1. Context
Irritable Bowel Syndrome (IBS) is a prevalent gastrointestinal disorder characterized by abdominal discomfort, bloating, and altered bowel movement patterns (1, 2). The prevalence of IBS varies across different geographical regions, affecting approximately 1% to 18% of the general population (2-4). While the exact etiology of IBS remains unknown, potential risk factors include individual characteristics such as age and gender, psychological factors like stress, and social, economic, and environmental influences (5, 6). Despite not being life-threatening, the chronic and recurrent nature of IBS significantly impacts patients' quality of life and imposes substantial personal and familial burdens (7-9).
Several pharmacological and non-pharmacological interventions are available for the management of IBS. Pharmacological options include probiotics, serotonin reuptake inhibitor antidepressants, antispasmodics, and alpha-2 adrenergic receptor agonists. However, the efficacy of these treatments remains debated among researchers, and there is no consensus regarding their effectiveness as standalone therapies (10, 11). Furthermore, these medications can have distressing side effects, often necessitating additional medications to manage them (12-14). As a result, some patients may feel dissatisfied with the outcomes of their prescribed drugs. Given the range of side effects and individual responses, it is crucial to incorporate non-pharmacological approaches alongside pharmaceutical interventions to optimize IBS treatment strategies.
Various psychological interventions have been explored to improve the condition and quality of life of individuals with IBS (15, 16). Non-pharmacological approaches, such as mindfulness, have garnered attention as cost-effective and low-risk interventions, supported by numerous researchers (17-19). Mindfulness includes the practice of Mindfulness-Based Stress Reduction (MBSR), a structured, short-term intervention that focuses on cultivating awareness of actions, sensations, thoughts, and emotions while promoting a non-judgmental, present-moment focus (20, 21). Mindfulness has emerged as a promising complementary treatment for IBS due to its potential benefits and minimal adverse effects.
Given the high prevalence of IBS and its significant impact on those affected, identifying effective treatments is essential for improving daily functioning and overall quality of life. With this in mind, the primary objective of this investigation is to critically examine the impact of mindfulness on the quality of life in individuals diagnosed with IBS.
2. Objectives
This study aims to contribute to the existing body of knowledge on the potential benefits of mindfulness-based interventions in IBS management, ultimately enhancing the well-being and daily lives of those affected by the condition.
3. Methods
3.1. Research Question
This study aimed to investigate the impact of mindfulness-based therapy on the quality of life, anxiety, and depression in individuals diagnosed with IBS.
3.2. Research Process
A comprehensive literature search was conducted across multiple databases, including PubMed, Scopus, Web of Science, and Cochrane, covering a 15-year period from 2010 to the end of 2024. The accepted languages for the article search were English and Farsi. The following predetermined search syntax was used to identify relevant published articles:
Keywords: "Mindfulnes [MeSH]
• Content related to quality of life: "Quality of Life" [MeSH], "Life Quality" [tiab], "Health-Related Quality of Life [tiab], "Health-Related Quality of Life" [tiab], "HRQOL" [tiab
• Content related to stress, anxiety, and depression: "Stress Disorders, Traumatic” [MeSH], "Stress disorder" [tiab], "Anxiety" [MeSH], "Anxiet [tiab], "Angst" [tiab], "hypervigilance" [tiab], "nervousness" [tiab], "Anxiousness" [tiab, "Depression" [MeSH], "Depress" [tiab] Date range: 2010/01/30 - 2024/05/30 [dp]
In addition to the databases, other sources such as conferences and critical journals were searched for gray literature.
3.3. Target Population
The study focused on individuals diagnosed with IBS from various countries. Participants were enrolled in studies that utilized mindfulness-based therapy as a psychological intervention to improve quality of life and manage symptoms of depression and anxiety.
3.4. Inclusion and Exclusion Criteria
Studies selected for inclusion primarily investigated the effects of mindfulness-based therapy on quality of life, anxiety, and depression in patients diagnosed with IBS. The search encompassed clinical, experimental, or quasi-experimental trial designs published in any language. However, studies that employed alternative behavioral treatments for this patient population were excluded from the analysis.
3.5. Intervention Type
Mindfulness-based therapy was the primary intervention type in the included studies.
3.6. Control Group
Due to the nature of the research, studies with control groups and within-subject designs were included.
3.7. Primary and Secondary Outcomes
The primary outcome of the study focused on evaluating changes in patients' quality of life before and after the intervention. The secondary outcome involved assessing changes in depression and anxiety levels before and after the intervention.
3.8. Data Extraction (Selection and Coding)
Full-text articles meeting the inclusion criteria were thoroughly evaluated. Relevant data, including the primary author, publication year, research location, target group, sample size, average age, primary and secondary outcomes, and intervention results, were extracted and organized in an Excel file (Table 1). Corresponding authors were contacted if additional information was needed for any article. Two researchers independently performed these steps, and the collected data were subsequently shared and aggregated.
| Authors; Year | Country | Sample Size | Target Group | Intervention | Control Group | Measured Variable | Outcome Measure | Important Outcomes |
|---|---|---|---|---|---|---|---|---|
| Henrich et al.; 2020 (17) | UK | 67 | Female | MBCT (mindfulness-based cognitive therapy) | Waiting list | Quality of life and IBS symptoms | Standardized self-report measures of IBS symptom severity, IBS quality of life, maladaptive illness cognitions (catastrophizing, visceral anxiety sensitivity) | Mindfulness significantly improved patients' symptoms and quality of life. |
| Gaylord et al.; 2011 (22) | USA | 75 | Female | Mindfulness training | IBS Support Group | Quality of life and IBS symptoms | IBS Severity Scale (primary outcome), IBS-quality of life, brief symptom inventory-18, Visceral Sensitivity Index, Treatment Credibility Scale, and five-facet mindfulness questionnaire | Mindfulness training reduced IBS symptom severity substantially and produced benefits that persisted for at least 3 months after the intervention. |
| Mohamadi et al.; 2019 (19) | Iran | 76 | Female and male | Dialectical behavior; therapy, mindfulness-based cognitive therapy, and positive psychotherapy | without any intervention | Perceived stress; and quality of life | Perceived Stress Scale (PSS) and irritable bowel syndrome quality of life (IBS-QOL) | In the mindfulness group, sleep quality was significantly improved compared to the control group, and levels of PS were significantly lower for the MBC intervention compared with the other groups. |
| Ghandi et al.; 2018 (23) | Iran | 24 | Female and male | Mindfulness-based stress reduction therapy with emotion regulation treatment | Without any intervention (no psychological intervention) | Quality of life and IBS symptoms | Irritable bowel syndrome quality of life (IBS-QOL) and Questionnaire of Severity of Bowel Symptoms (IBS-SSS) | MBSR improved the quality of life of IBS patients and dicreased severity of their condition |
| Zernicke et al.; 2012 (24) | Canada | 90 | Female and male | Mindfulness-based stress reduction | Waiting list | IBS symptom severity, stress,mood, quality of life (QOL), and Spirituality Scales | IBS Severity Scoring System (IBS-SSS), irritable bowel syndrome quality of life (IBS-QOL), Profile of mood states; (POMS), the Calgary Symptoms of Stress Inventory (C-SOSI), FunctionalAssessment of Chronic Illness Therapy—Spiritual Well-being (FACIT-sp) Scale | Mindfulness intervention; reduced IBS symptom severity and symptoms of stress |
| Ljótsson et al.; 2011 (25) | Sweden | 85 | Female and male | Long-term follow-up of internet-delivered exposure and mindfulness-based treatment for irritable bowel syndrome | Waiting list | IBS symptoms, quality of life, and anxiety related to gastrointestinal symptoms | Standardized self-report measures of the Gastrointestinal Symptom Rating Scale (GSRS-IBS), irritable bowel syndrome quality of life (IBS-QOL), and The Visceral Sensitivity Index (VSI) | Mindfulness intervention reduced IBS symptoms and improved the quality of sleep. |
| Garland et al.; 2012 (26) | USA | 75 | Female | Mindfulness-based treatment for IBS | Support group intervention | IBS severity, IBS-Related quality of life, dispositional mindfulness, pain catastrophizing, visceral sensitivityreinterpretation of pain sensations, psychological distress | The Irritable Bowel Symptom Severity Scale (IBS-SS), the IBS-quality of life (IBS-QOL) scale, the five facet mindfulness Questionnaire (FFMQ), the Coping Strategy Questionnaire (CSQ), the Visceral Sensitivity Index (VSI), reinterpreting pain sensations subscale of the CSQ, the Brief Symptom Inventory-18 (BSI-18) | Mindfulness significantly improved patients' symptoms and quality of life. |
| Naliboff et al.; 2020 (18) | USA | 68 | Female and male | Mindfulness-based stress reduction | There was no control group | GI symptom severity, quality of life, and GI-specific anxiety | The IBS Severity Scoring System (IBS-SSS), the IBSQOL, the Visceral Sensitivity Index (VSI), the Five Facet Mindfulness Questionnaire (FFMQ), and the Hospital Anxiety and Depression (HAD) Scale. | Mindfulness improved GI symptoms and associated problems in participants with IBS. |
| Dehkodi et al.; 2014 (27) | Iran | 30 | Female and male | Mindfulness-based stress reduction | drug therapy | Quality of life | Quality of life questionnaire for patients with irritable bowel syndrome (QOL-IBS) | MBSR improved the quality of life of IBS patients |
| Ljótsson et al.; 2010 (28) | Sweden | 86 | Female and male | Internet-delivered exposure and mindfulness-based therapy for irritable bowel syndrome | An online discussion forum | IBS-symptom Severity, IBS-related quality of life, GI-specific anxiety, depression, and general functioning | GSRS-IBS, IBS-QOL, VSI, MADRS-S, the Sheehan Disability Scales, and the GI symptom diary | Mindfulness delivered via the Internet effective treated IBS patients alleviated the total burden of symptoms and increased the quality of life. |
| Zomorrodi et al.; 2015 (29) | Iran | 24 | Female and male | Mindfulness-based therapy (MFT) for IBS patients | Without any intervention | Quality of life | IBS-QOL-34 (Quality of Life) Questionnaire | Mindfulness was influential on the life quality of patients suffering from IBS. |
| Zomorrodi et al.; 2015 (29) | Iran | 36 | Female and male | Cognitive-behavioral therapy and mindfulness therapy | The control group underwent medical therapy, and no psychological therapy was done in this group. | Quality of life, IBS-symptom severity | Coping ways questionnaire of Lazarus & Folkman, Bowel Syndrome Quality of Life Questionnaire (IBS-QOL-34), ROMEIII Criteria (IBS Symptoms Index) | Mindfulness-based therapy was more effective in reducing symptoms and quality of life in the follow-up stage than cognitive-behavioral therapy. |
| Harding et al.; 2018 (30) | USA | 55 | Female and male | Mindfulness-based stress reduction | There was no control group | PTSD, IBS, GSA, and depression symptoms | 17-item PTSD Checklist—Civilian Version (PCL-C), DSM-IV (Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition), Irritable Bowel Severity Scoring System (IBS-SSS), 15-item Visceral Sensitivity Index (VSI), the Patient Health Questionnaire 9-Item Depression Scale (PHQ-9), the 39-item Five Facet Mindfulness Questionnaire (FFMQ). | Veterans reported reduced trauma-related, irritable bowel, GSA, and depression symptoms and greater mindfulness skills immediately post-treatment |
| Mohammadi et al; 2021 (31) | Iran | 30 | Female and male | Integrating cognitive-behavioral therapy and mindfulness therapy | Without any intervention | Lifestyle | Lifestyle Questionnaire (LSQ) | Integrating cognitive-behavioral therapy and mindfulness therapy effectively improved lifestyles in women with IBS. |
| Shakernejad et al.; 2015 (32) | Iran | 3 | Female and male | Mindfulness-based stress reduction | There was no control group | Anxiety and Depression | Beck Anxiety Inventory (BAI) and Beck Depression Inventory-II (BDI-II) | MBSR reduces depression and anxiety symptoms post-treatment |
| Gol et al.; 2021 (33) | Iran | 45 | Female | Mindfulness-based cognitive therapy and neuro feedback | Without any intervention | Quality of life | WHOQOL-BREF | MBCT was only effective in the improvement of general health in comparison with the control group. |
| Dabaghi Zarif et al.; 2021 (34) | Iran | 24 | Female | Stress-based mindfulness training | Without any intervention | Quality of Life Scale | Quality of life questionnaire 1998 | reduce the amount of stress in women and increase the level of mental health and quality of life |
| Eskafi Sabet et al.; 2022 (35) | Iran | 30 | Female and male | Mindfulness-based cognitive therapy (MBCT) | Without any intervention | Quality of life | Short Quality of Life Scale (SF-36) | Mindfulness-based cognitive therapy is effective in reducing symptom severity and increasing the quality of life |
| Patange et al.; 2023 (36) | India | 95 | Female and male | Mindfulness based stress reduction | There was no control group | Quality of life | IBS-QOL-34 | IBS patients with MBSR showed significant improvement. Degrees of improvement are solely dependent on emotional control, acceptance of thoughts and reality, and patience. |
| Gaylord et al.; 2011 (22) | USA | 76 | Female | Mindfulness training | Social-support group intervention led by master’ s level social workers | IBS-QOL-34 | IBS-QOL-34 | Mindfulness Training effect on bowel symptom severity, improves health-related quality of life, and reduces distress |
3.9. Assessment of Bias
To evaluate the quality of the studies, a modified version of Verhagen's checklist (37), specifically designed to assess the quality of clinical trial studies, was employed. Two researchers independently conducted qualitative assessments of all studies that met the inclusion criteria, and any discrepancies in evaluations were resolved through discussion and analysis until a consensus was reached.
3.10. Evidence Evaluation
The GRADE approach was used to evaluate the overall quality of evidence in this study. The quality of evidence was categorized as high, moderate, low, or very low, considering factors such as inconsistency, indirectness, and imprecision.
3.11. Analysis Method
STATA 17 software was used for the analysis. Heterogeneity was assessed using the I² criterion, considering the study design and quality assessment scores for subgroup analysis. Publication bias was examined using the Egger test. Additionally, a meta-regression analysis was performed to explore the impact of various factors on treatment effects related to quality-of-life heterogeneity. Statistical tests yielding P-values less than 0.05 were considered statistically significant.
4. Results
4.1. Selected Studies
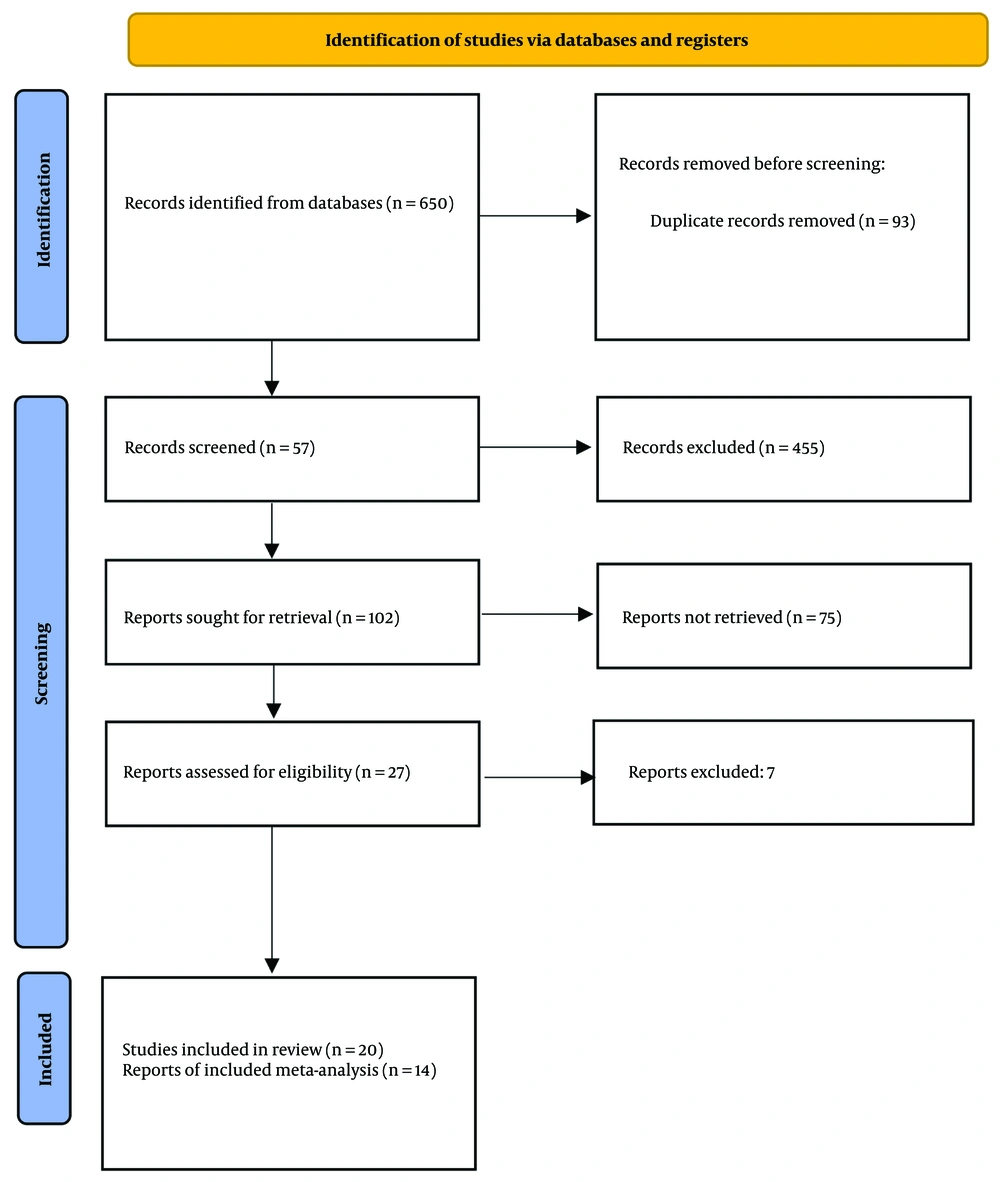
Following an extensive search in the aforementioned databases, 20 studies were included in the qualitative section, and 14 studies were included in the quantitative synthesis of our work. Articles were excluded based on the following criteria: Availability in two languages, lack of full-text accessibility, evaluation of anxiety through vital signs, inappropriate methodology, and interference with other treatment methods, such as cognitive-behavioral therapy, during the screening process (Figure 1).
PRISMA 2020 flow diagram for reviews, which included searches of the database (38)
4.2. Characteristics of the Included Studies
Following the initial assessments, the systematic review included 20 studies that met the inclusion criteria, while the meta-analysis encompassed 10 studies. The published articles spanned from 1970 to May 2024, with sample sizes ranging from 3 to 95 patients. The study participants included both men and women diagnosed with IBS (Table 1).
We evaluated all the articles included in the meta-analysis using the Verhagen checklist. It was determined that 3 studies displayed a high risk of bias, 12 studies were of moderate quality, and the remaining studies exhibited a low risk of bias. The primary limitation affecting the overall quality of the evaluated studies was that most did not explicitly mention whether blinding procedures were implemented for evaluators and participants during the research (Table 2).
| Authors; Year | 1- Was A Method of Randomization Performed? | 2- Were the Groups Similar at Baseline? | 3- Were the Eligibility Criteria Specified? | 4- Is a Sample Size Justification Described? | 5- Was the Patient Blinded? | 6- Was the Care Provider Blinded? | Score | Risk of Bias |
|---|---|---|---|---|---|---|---|---|
| Henrich et al.; 2020 (17) | 1 | 1 | 1 | 1 | 0 | 0 | 4 | Moderate risk of bias a |
| Mohamadi et al.; 2019 (19) | 1 | 1 | 1 | 0 | 0 | 0 | 3 | Moderate risk of bias |
| Ghandi et al.; 2018 (23) | 1 | 1 | 1 | 0 | 0 | 0 | 3 | Moderate risk of bias |
| Zernicke et al.; 2012 (24) | 1 | 1 | 1 | 0 | 0 | 0 | 3 | Moderate risk of bias |
| Naliboff et al.; 2020 (18) | 0 | 1 | 1 | 0 | 0 | 0 | 2 | High risk of bias b |
| Dehkordi et al.; 2014 (27) | 1 | 1 | 1 | 0 | 0 | 0 | 3 | Moderate risk of bias |
| Ljótsson et al.; 2010 (28) | 1 | 1 | 1 | 1 | 0 | 0 | 4 | Moderate risk of bias |
| Ljótsson et al.; 2011 (39) | 1 | 1 | 1 | 0 | 0 | 0 | 3 | Moderate risk of bias |
| Zomorrodi et al.; 2015 (29) | 1 | 1 | 1 | 0 | 0 | 0 | 3 | Moderate risk of bias |
| Mohamadi et al.; 2019 (19) | 1 | 1 | 1 | 1 | 0 | 0 | 4 | Moderate risk of bias |
| Gol et al.; 2021 (33) | 1 | 1 | 1 | 1 | 0 | 0 | 4 | Moderate risk of bias |
| Gaylord; 2011 (22) | 1 | 0 | 1 | 0 | 0 | 0 | 2 | High risk of bias |
| Dabaghi Zarif et al.; 2021 (34) | 1 | 1 | 1 | 0 | 0 | 0 | 3 | Moderate risk of bias |
| Eskafi Sabet et al.; 2022 (35) | 1 | 1 | 1 | 1 | 0 | 0 | 4 | Moderate risk of bias |
| Patange et al.; 2023 (36) | 1 | 1 | 1 | 1 | 1 | 1 | 6 | Low risk of bias c |
| Eskafi Sabet et al.; 2022 (35) | 1 | 1 | 1 | 1 | 1 | 1 | 6 | Low risk of bias |
| Gaylord et al.; 2011 (22) | 1 | 1 | 1 | 1 | 1 | 1 | 6 | Low risk of bias |
a 3 - 4: Moderate risk of bias.
b 0 - 2: High risk of bias.
c 5 - 6: Low risk of bias.
4.3. Quality of Life (Primary Outcome)
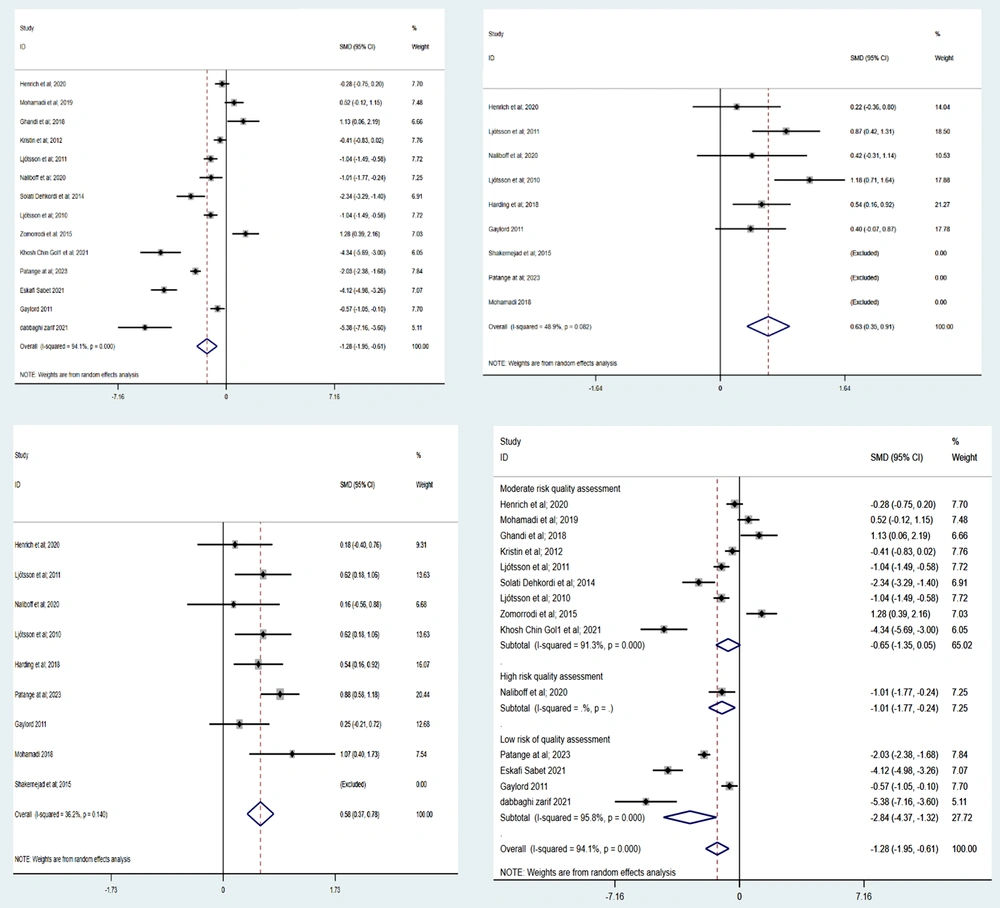
A random-effects model was used to calculate the combined effect size of the mean quality of life scores before and after the intervention. The overall analysis demonstrated that mindfulness-based interventions led to a significant improvement in quality of life within the intervention group (SMD = -0.683, 95% CI = -1.27, -0.608, P = 0.000) (as shown in Table 3). However, substantial heterogeneity was observed in this analysis. To address this, subgroup analyses were conducted, considering factors such as gender, target group, study design, and the qualitative evaluation of the studies (Table 3 and Figure 2).
| Variables | Number of Studies | Heterogeneity Chi-squared | P-Value | Overall, I-Squared; (%) | z | P-Value |
|---|---|---|---|---|---|---|
| Total result (primary outcome) | ||||||
| Quality of life | 14 | 220.71 | 0.000 | 94.1 | 3.74 | 0.000 |
| Subgroup analysis according to "quality assessment." | ||||||
| High risk of bias | 1 | 0 | 0.000 | 94.1 | 2.59 | 0.069 |
| Moderate risk of bias | 10 | 91.3 | 0.000 | 1.82 | 0.01 | |
| Low risk of bias | 4 | 95.8 | 3.6 | 0.000 | ||
| Secondary outcomes | ||||||
| Anxiety | 6 | 9.78 | 0.08 | 48.9 | 4.40 | 0.000 |
| Depression | 8 | 10.97 | 0.1 | 36.2 | 5.49 | 0.000 |
The effect of mindfulness on quality of life was investigated within each subcategory. As shown in Table 3, these analyses did not result in a significant reduction of the observed heterogeneity. Consequently, a meta-regression was performed to explore the potential impact of various factors on the heterogeneity of mindfulness effectiveness in improving the quality of life for patients with IBS.
4.4. Secondary Outcomes (Effect of Mindfulness on Anxiety and Depression)
Four studies addressing depression outcomes and four studies focusing on anxiety outcomes were included in the meta-analysis. Using a random-effects model, the analysis of secondary outcomes showed that mindfulness-based therapy significantly reduced depression (SMD = 0.57, 95% CI = 0.37, 0.87) and anxiety (SMD = 0.63, 95% CI = 0.35, 0.91) in patients with IBS (Table 3).
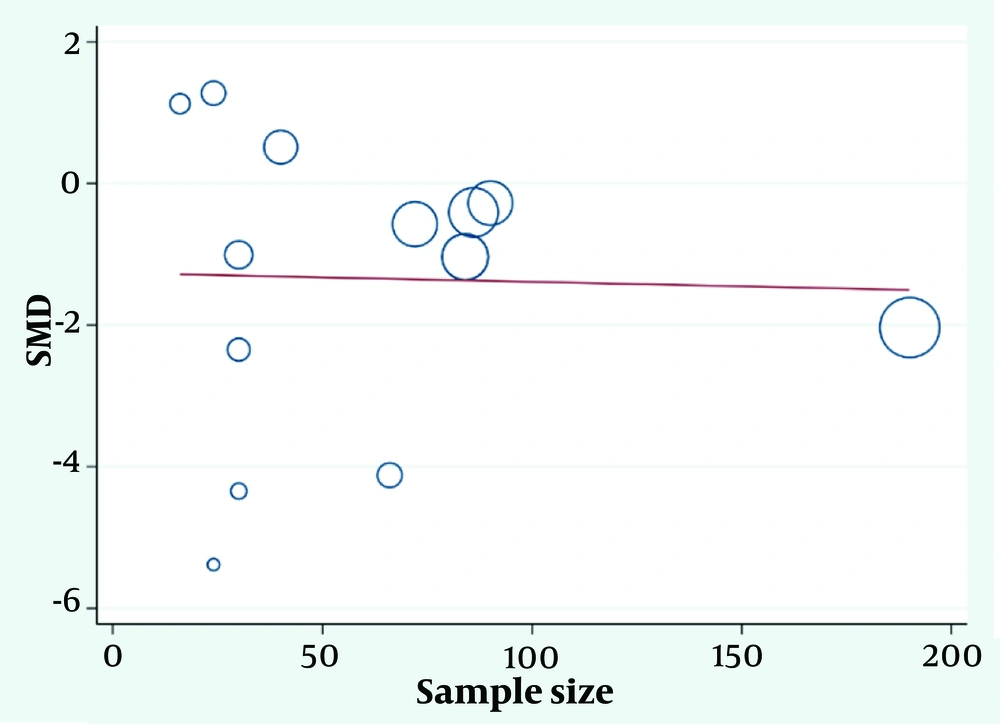
4.5. Meta-Regression
Cochrane's meta-regression approach was employed to examine the influence of potential factors on the heterogeneity of mindfulness effectiveness in enhancing the quality of life for patients with IBS. The results indicated that as the sample size increased, the average effectiveness score of mindfulness-based therapy in improving quality of life decreased, although this decrease was not statistically significant (P = 0.92) (Figure 3).
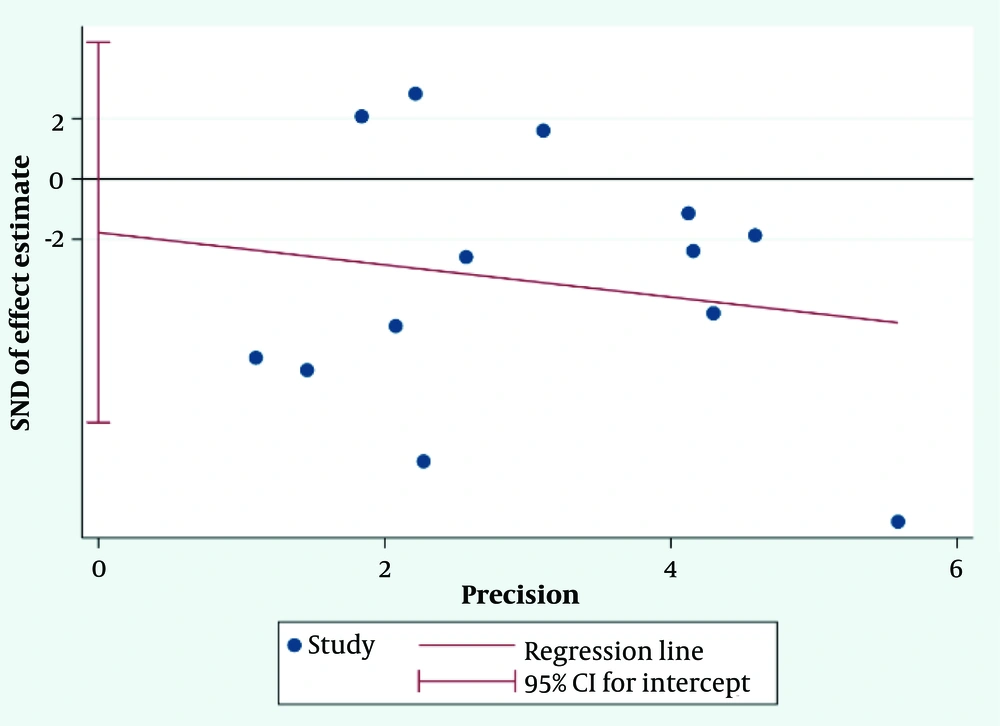
4.6. Publication Bias
Figure 2 shows that the distribution of studies is not uniform on both sides of the funnel. The results of the Egger test (P = 0.55) further confirm the existence of non-negligible bias (Figure 4).
4.7. Assessment of Evidence Quality using the GRADE Approach
The GRADE approach was used to assess the strength of evidence derived from the final results. The quality of evidence was classified into four categories: Risk of bias, stability, directness, and precision. A detailed description of these categories is provided in Table 4.
| Subgroups | The Number of Studies | Effect Size; SMD (95% ci) | Precision | Directness | Stability | Risk of Bias | Overall Quality Assessment |
|---|---|---|---|---|---|---|---|
| The quality of life in IBS patients | 14 | -1.277 (- 1.94,0.60) | Medium | High | Medium | Medium | Medium |
| Anxiety in IBS patients | 6 | 0.63 (0.35 ,0.91) | Medium | High | Medium | Medium | Medium |
| Depression in IBS patients | 8 | 0.57 (0.37, 0.78) | Medium | High | Medium | Medium | Medium |
5. Discussion
The findings of this systematic review, which included 16 studies in the quantitative and qualitative synthesis, indicated that mindfulness-based therapy is effective in improving the quality of life for individuals with IBS, while also reducing symptoms of depression and anxiety. Considering the potentially detrimental consequences of pharmacological treatments for these patients, it is crucial to prioritize the use of therapeutic and non-pharmacological interventions, such as mindfulness-based therapy.
Recently, IBS has been classified as a mind-body illness, with people experiencing significant mental health comorbidities (40). The present study aimed to examine the potential benefits of mindfulness training on the quality of life, anxiety, and depression in individuals diagnosed with IBS. The findings revealed that the application of mindfulness techniques in this population led to a significant improvement in their quality of life. Several studies have corroborated this finding. For instance, a study conducted by Martin et al. in 2019 demonstrated that after six weeks, mindfulness-based cognitive therapy effectively improved quality of life (41). Furthermore, aligning with our research, Dehkordi et al's findings indicated that MBSR therapy enhanced the quality of life (27). It appears that the mechanism underlying the improvement in quality of life is the reduction of IBS symptoms.
In the present study, the results also demonstrated that mindfulness training effectively reduced anxiety levels in patients with IBS. In similar studies, the results showed that anxiety was significantly reduced in both the short and long term. This is consistent with a previous review, which found that anxiety was the only outcome consistently impacted by mindfulness interventions at both brief and long-term follow-ups (40, 42).
This finding aligns with previous research, such as Taghvaeinia et al.'s study, which showed that MBSR led to a significant decrease in IBS symptoms, anxiety, and depression levels (43). Similarly, Mohammadi's study concluded that eight sessions of mindfulness-based cognitive therapy have the potential to reduce the severity of anxiety in IBS patients (44). Several studies have demonstrated the efficacy of mindfulness in alleviating depression severity in patients with IBS. These findings further underscore the potential benefits of integrating mindfulness practices into the treatment plans for individuals diagnosed with IBS, ultimately enhancing their mental well-being and overall quality of life (32, 43, 44).
In alignment with our findings, Teasdale, Segal, and Williams (2000) emphasized that the attention control skills acquired through mindfulness practice can be beneficial in reducing depressive symptoms and preventing the recurrence of depressive episodes. This effect occurs as patients learn to observe their thoughts and emotions without judgment throughout treatment, viewing them as transient mental events that come and go. Ultimately, individuals learn to avoid becoming trapped in rumination and worry, which can contribute to depression and anxiety (45).
The level of heterogeneity observed in this study is significantly high, a common occurrence in meta-analyses and systematic reviews. Methodological disparities, such as differences in blinding, randomization, or outcome measurement techniques, can contribute to variations in intervention effectiveness, thus causing heterogeneity (46, 47). This investigation highlights the diverse designs of the included studies, methodological disparities, potential biases due to a lack of blinding, differences in individual patient characteristics, and the disregard for disease severity as significant factors contributing to the high heterogeneity.
5.1. Limitations
Despite the findings, several factors should be considered when interpreting and generalizing the results. Most of the included studies were of moderate quality, except for one that exhibited a high risk of bias. The lack of blinding in these studies, and the resulting biases, may have impacted the validity of the findings and efficacy assessments. Comparing the intervention groups with control or placebo groups would have provided more accurate results, but this aspect was not explored in our study. Another limitation was the exclusive inclusion of English and Persian-language publications, potentially overlooking relevant studies in other languages, which may have influenced the overall effect size observed.
5.2. Conclusions
The results of this study demonstrated that mindfulness-based therapy effectively enhances the quality of life for individuals with IBS, while also reducing symptoms of depression and anxiety. Given the adverse effects of pharmacological treatments for these patients, prioritizing therapeutic and non-pharmacological methods, such as mindfulness-based therapy, is crucial for their overall well-being. Future research should aim to address the limitations of the current study and further explore the potential benefits of mindfulness-based interventions for individuals with IBS.