough attention to local needs, and will have sufficient consideration on local conditions and resources of the Iranian health system (1, 6).
2. Objectives
Since studies have not developed a comprehensive and applied model to provide effective elderly care in Iran, the present study was carried out to develop an executive applied framework and a national model of care using the available valid scientific methods.
3. Methods
3.1. Design
The current study was conducted during 2014 - 2018. After conducting a systematic review to identify pioneer and prosperous elderly care models and their care standards, a two-round Delphi study was used to identify essential standards in the national care model for elderly individuals in residential care centers. The data gathering tool was a questionnaire, with a 9-point scale containing all the care standards, which should have been assessed from experts’ perspectives based on "significance" and "applicability" criteria. The experts were contacted by e-mail or face-to-face meetings. They were also informed of the objectives of the study and assured that the data would be confidentially treated (7, 8).
3.2. Participants
Based on the purposive sampling approach and for the provision of the most comprehensive information, potential and eligible participants were carefully recruited because they fit a particular profile. Therefore, the study focused on areas relating to health care for elderly individuals and professors and officers with at least 5 years of academic and executive experiences in geriatric health. The expert panel of the present study included the officials and headquarter staff of elderly planning at the Iranian Ministry of Health and Medical Education, Deputy of Health, faculty members, students involved in the field of aging studies, such as elderly health, health education, and promotion, nursing, and epidemiology, physicians with MPH degree, staff of management of health care system and health policymaking, staff of daycare centers and residential centers for the elderly, experts of the elderly health program in welfare organization, and experts in research centers for the elderly health, altogether 48 individuals.
3.3. Procedure
The research group performed a systematic review of credible databases and search engines to meet the existing requirements in the common model of care centers for the elderly in the world, such as extra care housing, sheltered housing, assisted living, day care centers, senior centers, nursing home, long-term care, and home care (research team) (1). Then, the initial requirements were identified and considered in the questionnaire in the form of care standards. In this regard, 305 primary standards were developed in six categories, including the package of health services, package of public services, service providers, service conditions, financing methods of services, and facilities of care schemes, based on the results of the conducted systematic review. Subsequently, all the standards were sent to the experts in various disciplines with a request for feedback on the relevance of each item to the questionnaire’s aim and based on the two criteria of significance and applicability using a 9-point scale to be reviewed and approved. The significance was clarified as the necessity of having any standard in the applied model for the care of the elderly in the care centers. The applicability was also well defined as the feasibility of implementing and measuring each of the standards in the status of the health care system, given the required financial resources, compliance with high-level laws, administrative and executive facilities and procedures, and political support in Iran.
3.4. Data Analyses
Given that using scale had a 9-point degree, the study had three phases of agreements, including "no agreement", "neutralized", and "agreement" phases with the median scores of 1 - 3, 4 - 6, and 7 - 9, respectively. Therefore, the care standards with scores lower than 4 will be eliminated, those with a median score of 7 - 9 were accepted, and those with a median score of 4 - 6 will go to the next round of the Delphi technique. After completing each round, the results need to be reviewed except for the approved or unapproved standards (with a mean higher than 4 and less than 7). For this purpose, the obtained median score of the standards from all experts and the scores given by each expert are provided to him/her while being informed of the views of other experts, and if desired, to change his/her views. This will continue until the experts reach a consensus. According to the Delphi technique principles, the response rate of experts in each round should be more than 70% to maintain its validity, and if the rate of changes in the scores given by experts in two consecutive rounds was lower than 15%, it would mean a consensus (7, 8).
3.5. Ethical Considerations
This study was approved by the Ethical Review Committee of Tabriz University of Medical Sciences, Tabriz, Iran (5/4/8099). To comply with ethical principles, researchers bound themselves to observe codes, such as the experts’ freedom to accept or refuse to cooperate in the study, respecting privacy, obtaining informed consent from experts, and assuring experts that the results would only be used for the defined and determined purposes.
4. Results
The experts who developed the final care model based on their views formed a wide range of specialized and experienced individuals related to the field of geriatric care. As shown in Table 1, the faculty members in the related disciplines of elderly care and headquarter and executive experts in institutions providing services to the elderly have the highest participation in the study to develop a care model.
| Responders | Frequency | Percentage |
|---|---|---|
| Academic professors in geriatrics, health services management, health education, and promotion, nursing, and epidemiology | 13 | 27.03 |
| PhD students in geriatrics, health services management, and health education and promotion | 8 | 16.66 |
| General physicians with geriatrics MPH | 7 | 14.58 |
| Experts of elderly care programs in medical sciences universities and organization of welfare | 12 | 25 |
| Top managers in medical sciences universities and organization of welfare | 8 | 16.66 |
| Total | 48 | 100 |
4.1. The First Round of Delphi Technique
At this stage, after giving a 45-day period to the experts for answering the questionnaire and the ongoing follow-up of the research group, Delphi first round was completed by collecting 40 questionnaires (83.33% of the response rate). In the next stage, all the questionnaires were analyzed, and a questionnaire was designed for the second round based on the results of the analysis. At this stage, based on the common principles, the standards scored less than 4 were excluded from the study, and those scored more than 7 were directly approved. The standards scored from 3 to 6 were included in the second round. Given that none of the standards gained a score less than 4, none of them were removed at this stage, and all the standards, except for 73 cases which scored 3 to 6, were finalized by the experts based on two criteria of significance and applicability (Table 2).
| Delphi Round | Response Rate | Total Standards | Approved Standards | Rejected Standards | Entering to Next Round |
|---|---|---|---|---|---|
| Round 1 | 83.33 | 305 | 232 | 0 | 73 |
| Round 2 | 95 | 73 | 43 | 30 | 0 |
4.2. The Second Round of Delphi Technique
In the second round of the study, 73 standard items scored within 4 to 7 were designed in a new questionnaire that contained the median scores of the experts and the score of each expert in the first round, which was specifically presented to the experts. At this stage, the experts re-scored the standards given the presented points. After giving a 1-month period to the experts, the questionnaires were re-collected, and 38 questionnaires were received (95% of the response rate) from the 40 submitted questionnaires. In total, 43 standards were accepted, and 30 standards failed to enter the final model due to failure to obtain acceptable scores in at least one of the aspects and reach a consensus (less than 15% of the change in score) (Table 2).
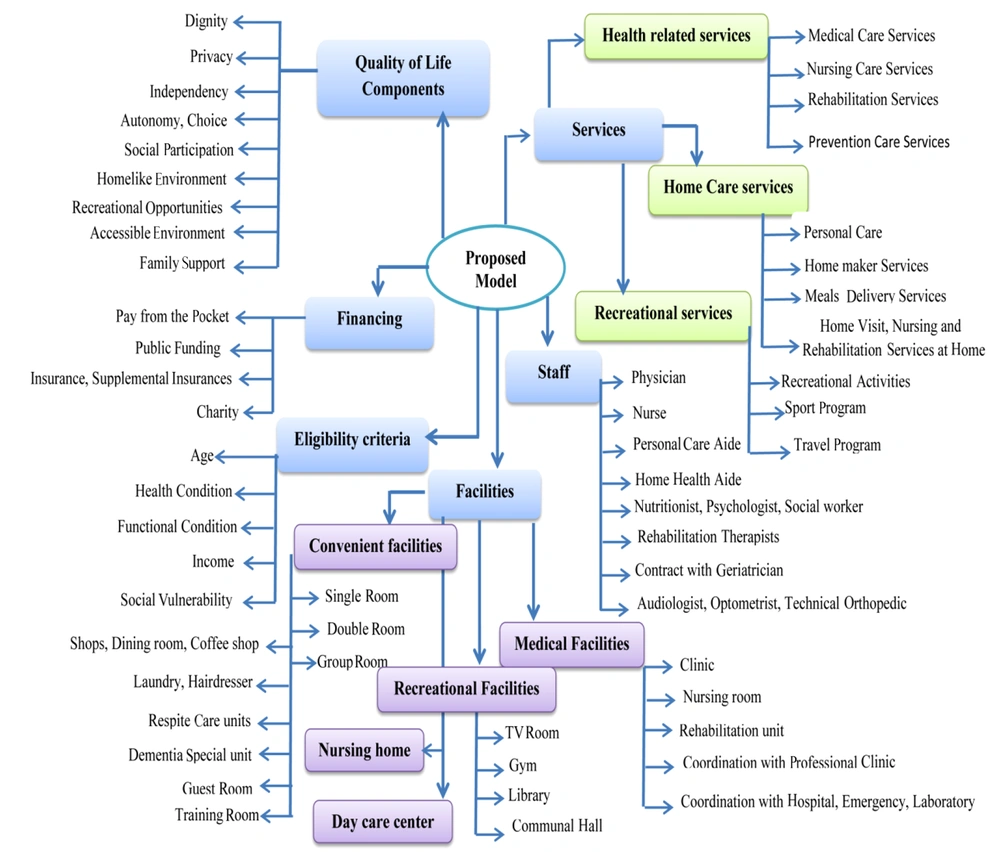
Out of the 275 final accepted standards, 102 (37.09%) 75 (27.27%), 42 (15.27%), 42 (15.27%), 9 (3.27%), and 5 (1.81%) standards were related to health-related services, service providers, public services, facilities of care centers, eligibility criteria, and financing, respectively.
4.3. Characteristics of Obtained Model
The field of health services in care centers included several issues, such as the assessment of the elderly upon admission, setting up a care plan based on the outcome of the assessment and care needs of the elderly, periodic assessment of the nutritional status, screening programs, treatment and rehabilitation programs related to common aging diseases, specialist referral services, nursing services, management and supervision of medicine consumed by elderly individuals, self-care educational programs for the elderly, mental health and nutrition counseling services, palliative care, rehabilitation services, and laboratory and radiology services. Public services included helping elderly individuals to carry out daily activities, such as eating, bathing, dressing up, and essential daily life activities (e.g., shopping, housekeeping, calling, and managing financial issues), hot meal delivery services and self-service, elderly leisure enrichment programs, elderly transportation services, educational courses based on the preferences of the elderly, legal counseling and setting up wills, and travel and tourism programs. Accordingly, the required human resources and physical environments were determined to properly provide these services.
The human resources domain in care centers includes two groups of specialized and non-specialized staff. For the specialized staff, nurses, geriatric nurses, general practitioners, paramedics, rehabilitation experts, social workers, nutrition experts, psychologists, dentists, geriatrics, internal medicine specialists, infectious diseases specialists, gynecologists, and orthopedists were proposed. Furthermore, the general staff includes supervisors, religious expert, and different types of coaches considering the interests of the elderly, administrative personnel, public services, security personnel, police forces, and volunteers. Facilities in the care center include the residential, health, administrative, entertainment, and welfare sites. At the residential site, private units should be arranged for elderly residence so that elderly couples, two friends, or two sisters can be accommodated. Moreover, suitable bathrooms, sanitary facilities, temporary accommodation for guests, units for providing respite care, a dining room, and space for holding classes and kindergartens should be provided.
At the health site, the general clinic, examining room, nursing room, rehabilitation department, isolated room, end-of-life care center, and medical equipment were emphasized. The welfare site included green space, restaurant, shop, cafe, library, gym, barbershop, and laundry service. At the administrative site, physical spaces were intended for the administrative staff. Furthermore, experts suggested that priority of admission to care centers should be given based on the criteria, including age (over 60 years), the elderly who are considered eligible for assessment in terms of their health or performance status based on the evaluation, elderly without a child, elderly without sufficient income or with low income, and elderly without housing. End-of-life care services should be provided to individuals who have a life expectancy of fewer than 6 months, according to a physician’s diagnosis. The financing domain includes various methods, such as out-of-pocket payments (OOPs) based on the financial power of the elderly, government support, public contributions, volunteers, and long-term care for the elderly by primary and supplementary insurance. Figure 1 depicts a summary of the final scheme of the developed model.
5. Discussion
Given that the current system of long-term health care in Iran has not been developed based on the growing population of the elderly and in accordance with their various health, psychological, and social needs, an initiative scheme has been presented in this study to provide long-term services for the Iranian elderly according to the findings obtained from the review of scientific literature and surveys of Iranian healthcare experts to design a national model. The developed model included six categories of health services, general services, service providers, facilities of care centers, financing methods of services, and eligibility criteria.
Due to the prevalence of chronic diseases among elderly individuals and various degrees of functional difficulties and mental health disorders, the demand for all types of health care and social support increases. Therefore, the elderly should have access to a variety of health, social, and recreational facilities. Long-term care includes a range of services and supportive care provided to the elderly and frail individuals to meet their health, psychological, social, and spiritual needs. Moreover, the goal of long-term care is to maintain and improve health status, independence, dignity, right to choose, and freedom.
In the package of health services, given the care needs of the elderly, the experts not only included the assessment during the admission in the center but also periodic assessments for updating the care plan of individuals, nursing services, medication management, radiology services, laboratory services, assessing and monitoring of nutritional status, nutrition counseling, mental health counseling, and various screening for cardiovascular diseases, diabetes, hypertension, urinary incontinence, mental health, sleep disorders, rehabilitation services (e.g., speech therapies, occupational therapy, audiometry, and optometry), in-service training courses, and self-care education sessions for staff considering common medical conditions affecting older adults and their needs. Furthermore, a variety of care models, such as extra care housing, residential homes combined with assisted living, and areas with a high percentage of the elderly population, have been developed to provide long-term care for the residents, including medical and nursing care, chronic disease management, rehabilitation services, vaccination, screening, nutrition counseling, and mental health care (9).
As the majority of older adults are suffering from functional limitations and are not able to carry out daily activities, social care services, namely personal hygiene, eating, bathing, dressing up, shopping, medication management, calling, financial management, hot-food delivery, and self-service, have been included in the proposed model. It can be claimed that personal care is an item of care involved in almost all long-term care models for the elderly in their packages of general services (10-12).
Long-term care should be comprehensive and unique. Older adults should access a care program appropriate to their physical, psychological, and disease conditions. In the proposed model, an initial assessment would be performed by a multidisciplinary team, including physicians, nurses, social workers, and mental health professors, to identify their care needs and accordingly design the care program. If further check-up by a specialist is required, the order would be issued by a general practitioner. In Japan, long-term care for individuals is assessed in two stages, and the care plan is arranged based on the dependence and care needs of individuals (13, 14). In the exclusive elderly care services in the United States, the elderly are also assessed by a team of physicians, nurses, geriatric nurses, social workers, and rehabilitation experts (15).
Grieving for the loss of a loved one, disabilities, depression, and negative effects of pain are known as the sources of stress in old age. Difficult life situations require the elderly to have a variety of psychosocial support to deal with these complications. In the proposed model, similar to other countries, such as the United States, Canada, and Sweden, community-based social and psychological support would be provided by staff, friends, family members, volunteers, and various social groups as one of the key components of long-term care for older adults (16-18). Respite care (i.e., temporary institutional care of sick, elderly, or disabled individuals, providing relief for their usual care) would be facilitated in the new model of care for caregivers. In countries, such as Japan, the United States, Taiwan, and Canada, respite care is also included in the package of long-term care services to support family members and those caring for the elderly (14, 16, 19).
With regard to the package of services, human resources are considered in the specialized and general fields. For the specialized staff, it is expected to include nurses, general practitioners, paramedics, rehabilitation experts, social workers, nutritionists, psychologists, and coordination with specialists, such as internal medicine specialists, rheumatologists, and orthopedists. The general staff includes caregivers, religious expert, and different types of coaches considering the interests of the elderly, administrative personnel, service and security personnel, and volunteers. In different models of long-term care in other countries, given the care needs of the elderly, a variety of technical staff are used to provide specialized and non-specialized care for the elderly.
Long-term specialized care services in the United States and home care in Sweden are provided by a team of general practitioners, nurses, nutritionists, social workers, occupational therapists, and physiotherapists (20, 21). Furthermore, in the residential care centers for older adults in Japan, physicians, nurses, practical nurses, occupational therapists, and physiotherapists collaborate (22). Finally, in Italy, nurses, nurse assistants, psychologists, psychiatrists, and rehabilitation specialists are employed in the residential care centers for older adults (23).
According to anticipated services (e.g., such as accommodation, personal care, and therapeutic and non-therapeutic care in the new model), facilities (e.g., guest room, outpatient clinic, and administrative department for employees), and recreational and welfare site facilities are projected for to scheme. In the welfare sector, stores, barbershops, laundries, cafes, gyms, and green spaces would be considered. In the extra care housing complex, a variety of facilities, such as an adapted bathroom, living room, shop, restaurant, playroom, laundry, and barbershop are well established (24). In the outpatient clinic, examination room, nursing station, rehabilitation department, isolated room, end-of-life care center, and medical equipment are accordingly proposed.
Maintaining and promoting the independence of the residents is also one of the goals emphasized by long-term care. To realize the above-mentioned issue in the proposed model, in addition to the provision of care for the elderly, the equipped micro spaces, such as baths and toilets, corridors, residential units, and transportation services, have also been proposed.
Moreover, retirement, lack of job opportunities, and social isolation are considered the psychosocial changes of old age. The reduction of social communication and loss of beloved ones and friends may lead to a sense of loneliness among older adults. Since the elderly are not able to optimize social relationships, and the reduced social interactions lead to reduced social support and perceived loneliness, it is necessary to create opportunities for their social well-being (25). The proposed model is intended to provide spaces for increasing social interactions of the elderly, such as the dining room, living room, gym, shop, cafeteria, and green space.
Today, in providing long-term care for the elderly, not only improving the quality of care but also the quality of life is intended. In the proposed model, the emphasis is placed on the individual or group accommodation of the elderly in a home-like environment as much as possible. It is also possible to accommodate elderly couples, two friends, or two sisters. Moreover, providing accommodations with circumstance similar to home is emphasized. The accommodation of older adults in an environment similar to home, arrangement of the furniture based on their wish and taste, and inclusion of sports, recreation, entertainment, and spiritual and intergenerational programs would enhance the quality of life. In residential complexes with assisted living in the United States, the architectural style is derived from the home design (26). There are also facilities, such as restaurants, adapted bathrooms, restrooms, laundries, barbershops, guest rooms, artistic activities, crafts, sports, games, music facilities, and transportation services (9, 24).
The target group in the proposed care model is the elderly, and the priority of admission to care centers is based on criteria, such as the age of over 60 years, the elderly without children, the elderly with low (or no) income, the elderly without housing, and the elderly with undesirable health status or functional limitations who are recognized as qualified during assessment for admission. In Japan, individuals over the age of 65 years are the target group for long-term care, and if individuals aged 40 - 64 years with some physical or mental disabilities are recognized as qualified, they will also receive medical and nursing care (27). In Sweden, the senior housing target group is those over 60 years of age (28).
Various methods are included for financing, such as OOPs, government support, public contributions, volunteers, and long-term care for the elderly by supplementary insurance. In other countries, long-term care is also provided through social insurance, private insurance, public participation, and charities, and the payment of part of the costs is made by the elderly through public funds (29, 30).
The strengths of the present study included the initial design of the model based on a systematic review of studies, finalizing the model based on the Delphi technique as an accepted scientific method for the achievement of scientific consensus, using the potential and eligible experts with high knowledge and experience in the field of elderly health, low attrition of experts in two Delphi rounds, and high mean scores of accepted standards. Furthermore, the low number of eliminated standards suggests that there has been a strong consensus.
5.1. Limitations
The first issue in this study was the limitation of relevant studies performed/published in Iran to compare the results and provide richer discussions in this regard. Another limitation was related to potential challenges which are posing to any Delphi technique, including selecting the key informants as the experts, ensuring the anonymity of experts in order to avoid their direct impact on each other’s perspectives. In addition, the high number of assessed developed care standards might affect the response rate of experts and accurateness of their delivered answers.
5.2. Conclusion
This study led to the development of a comprehensive model for elderly care in Iranian care centers and the inclusion of all aspects of care in it. The care standards were categorized into six domains, including the package of general services, package of health services, general service providers, service conditions, financing methods of services, and facilities of care centers. Given the use of valid scientific methods in this study and the unique comprehensiveness of the obtained model, the researchers are hopeful that its implementation improves the level of health and satisfaction of the elderly and enhances their quality and quantity of life. No doubt that the successful implementation of this model in Iranian elderly care centers needs conducting a pilot test phase and more improvement and flexibility.