1. Background
Pain is an unpleasant experience about which people complain (1). For patients, it is the most important problem after surgery (2). Pain is a complex, multifactorial experience manifested as an unpleasant feeling (3, 4). Postoperative pain could exert adverse effects on the patient’s condition such as avoiding movement, coughing and deep breathing to prevent pain. This can entail many complications, including deep vein thrombosis, pulmonary embolism, sleep disturbance, atelectasis, ischemic myocardial infarction, respiratory infection, immune system disorders, and anxiety (5, 6). Pain is one of the most common causes of delay in discharge after surgery (7). Over 70% of patients experience moderate to severe pain following surgery, and more than 25% of individuals develop side effects after taking pain medications (8).
The most common cause of orthopedic problems is associated with road traffic accidents, which have a staggering rate in Iran. Patients with extremity trauma experience severe pain in their bones and soft tissues. About 50% of these patients report moderate to severe pain in the hospital. In fact, the main complaint of orthopedic patients of all ages and conditions is pain (9-12). Pain control is especially important in these individuals because its failure can lead to delay and restriction of joint movements (8, 13). Despite the high prevalence of acute postoperative pain and significant progress in understanding the pathophysiology of pain and its therapeutic approaches, patients often receive medication and are rarely provided with non-pharmacological pain therapy (14). Since medication could have many side effects, other pain management techniques are growing more popular. There are many non-pharmacological methods for pain relief, including relaxation, distraction, thermotherapy, cryotherapy, and transcutaneous electrical nerve stimulation (TENS) (15). With regard to its great range of frequencies and intensities, TENS has been increasingly administered to relieve pain (16, 17). There are numerous studies on pain relief through TENS, which have reached different results. Systematic review studies examining the impact of TENS on acute pain have not obtained identical results and, to date, there is no general consensus in this regard, such that a number of authors have supported TENS, but others have dismissed it (18-21). In Iran, several studies have been done into the effect of TENS on acute pain control (post-cesarean pain, pain during the insertion of peripheral venous catheter, burn dressing change, and subcutaneous injection pain) (22-28). However, no research has so far addressed the use of TENS in patients with bone fracture. Moderate-to-severe postoperative pain in these patients is frequently reported due to damage to the bone tissue and surrounding soft tissues. Nowadays, the most common approach to controlling pain during and after surgery is to administer injectable opioids, which can give rise to many cardiovascular and respiratory complications. Patients with bone fracture who are hospitalized in the orthopedic ward appear to be one of the high-risk groups for postoperative pain and opioid side effects (7).
2. Objectives
Thus, the present study was conducted to compare the effect of TENS and routine care on pain relief in patients with bone fracture.
3. Methods
This clinical trial included an intervention and a control group. The statistical population consisted of all patients with bone fracture admitted after surgery to the orthopedic ward of Khatam al-Anbia Hospital in Zahedan. The inclusion criteria were patient’s consciousness, age above 18 years, no pacemaker, no dangerous arrhythmias, no diabetes, no addiction, not taking any painkiller 6 hours before the intervention, having pain, no pregnancy, no eczema, and passage of at least 24 hours after surgery. Based on the risk of type I error (5%) and the test power of 80%, the authors estimated the sample size of 40 for each group (s1 = 0.48, s2 = 0.56 and x1 = 5.4, x2 = 7).
After obtaining the ethics code (IR.ZAUMS.REC.1396.151) and necessary permits from Zahedan University of Medical Sciences, the researcher conducted sampling by referring to the orthopedic ward of the abovementioned hospital. Prior to the study, the patients were informed of the purpose of the project and their written consent was obtained. Convenience sampling was adopted to recruit patients, who were then randomized into an intervention and a control group based on 80 blue and red cards.
Data collection was carried out through a demographic questionnaire and a visual analog scale (VAS). The scale consists of a 10-cm-long line that represents the continuous spectrum of pain experience, ranging from “no pain” on the left end to “worst pain” on the right end. After completing the demographic questionnaire, the participants were asked to indicate their pain intensity on the scale. The validity and reliability of the tool have been established in numerous studies (29, 30). Gallagher et al. (31) reported VAS as a valid and reliable scale (ICC: 0.99), and in another study, the reliability of VAS was reported 0.88 (32). At first, pain was assessed in the both groups using VAS. Then, high-frequency TENS was implemented in the intervention group. To this end, the TENS PM70 physiotherapy device (Arman Pouya Co., Iran) was used. Initially, 10 cm of both sides of the fracture were cleaned with cotton and alcohol. The electrode pads were then inserted, and the device was set at a frequency of 100 Hz and current of 10 - 30 amperes. The intervention lasted for 30 minutes. In the control group, the routine care of the ward was provided. After 30 minutes, VAS was used to measure pain in the both groups for the second time.
Once collected and codified, the data were analyzed in SPSS 21 using descriptive and inferential statistics. Before analysis, normality of data distribution was assessed using the Shapiro-Wilk test. Frequency, percentage, mean, standard deviation, minimum, and maximum values were initially calculated. A paired t-test was used to compare the mean scores of each group before and after the experiment. Furthermore, an independent t-test was employed to compare the mean scores between the two groups before and after the experiment. P values below 0.05 were considered statistically significant.
4. Results
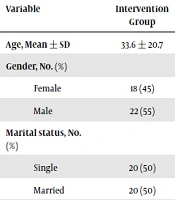
There was no significant difference between the two groups in terms of age, gender, ethnicity, and marital status (Table 1). Similarly, comparison of the mean scores of pain intensity in the two groups showed no significant difference prior to the experiment. However, a significant difference occurred in the mean pain intensity between the two groups after the experiment, with the intervention group reporting less pain (P < 0.001). Additionally, comparing pain intensity before and after the experiment revealed a significant relief only in the intervention group (P < 0.001) (Table 2).
aIndependent t-test
bChi-squared test
5. Discussion
The results of the present study demonstrated the effectiveness of TENS after orthopedic surgery. Investigating manual therapy and TENS in patients with neck pain, Escortell-Mayor et al. (33) observed that TENS helped reduce pain, increase the ability to perform daily tasks, and, consequently, improve quality of life. Vance et al. (34) found that TENS could improve the pain tolerance threshold in patients with knee osteoarthritis. In Brazil, Pitangui et al. (35) explored the efficacy of low- and high-frequency TENS on pain relief after episiotomy and compared their respective effects with those of placebo TENS. After analyzing the data, it was concluded that low- and high-frequency TENS could be effective in controlling episiotomy pain. Siavoshi et al. (24) investigated the effect of TENS on pain intensity during dressing change in 60 patients admitted to a burn center in Sabzevar, Iran. The intervention group received morphine and TENS, and the control group was provided with morphine and placebo TENS. At the end of dressing, the patients’ pain was re-measured using a numerical pain scale, and it was shown that the combined use of TENS and morphine could help alleviate pain in burn patients during dressing change. Asgari et al. (23) examined the effect of three kinds of TENS on pain associated with peripheral venous catheter insertion in 80 patients admitted to the internal ward and the CCU of Fatemieh Hospital in Semnan, Iran. They concluded that high-frequency TENS as well as burst-mode TENS allayed pain but low-frequency TENS could not produce this impact. Breit and Van der Wall (36) probed the effect of TENS on pain relief after total knee arthroplasty. The results suggested no significant difference in the need for patient-controlled painkiller with or without TENS, meaning that TENS was not useful for relieving pain after knee arthroplasty (36). It appears that the intensity (amplitude), duration, and frequency of pulse vary in different studies, which may be one of the causes for inconsistency in research findings (16, 22, 37).
In the present research, there was a significant difference in the mean of pain relief after the intervention between the two groups, such that individuals receiving TENS reported a significantly lower pain score. Conversely, patients in the control group did not show a substantial decrease in their pain score at the end of the study. The significant difference between the mean intensity in the two groups not only indicates the usefulness of the TENS method but also indicates the low efficiency of the routine method in reducing the pain in patients.
In this study, opioid analgesics were used ‘when required’ (PRN) whereas non-opioid analgesics were administered at regular intervals (every 8 hours). These two methods of analgesic administration have been criticized in some studies (38). Although TENS is one of the pain relief methods reported in some studies, the significant difference in mean pain intensity between the two groups of TENS and routine care in this study may indicate the need and more attention of health personnel in acute pain relief of patients (39).
5.1. Conclusions
The results of this study illustrated that TENS was effective in mitigating postoperative acute pain in patients with bone fracture but routine care methods were not sufficient in reducing pain. Therefore, it is recommended to adopt TENS as a low-risk method to lower patients’ pain. Moreover, according to the results, healthcare providers urgently need to upgrade routine methods of pain management in hospitals.