1. Background
End-stage renal disease (ESRD) is a condition that puts the patient at risk of death, this is due to the inability of the kidney to discharge waste and maintain fluid and electrolyte balance by causing uremia (1). Although the best treatment for these patients is kidney transplant, it is not a feasible method due to the lack of enough kidney donations. As a result, hemodialysis (HD) is currently the most common treatment for patients with ESRD in most countries (2). The goal of hemodialysis is to approximate patient’s life to normal conditions as much as possible (3). The global prevalence of chronic kidney disease (CKD) in 2012 was 242 per million, and it was estimated to annually rise by 8% (4). Similarly, five years earlier in 2007, the prevalence of renal failure was high around the world, including Iran (5). Since treatment with hemodialysis is a long-term process, it can lead to many complications, including arterial hypertension, anorexia, anemia, inability to concentrate for a long time, renal osteodystrophy, reproductive system diseases, skin disorders, and arteriovenous access infection, all of which can impair the patient’s quality of life (6).
There is compelling evidence demonstrating that the best healthcare outcomes are achieved when patients are actively engaged in caring for themselves. Self-care includes patient’s active participation in the treatment process by doing certain physical care activities. Tracking the treatment progress, monitoring symptoms, evaluating side effects, adopting positive health-related behaviors (such as having a healthy diet and regular exercise), and improving the patient’s general health are some of the more common activities in this regard that will ultimately lead to a reduction in medical costs (7-9). Serving as one of the integral therapeutic components for HD patients, self-care could include daily self-weighing, following the prescribed diet, using proper fluids and medications, fistula care, and avoidance of heavy work (10, 11). Such activities can play a remarkable role in helping patients adapt to the disease process, promoting quality of life, modifying behaviors, accepting treatment and, thereby, improving physical and mental health (12, 13). Studies have indicated that people with high self-care skills have a greater potential to rehabilitate and maintain their independence (14, 15). Despite the role of self-care in the management of CKD, most individuals with this condition have difficulty caring for themselves owing to complex therapeutic regimens as well as physical and psychological limitations of the disease (16). Therefore, any restriction on self-care activities could be directly associated with the patients’ mortality (17). Various levels of self-care in HD patients have been reported around the world (18-21). Self-care activities in these patients can play a major role in improving their quality of life (21), reducing the length and frequency of hospitalization, and lowering medical costs as well as mortality rates (22). Treating these patients without their own participation and doing certain self-care activities may not be sufficiently effective and will not produce the desired outcomes (23). Since nurses, compared to other members of the treatment team, are most in touch with patients during hemodialysis, they can greatly assist in establishing a continuous and dynamic relationship with patients to improve their awareness and self-care behaviors (24). One of the methods of teaching HD patients after discharge is telenursing, i.e., nursing interventions conducted by means of communication media. This technique saves patients’ time and provides the opportunity to educate them remotely. Thus, patients, especially those living in rural areas, are no longer obliged to travel long distances and, consequently, both medical costs and self-referrals to the emergency department decrease (25). In general, telenursing is an efficient route for enhancing patient care and disease management (26).
Studies have indicated that telephone follow-up and tele-education by nurses lead to heightened self-care in patients (27, 28). Telenursing denotes the provision of nursing services through the use of information technologies. These technologies can include telephone, computer, remote monitoring tools, and the Internet. The use of telenursing has enabled nurses to perform tasks such as patient monitoring and education, certain nursing interventions, and pain control. Among the telecommunications equipment used in this area, telephone is the most widely used device, which is available to most people (29). Telenursing strengthens the relationship of the patient and nurse and allows for the provision of health services regardless of time or place. Using this technology results in faster and easier access to better (specialized) services, lower costs, and an all-inclusive growth in the quality of patient care (30). Previous studies have reported the positive effects of telenursing on self-care in patients with hypertension, diabetes, and heart failure (31-33).
2. Objectives
The purpose of this study was to determine the effect of telenursing on self-care behaviors of patients undergoing hemodialysis at Ali Ibn Abitalib Hospital in Zahedan in 2019.
3. Methods
After obtaining the required permissions from the Ethics Committee of Zahedan University of Medical Sciences (code: IR.ZAUMS.REC.1397.374), the researchers performed this clinical trial on patients undergoing hemodialysis at Ali Ibn Abitalib Hospital in Zahedan in 2019. Eighty HD qualified patients discharged from the Nephrology Ward were recruited using convenience sampling. Next, they were randomized to the experimental and control groups. A container with colored cards was used to determine the group each patient was to be assigned; individuals picking green cards were placed in the experimental group and those picking blue cards were allocated to the control group.
The eligibility criteria included: willingness to participate in the study, having a mobile phone for telenursing, verbal communication ability, undergoing hemodialysis at Ali Ibn Abitalib Hospital, hearing and speaking ability for question/answer purposes, hemodialysis initiation during the last year, and an age of 16 - 65 years. On the other hand, the exclusion criteria were: non-cooperation at any time during the study, lack of telephone accessibility for two weeks in the first month of the intervention or for three weeks in the second and third months of the intervention, as well as patient’s death, migration, or long-term travel.
Considering the mean and standard deviation (S1 = 3.04 and S2 = 2.87;
The [data collection] tools used in this study comprised a demographic questionnaire (age, gender, marital status, education, residence, occupation, hemodialysis history, number of dialysis sessions per week, vascular access, and etiology of CKD) and an 18-item questionnaire for assessing self-care behaviors in hemodialysis patients. The latter instrument was designed by Baghiani Moghadam et al. (10), by using the test re-test method, where we established the reliability (84%) of this scale. This questionnaire has 18 items that are scored based on a 5-point Likert scale: never (0), rarely (1), occasionally (2), often (3), and always (4). The highest score achieved on this tool is 72, indicating high levels of self-care capacity. The face and content validity of this instrument was confirmed in the present study by a panel of experts (three health education experts, a nephrologist, and one statistician). Using Cronbach’s alpha, Baghiani Moghadam et al. (10), confirmed the internal consistency (88%) of this scale.
The educational intervention by telephone was undertaken twice a week for 12 weeks each time for an average of 15 - 20 minutes. Depending on the subject's preference and to acquire more accurate answers, the researchers would make the telephone contacts from 8 AM to 8 PM, thus, offering the respondents a great flexibility. During phone calls, necessary instructions were given about diet, fluid intake, medication, fistula care, skin care, activity and rest, treatment follow-up, infection prevention, gastrointestinal problems, and reducing anxiety and stress. Each week, one topic was discussed based on the conditions of each single patient and the priority of their respective needs. The subjects were provided with the researchers’ phone numbers to ask their possible questions. In addition to phone calls, a text message was sent weekly to each patient in the intervention group regarding the above topics. At the end of the intervention, the patients were contacted and asked about the time when they would refer for hemodialysis. Upon referral, the experimental group was required to fill out the self-care questionnaire for the second time.
The control group received no instructions except for routine training; after three months, they completed the self-care questionnaire and their answers were compared with those of the experimental group. To abide by ethical considerations, the authors provided the control group with the educational booklet at the end of the study. Data were analyzed in SPSS-22 using chi-square test, independent t-test, paired t-test, and ANCOVA at the significance level of P < 0.05.
4. Results
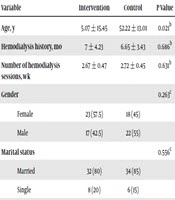
Eventually, 80 participants completed the study. The mean age of participants was 45.07 ± 15.45 years in the experimental group and 52.55 ± 13.01 years in the control group, indicating a significant difference between the two groups (P = 0.021). No significant difference occurred between the two groups with respect to gender, marital status, education, residence, employment, vascular access, cause of CKD, hemodialysis history, and the number of weekly hemodialysis sessions (Table 1).
| Variable | Intervention | Control | P Value |
|---|---|---|---|
| Age, y | 5.07 ± 15.45 | 52.22 ± 13.01 | 0.021b |
| Hemodialysis history, mo | 7 ± 4.23 | 6.65 ± 3.43 | 0.686b |
| Number of hemodialysis sessions, wk | 2.67 ± 0.47 | 2.72 ± 0.45 | 0.631b |
| Gender | 0.263c | ||
| Female | 23 (57.5) | 18 (45) | |
| Male | 17 (42.5) | 22 (55) | |
| Marital status | 0.556c | ||
| Married | 32 (80) | 34 (85) | |
| Single | 8 (20) | 6 (15) | |
| Education | 0.357c | ||
| Primary school | 22 (55) | 26 (65) | |
| Secondary school | 10 (25) | 5 (12.5) | |
| Above secondary school | 8 (20) | 9 (22.5) | |
| Residence | 0.606c | ||
| Urban | 29 (72.5) | 31 (77.5) | |
| Rural | 11 (22.5) | 9 (22.5) | |
| Occupation | 0.752d | ||
| Unemployed | 5 (12.5) | 7 (17.5) | |
| Housewife | 20 (50) | 16 (40) | |
| Self-employed | 11 (27) | 12 (30) | |
| Other (employee, retired, farmer) | 4 (10) | 5 (12.5) | |
| Vascular access | 0.478c | ||
| Permacath | 28 (70) | 25 (62.5) | |
| AVF, arteriovenous graft, and CVC | 12 (30) | 15 (37.5) | |
| Cause of CKD | 0.656c | ||
| Diabetes | 5 (12.5) | 8 (20) | |
| Hypertension | 15 (37.5) | 16 (40) | |
| Diabetes and hypertension | 11 (27.5) | 7 (17.5) | |
| Other | 9 (22.5) | 9 (22.5) |
Abbreviations: AVF, arteriovenous fistula, CVC, central venous catheter.
aValues are expressed as mean ± SD or No. (%).
bIndependent t-test.
cChi-square test.
dFisher’s exact test.
Controlling the effect of age (which was significantly different between the two groups) and considering the mean score of self-care before the intervention (as the intervening variable), we observed that the self-care scores differed significantly in the two groups [after the intervention] (P < 0.001).
There was no statistically significant difference between the two groups with respect to the mean scores of self-care at the beginning of the study (P = 0.121); with the experimental group scoring higher than the control group. In addition, the mean score of self-care in the experimental group increased from 24.40 ± 14.73 before the intervention to 48.65 ± 9.19 after the intervention P = < 0.001 (Table 2).
aValues are expressed as mean ± SD.
bPaired t-test.
cIndependent t-test.
5. Discussion
The results of this study revealed that the mean score of self-care in the group receiving telenursing was higher than the control group after the intervention. This positive impact could be related to the long duration of follow-up and continuous education based on the specific needs of each patient. There are some studies supporting the findings of the current research. For example, Ramazani et al. (34), reported the positive effect of education on self-care in HD patients. Consistent with these results, Evangelista et al. (35), explored the impact of remote monitoring systems on self-care and quality of life in older adults with heart failure. Their findings demonstrated the effect of these systems after a three-month follow-up. The nurse researcher contacted patients every 24 - 48 hours after discharge to ensure that they followed the instructions. The results suggested that educational interventions can potentially enhance problem-solving skills that enable patients to participate confidently in decision-making and take necessary steps to effectively manage their chronic health status. Thus, patients who received the intervention showed greater improvements in self-care activities and quality of life; this is in good agreement with the present study, except that Evangelista et al. (35), studied old patients with heart failure. In their systematic review, Madmoli et al. (36), assessed the effect of some factors on self-care in diabetic patients and reported that educational interventions could promote the self-care of these patients, such that they acquired greater control over their blood sugar. Another similar study by Ahmadi et al. (37), investigated self-care in diabetic patients and proposed that these individuals can improve their self-care behaviors by taking part in educational interventions. Furthermore, Hosseini and Ziaei Rad (38), examined the impact of telenursing through social networks on weight control and self-efficacy of HD patients and found that this intervention increased their subjects’ self-efficacy. While this report and the present study addressed different variables, they both agree that educational interventions bring positive effects on self-care.
Meanwhile, there are some other reports that contradict the findings observed in the present study. Comparing three methods of training self-care through video call, telephone, and routine care in patients with heart failure, Jerant et al. (39), found that the rate of readmission in the intervention groups plummeted significantly (80%), which is relative to the control group; nevertheless, no significant difference occurred in patients’ self-care indices at baseline and at the end of the study. It should be noted that the population investigated by Jerant et al. (39), is not the same as that of the current study.
Carlson et al. (40) examined the effectiveness of a healthy heart tracker in improving self-care among patients with heart failure; they observed that, compared to the control group, their intervention, involving a patient education booklet designed specifically for recovery, could not substantially change self-care behaviors over time. This is inconsistent with the results of the present study, which could be justified with respect to the high rate of attrition during the follow-up period in the study by Carlson et al. (40).
The impact of telenursing on self-care improvement in our research and other studies could be associated with continuous monitoring and follow-up of patients, which could help them learn how to cope with their illness and mitigate their disability. In addition, using telenursing, nurses can identify and help meet patients’ needs. Another factor involved in this improvement is the reduction in stress, anxiety, and depression as a result of increased self-esteem and ultimately self-care. Finally, thanks to telenursing, patient care may be transferred from clinics and hospitals to patients’ homes, thus, reducing medical costs.
5.1. Conclusions
The results of this study established that patient training and follow-up by telephone (telenursing) could boost self-care behaviors in hemodialysis patients. Given the wide availability of telephone and the low cost of education using this medium, healthcare providers and nurses can adopt telenursing to promote self-care in hemodialysis patients. In addition, telenursing is an effective and convenient method for training other chronic patients, especially for those who live in rural areas and have no access to treatment centers.