1. Background
Thalassemia is a genetic disorder that is manifested by impaired production of the globin chain (1). In patients with beta-thalassemia, the production of the beta-globin gene either stops (β0 thalassemia) or decreases (+β thalassemia) (2). In 2007, the World Health Organization identified this disease as the most widespread chronic disorder with a genetic pattern in 60 countries, affecting the lives of approximately 100,000 children annually (3). In 2011, more than 2 million beta-thalassemia carriers and approximately 25,000 cases of beta-thalassemia major were reported in Iran (4). Sistan and Baluchistan province recorded the highest prevalence of thalassemia in Iran in 2010 (5). Like other chronic diseases, thalassemia brings about many problems for patients and their families. Frequent referral of these patients for blood transfusion can lead to lifestyle changes, frequent absences from school, reduced social activities, reduced self-esteem, feeling of inadequacy and inferiority due to being dependent on others, anger, disappointment, and fear of premature death. This condition exerts adverse effects on the mental health of other family members, as well (6). Parents of these patients feel guilty, frustrated, and worried about their children’s health as they consider themselves responsible for their illness (7). Since medical care and being worried about premature death prompt feelings of despair, indignation, loneliness, and stress, parents should work out appropriate coping strategies (adaptive behaviors) to improve their performance (8). In dealing with stressful events, like chronic and life-threatening illnesses, these strategies play a crucial role in ensuring one’s mental health (9). Adaptive behaviors include actions and reactions by an individual to control and manage the stress caused by a given situation. These behaviors need to be reinforced, especially in families taking care of sick children. Better adaptation can lead to a higher quality of life for the sick child (10). In this regard, Brannon et al. (11) showed that adaptive behaviors are effective ways to control and reduce the outcomes of diseases and help parents improve their quality of life. Parents of children with chronic and life-threatening illnesses use adaptive behaviors, such as positive thinking (12), information seeking (12), spirituality and religiosity (13), and social support (14) to cope with and accept the disease. The most common adaptive behaviors adopted by parents of children with thalassemia major are strengthening trust in God, decreasing social and recreational activities, and communicating with the spouse and relatives ((10, 15, 16). Adaptive behaviors proposed by McCubbin et al. (17) are particularly relevant to planning and clinical interventions. In this model, adaptive behaviors are classified into three patterns, including maintaining family integration and ameliorating the current situation; social support, self-esteem, and psychological stability; and understanding the medical state of the patient via communicating with parents of similar children and consulting with the medical team.
Caring for a sick child can place a great burden on family caregivers, especially mothers. The caregiver burden is accompanied by persistent hardship, stress, or negative experiences felt by the caregiver (18). This burden could give rise to an imbalance between patients’ caring needs and the caregiver’s other responsibilities, thus affecting the social, personal, physical, emotional, and financial roles of the caregivers (19). Chang et al. (20) revealed that people who spend more hours per day caring for their patients undergo a heavy burden and have relatively low mental health. The timely diagnosis of caregivers’ suffering plays a crucial role in promoting their health (21). As the main caregiver, mothers of sick children endure considerable psychological stress, which can transfer to other family members. In many societies, including Iran, mothers play a more active role in caring for sick children (22) and are more susceptible to psychological stress than fathers (6, 22). The results of the study by Andren et al. (23) demonstrated that providing instructions about adaptive behaviors was associated with a decrease in caregiver burden. Reviewing the results of previous studies on how to adapt to chronic illnesses and reduce caregiver burden suggests several coping strategies, such as group discussion training (24), individual training (25), and group counseling (26). Studies have regarded individual training methods to be effective because participants have enough time to express their problems (25, 27); meanwhile, Riyazi et al. (27) reported that female subjects taking part in group training felt more secure and less anxious than those attending the individual training program. People with similar problems prefer to share personal, family, and objective concerns and to benefit from others’ experiences in a trusted environment (28). This process enables them to cope with their situation and adapt to new changes (29).
Families having patients with chronic illnesses experience a difficult and stressful situation, and urgently need help and support (30). Nevertheless, healthcare providers commonly focus on patients and consider their families to play just an ancillary role in the treatment process. As a key aspect of family-based care, nurses have to support patients’ parents by raising their awareness and allowing them to better cope with the child’s disease (31).
Chiou et al. (18) observed that training could empower parents to relieve their caregiver burden and reinforce their coping strategies. Utilizing group education for families with chronic patients is an appropriate method since people will learn how to respond to different situations. Examples in this context might include catharsis, participating in support group programs, and training social skills (26). Although family members’ adaptation to the child’s chronic illness is fundamental in terms of health care, parents usually have little awareness of coping strategies. Besides, there is an urgent need for gathering credible evidence to identify educational needs, undertake interventions to improve adaptation to illnesses, and thus attain a greater quality of care (32). Kermansaravi et al. (15) study conducted in Zahedan indicated that parents, especially mothers, who had children with thalassemia major, often were not equipped with effective coping behaviors compared with parents with healthy children.
Given the controversial results regarding this subject and the significance of adaptive behaviors, as well as reducing caregiver burden on the one hand, and the high prevalence of patients with thalassemia in Sistan and Baluchistan Province (most of their parents lack effective coping behaviors and undergo a great burden taking care of their sick child) on the other hand, this study was conducted to assess the effect of group training on adaptive behaviors and caregiving burden of mothers of children with thalassemia major.
2. Objectives
The present study aimed at exploring the effect of group training on adaptive behaviors and caregiving burden of mothers of children with thalassemia major.
3. Methods
After obtaining the permission from the Ethics Committee of Zahedan University of Medical Sciences (no.: IR.ZAUMS.REC.1397.195), the researchers conducted this clinical trial on the mothers of children with thalassemia major who had been admitted at Ali Asghar Hospital in Zahedan in 2019. The subjects were selected through convenience sampling based on the inclusion criteria and randomly assigned to the intervention and control groups. A vase with colored cards was used to determine the group for each subject (green: intervention and blue: control). The inclusion criteria included being diagnosed with thalassemia for at least six months ago, reading and writing literacy, residing in Zahedan, living with the spouse, no responsibility to care for a patient in the family other than the thalassemic child, no known psychiatric disorder, and no use of psychiatric drugs. On the other hand, the exclusion criteria were being absent for more than one educational session, experiencing severe stressful events, such as the death of a family member, using drugs and sedatives, and taking part in other consultation therapies during the study.
The sample size was estimated at 28/69 based on the study by Salehi and Morovati (10) using the following formula with a confidence interval of 95% and the power of 95%. Considering the possible attrition of participants, eventually, 35 subjects were recruited for each group (n = 70).
Z1 - α/2 = 1.96; S1 = 3.82;
Data were collected using three research tools, including a demographic questionnaire, the coping health inventory for parents (CHIP), and the Caregiver Burden scale (CBS). Demographic information covered the child’s gender and age, ethnicity, mother’s age and education, economic status, health insurance, number of children, and parents’ occupation. The CHIP comprises 45 items. Parents were asked to mark behaviors that were true about them; besides, they were required to indicate the effectiveness of each behavior in helping them adjust to their child's illness. This was carried out using a four-point Likert scale (3, very useful; 2, relatively useful; 1, slightly useful; 0, not useful). If the behavior was not performed by the parents, they had to specify whether “it was impossible to practice” or “it was possible but was not practiced”. The adaptive behaviors of CHIP are classified into three subscales: “family integrity and situation improvement” (the first pattern; 19 items), “social support, self-esteem, and psychological stability” (the second pattern; 18 items), and “communication and medical counseling” (the third pattern; 8 items). The scores of adaptive behaviors in the first, second, and third subscales, and the entire inventory ranged from 0 to 57, 0 to 54, 0 to 24, and 0 to 135, respectively. McCubbin et al. confirmed the internal consistency of CHIP in two distinct studies (Cronbach’s alpha: 0.71 and 0.79) (16, 17). The Persian version of this instrument was standardized for the Iranian population, and its reliability and validity were established by Nikfarid et al. (16). In the current study, the reliability of CHIP was assessed based on Cronbach’s alpha coefficient (0.75).
The Caregiver Burden scale (CBS) was designed by Elmstahl et al. (33). It includes 22 items, which evaluate the pressure and stress resulting from caring for a patient with chronic disease (29). The CBS comprises 5 domains, including general burden (8 items suggesting that the caregiver is not free and experiences burden); loneliness (3 items implying restricted social interactions and having no time for oneself); disappointment (5 items indicative of loneliness and the experience of physical pain, the effect of financial problems, and believing that life is not fair); emotional involvement (3 items representing patient’s anger and feeling shame due to the disease); and environment (3 items indicating the lack of caregiving experience and inability to handle the patient’s problems). This instrument is scored according to a four-point Likert scale (1, never; 2, seldom; 3, occasionally; and 4, most often). The obtained score could range from 22 to 88, with higher scores suggesting more severe levels of caregiver burden. In Iran, the content validity of CBS has been reported 0.82; additionally, its reliability (0.86) has been corroborated using the internal correlation coefficient and Cronbach’s alpha (3). The reliability of this scale was also approved in the present study (Cronbach’s alpha: 0.81).
After grouping, the researchers telephoned the participants and filled out the questionnaires. The collected data were analyzed. Based on the pre-test results, ineffective coping behaviors were identified in mothers, and the educational content was designed accordingly. Mothers in the intervention group actively attended 4 consecutive sessions (one 120-min session per week) in 4 subgroups of 8 to 9 persons. Following making necessary coordination with the subjects, the group-based training program was conducted according to the approved content (Table 1) at the hospital on a specific day of the week. One month after the intervention, both groups completed the questionnaires for the second time. To observe the ethical considerations, the control group was provided with a training session by the researchers at the end of the study. During the sessions, mothers were encouraged to ask their questions and engage in group discussions. At the end of each session, the researcher and the psychiatric nurse summarized the materials. The subjects were asked to practice the presented skills at home; they were also provided with the researcher’s phone number for counseling and solving their possible questions. Data were analyzed using SPSS-22 and independent t-test, paired t-test, chi-square test, and Fisher’s exact test. P < 0.05 was considered statistically significant.
| Session | Topics |
|---|---|
| First | Introduction, providing instructions on the nature of the disease, its signs and symptoms, and their associated complications; diet; physical activity; taking care of a thalassemic child; relaxation training and practice; presenting the educational pamphlet containing the key points of the session; question and answer to ensure that the mothers were informed about the provided contents; providing mothers with a telephone number to ask possible questions. |
| Second | Reviewing the previous session with the active assistance of mothers; group discussion and encouraging mothers to express their experiences of taking care of their sick children; discussing relevant challenges and introducing problem-solving skills to overcome them; relaxation practice; question and answer to ensure that the mothers were informed about the provided contents. |
| Third | Reviewing the previous session; group discussion about the stress, anger, and anxiety management strategies; relaxation practice; question and answer to ensure that the mothers were informed about the provided contents. |
| Fourth | Reviewing the previous session; teaching coping skills (acceptance of illness, acceptance of treatment, social support network, engaging in artistic activities, recreation, observing spiritual considerations, and problem-solving skills); relaxation practice; providing the educational booklet; question and answer to ensure that the mothers were informed about the provided contents; thanking mothers for their cooperation. |
4. Results
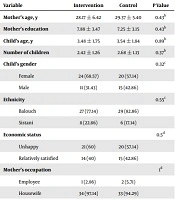
The mean age of mothers in the intervention and control groups was 28.17 ± 6.42 and 29.37 ± 5.40 years, respectively, indicating no statistically significant difference. The majority of children in the intervention (68.57%) and control (57.14%) groups were female. Moreover, no significant difference was observed in the two groups in terms of demographic characteristics (Table 2).
| Variable | Intervention | Control | P Value |
|---|---|---|---|
| Mother’s age, y | 28.17 ± 6.42 | 29.37 ± 5.40 | 0.43b |
| Mother’s education | 7.88 ± 3.47 | 7.25 ± 3.15 | 0.43b |
| Child’s age, y | 3.48 ± 1.75 | 3.54 ± 1.84 | 0.89b |
| Number of children | 2.42 ± 1.26 | 2.68 ± 1.13 | 0.37b |
| Child’s gender | 0.32c | ||
| Female | 24 (68.57) | 20 (57.14) | |
| Male | 11 (31.43) | 15 (42.86) | |
| Ethnicity | 0.55c | ||
| Balouch | 27 (77.14) | 29 (82.86) | |
| Sistani | 8 (22.86) | 6 (17.14) | |
| Economic status | 0.5d | ||
| Unhappy | 21 (60) | 20 (57.14) | |
| Relatively satisfied | 14 (40) | 15 (42.86) | |
| Mother’s occupation | 1d | ||
| Employee | 1 (2.86) | 2 (5.71) | |
| Housewife | 34 (97.14) | 33 (94.29) | |
| Father’s occupation | 1d | ||
| Employee | 3 (8.57) | 2 (5.71) | |
| Self-employed | 32 (91.43) | 33 (94.29) |
aValues are expressed as mean ± SD or No. (%).
bIndependent t-test.
cChi-square test.
dFischer’s exact test.
The mean score of different domains of adaptive behaviors in the intervention and control groups before the experiment was 58.57 ± 21.04 and 55.57 ± 18.75, respectively, indicating no significant difference (P = 0.53). However, after the experiment, this score changed to 83.68 ± 10.45 and 52.80 ± 17.46 in the intervention and control groups, respectively, illustrating the significant impact of group education on improving adaptive behaviors (P < 0.001) (Table 3).
| Group/Adaptive Behavior Pattern | Intervention | Control | P Value |
|---|---|---|---|
| Family integrity | |||
| Before experiment | 21.85 ± 7.21 | 21.85 ± 7.21 | 0.96b |
| After experiment | 28.60 ± 4.40 | 20.11 ± 6.29 | 0.001b |
| P value | P < 0.001c | P = 0.22c | |
| Social support | |||
| Before experiment | 25.08 ± 9.36 | 23.80 ± 8.37 | 0.54b |
| After experiment | 36.17 ± 5.37 | 23.22 ± 8.35 | < 0.001b |
| P value | P < 0.001c | P = 0.75c | |
| Communication and counseling | |||
| Before experiment | 11.54 ± 5.13 | 9.91 ± 4.78 | 0.17b |
| After experiment | 18.91 ± 2.17 | 9.45 ± 4.37 | < 0.001b |
| P value | P < 0.001c | P = 0.59c | |
| Total | |||
| Before experiment | 58.57 ± 21.04 | 55.57 ± 18.75 | 0.53b |
| After experiment | 83.68 ± 10.45 | 52.80 ± 17.46 | < 0.001b |
| P value | P < 0.001c | P = 0.45c |
aValues are expressed as mean ± SD.
bIndependent t-test.
cPaired t-test.
The mean score of different dimensions of caregiver burden before the experiment was 54.60 ± 12.05 in the intervention group and 59.25 ± 13.34 in the control group, showing no significant variation (P = 0.13). After the experiment, the mean caregiver burden changed to 41.28 ± 7.01 in the intervention group and 60.28 ± 13.19 in the control groups, implying a significant reduction in the caregiver burden in the intervention group (P < 0.001) (Table 4).
| Group/Caregiver Burden and Its Dimension | Intervention | Control | P Value |
|---|---|---|---|
| General burden | |||
| Before experiment | 19.88 ± 5.21 | 23.82 ± 8.87 | 0.2b |
| After experiment | 13.48 ± 2.50 | 23.91 ± 8.77 | < 0.001b |
| P value | < 0.001c | 0.96c | |
| Isolation | |||
| Before experiment | 6.80 ± 2.33 | 7.02 ± 2.03 | 0.66b |
| After experiment | 4.45 ± 1.03 | 7.62 ± 3.62 | < 0.001b |
| P value | < 0.001c | 0.38c | |
| Disappointment | |||
| Before experiment | 14.34 ± 3.19 | 14.71 ± 3.11 | 0.62b |
| After experiment | 8 ± 1.83 | 11.45 ± 3.11 | < 0.001b |
| P value | < 0.001c | 0.13c | |
| Emotional involvement | |||
| Before experiment | 5.31 ± 2.02 | 5.34 ± 1.98 | 0.95b |
| After experiment | 3.77 ± 0.91 | 5.37 ± 2.00 | < 0.001b |
| P value | < 0.001c | 0.95c | |
| Environment | |||
| Before experiment | 8.25 ± 2.2 | 8.34 ± 2.15 | 0.87b |
| After experiment | 5.22 ± 1.37 | 8.40 ± 2.18 | < 0.001b |
| P value | < 0.001c | 0.9c | |
| Total | |||
| Before experiment | 54.60 ± 12.05 | 59.25 ± 13.34 | 0.13b |
| After experiment | 41.28 ± 7.01 | 60.02 ± 13.19 | < 0.001b |
| P value | < 0.001c | 0.76c |
aValues are expressed as mean ± SD.
bIndependent t-test.
cPaired t-test.
5. Discussion
Comparing the results of the intervention and control groups demonstrated that implementing the group education program led to an improvement in all three dimensions of adaptive behaviors and a decrease in the caregiver burden in mothers of children with thalassemia major. These results are consistent with the results of other studies indicating the effectiveness of group education. For example, those studying the effect of coping skills training on the quality of life of parents of children with leukemia (34), the effect of stress coping skills training on the resilience of mothers with disabled children (35), and the effect of stress coping skills training on family functioning in families of mentally ill patients (36).
The usefulness of training coping skills through promoting positive thinking, self-assertiveness, and self-esteem/self-confidence, reconstructing memories, finding a meaning for one’s life, creating a positive family environment, and developing resilience in adjusting to existing conditions has been demonstrated (37). Using a simple educational method, Aziz et al. (38) observed that training the mothers of children with thalassemia reduces their psychosocial problems and depression. Bishop and Greeff (39) recommended group support as one of the major factors affecting adaptive behaviors in family caregivers of mentally ill patients.
The results of the present study also indicated that group training could be effective in alleviating the care burden of mothers of children with thalassemia major. Confirming our findings, Rezaei et al. (40) noted that their support group education could significantly lighten the caregiver burden in subjects similar to our study. Group training has been found to exert beneficial effects on other subjects, as well. For example, the impact of group training on the burden of family caregivers of hemodialysis patients (41), the impact of group supportive education on the burden of family caregivers of patients with heart failure (42), the effectiveness of group therapy on the mental health of mothers of children with thalassemia (6), the impact of participatory care model on the burden and resilience of family caregivers of patients with mental health disorders (43), and the effectiveness of communication skills training on the burden and quality of life of family caregivers of elderly patients with dementia can be mentioned (44). Conversely, Toseland et al. (45) rejected the efficacy of group supportive training on lowering the caregiver burden. No continuous implementation of the program to empower caregivers, as well as disregarding the livelihood needs of caregivers were mentioned as causes for the failure of the intervention. In the study by Hanzawa et al. (46), the favorable status of family coping skills, especially the ability to search for specific information about patients’ issues, was associated with reduced caregiver burden. The results of the present study exhibited that the mothers’ caregiving burden in the control group increased in all domains; in other words, routine instructions failed to mitigate caregiver burden, which is consistent with the results of other studies. Similarly, Rezaee et al. (40) reported that at the end of the study, while mothers’ caregiver burden decreased in all dimensions in the intervention group, it aggravated in all dimensions in the control group. Also, Pouraboli et al. (47) confirmed that thalassemia is socially stigmatized in Iran, and families try to conceal it; thus, they inadvertently exacerbate its adverse effects on physical and mental health. The results of this qualitative study indicated that expressing feelings and experiences by mothers is effective in reducing their psychological stress.
The effect of group training on lowering the caregiver burden of mothers of children with thalassemia major in the present study can be attributed to the application of different types of group discussion (including problem-solving and relaxation practice via relevant educational aids) and encouraging mothers and motivating them to express their caregiving experiences and different challenges encountered with. The group training program seems to be effective in both reducing the existing caregiver burden and preventing further burden (48).
On the other hand, in the present study, the intervention was carried out on a relatively large sample size compared with previous studies using a small group of subjects or conducting individual-based training methods. Also, previous studies have reported an increase in caregivers' knowledge (45, 49). In the present study, besides acquiring knowledge about their child’s illness, the subjects discussed each other’s experience of caregiving and its impact on their health. As a result, the intervention caused favorable effects on both caregiver burden and adaptive behaviors. In this respect, previous studies have proposed that holding group discussions, in addition to reducing caregiver burden, provides an opportunity for sharing experiences and cultivating empathy and psychological support among group members (40, 48). Concerning the training method for mothers, it should be stated that we attempted to empower mothers to learn and practice different coping skills, such as relaxation and stress, anger, and anxiety management. In this regard, previous studies have noted that caregivers who practice certain forms of coping strategies during the educational intervention experienced reduced caregiving burden, heightened satisfaction, and improved physical health (21, 40). Similarly, Carretero et al. (50) showed that providing caregivers with programs derived from authentic sources on mental health can raise comfort and mitigate caregiver burden, stress, and other negative consequences of caregiving. At any level, practicing adaptive mechanisms by mothers can be a source of securing maternal and child mental health (7).
Overall, according to the results of the present study, considering caregiver burden in mothers of children with thalassemia major, it appears that assessing mothers by the medical team, especially nurses, could be an appropriate method for identifying their needs. Consequently, the team can provide effective interventions to meet these requirements and alleviate the caregiver burden. These mothers should be supported by the treatment team, and their specific requirements should be addressed by a considered team member. Moreover, using support networks and associations and introducing mothers to these centers can play a substantial role in lowering the caregiver burden. As the main caregiver, families with patients with chronic diseases undergo a painful and stressful situation and urgently need help and support. However, healthcare providers usually focus on patients and treating their families as if they have a minor role in the treatment process. According to our findings, enrichment of adaptive behaviors through group training in mothers of children with thalassemia major can decrease mothers’ care burden and improve their coping skills. The intervention conducted in this study could be used in planning for the care of children with thalassemia and other chronic diseases.
5.1. Conclusions
The results of this investigation highlighted that group training focusing on mothers’ engagement can reinforce their adaptive behaviors and lower the burden they endure due to taking care of a sick person. Therefore, it may be adopted by nurses as a practical approach to boost family involvement in the health care process. Group training of parents, especially mothers, helps them identify their educational and caring needs and, by raising their awareness about the illness in question and its appropriate coping behaviors, change their situation and relieve their suffering.