1. Background
Coronary artery disease (CAD) is one of the most common cardiovascular disorders in the world. In 2012, CAD was reported as a chronic disease that could impose many restrictions on the life of an individual (1). By 2020, cardiovascular disease is estimated to be the first cause of disease-related disability worldwide. According to global statistics in 2013, the disease accounted for one-tenth of all deaths under the age of 35, one-third of all deaths between the ages of 35 and 45, and three-quarters of all deaths over the age of 45 (2). In Iran in 2015, cardiovascular disease, with an incidence of 181.4 per 100,000 people, was the cause of 46% of all deaths (more than one-third of all-cause mortality) (3).
Acute coronary syndrome (ACS) weakens one’s ability to perform daily activities. Thus, people having this condition develop depression and low quality of life. They gradually cease to continue treatment and adhere to physicians’ instructions, which may exacerbate illness, necessitate frequent hospitalization, and augment treatment costs (4). One of the most concerns in cardiovascular patients after discharge is their lack of awareness of self-care behaviors such as physical activity, nutrition, and the proper manner of taking prescribed medications. This situation can give rise to anxiety, uncertainty, and emotional issues.
In recent years, numerous plans have been advanced for patient care after discharge (5-7). E-health is a new, growing discipline where electronic devices are used to provide health care and prevention services. The World Health Organization predicts that more than 500 million patients use e-health software nowadays. The advantages of electronic devices include their portability and the fact that they can be personalized and used around the clock. These devices may also provide daily training in patient management. According to a review study exploring the impact of smart software on the self-care of patients with heart failure, these tools showed to play a positive role (8). The efficacy of these devices has also been assessed in other cardiac and non-cardiac patients, and evidence has confirmed their positive effect on self-care (9-11). In a qualitative study that deployed semi-structured interviews, it was stated that chronic patients used cell phones to monitor and manage their disease and its complications (12). The most effective measures in this regard are related to treatment and follow-up after discharge, which plays a substantial role in rehabilitation (7).
There are various methods and tools for providing written, photographic, audio, video, telephone, and internet content (13). Studies have exhibited that follow-up measures help reduce pain, anxiety, and heart failure, increase activity potential and social/family interactions, and eventually improve the quality of life of patients (14-17). Multiple studies have suggested that the self-care ability of patients with cardiovascular problems is low and readmission rates are high. Hence, it is imperative to provide them with the necessary training to improve their self-care skills (18-21). Self-care activities for patients with heart diseases include, first, committing them to take responsibility for and regulate their health-related tasks (such as how to use fluids, take medications, and live on a diet), and second, adopting appropriate measures to mitigate the symptoms. These are the most important control strategies and the key to successful treatment. Thus, the readmission rate will plummet by 50% if patients take proper self-care measures, adhere to medications and post-discharge prescriptions, and avail themselves of adequate social support. In recent years, most studies have focused on post-discharge programs aiming at allaying disease complications (5). While follow-up is effective however it is carried out, should choose an easier and less costly of follow-up methods (22).
The short message service (SMS) is one of the most convenient follow-up methods. The increasing popularity of mobile phones worldwide has turned it into a new tool in telehealth to establish communication between patients and healthcare providers (23). Another follow-up method, which has heightened the impact of hospital education, consists of providing pamphlets or educational booklets to patients (24). An advantage of this method is that it could be used in different circumstances (25). In addition to these two methods, many health centers use telephone counseling to train their clients after discharge (26). Telephone follow-up has been widely accepted as a low-cost, easy-to-use method in telehealth to exchange information, provide health education, identify complications, and manage symptoms.
However, these methods have not yet been integrated into the healthcare system of Iran (17) such that the patient has no communication with the treatment team after discharge. Therefore, it is crucial to find an effective, easy, inexpensive, and practical way to overcome this problem. On the other hand, several studies have shown the positive impact of structured telephone follow-ups in patients with heart failure (27-31), and different results have been reported concerning the effect of this method on the self-care ability of these individuals. Nevertheless, there is a scarcity of evidence comparing the effectiveness of conventional follow-up methods such as providing booklets and new approaches utilizing SMS and telephone.
2. Objectives
This study aimed to compare the effect of three follow-up methods of using the telephone, educational booklet, and SMS on the self-care ability of patients with ACS after discharge.
3. Methods
After obtaining the approval of the Ethics Committee of Zahedan University of Medical Sciences (no.: IR.ZAUMS.REC 404 1397), the authors conducted a quasi-experimental study on 120 patients with ACS who had been admitted to the CCU and PCCU of Khatam Al-Anbia Hospital and Ali Ibn Abi Talib Hospital in Zahedan between April and September 2019.
The eligibility criteria included the first-time diagnosis of ACS by a physician, age of 30 - 70 years, access to a landline or mobile phone at home, ability to use a smartphone, minimum basic literacy, and residence in Zahedan during the study period. On the other hand, the exclusion criteria included a patient’s withdrawal from the study, general deterioration of the patient for any reason, and failure to respond to at least two consecutive telephone calls.
At a confidence interval of 95% and statistical power of 95%, and according to the below formula, the sample size was estimated at 31 for each group based on the study by Farazmand et al. (17). To ensure the adequacy of sample size and consider possible attrition, the authors finally recruited 40 individuals for each of the three groups.
Z1-α/2 = 1.96; S1 = 15;
Data collection tools included a demographic questionnaire form and the self-care assessment scale designed by Kearney and Fleischer in 1979. The tool comprises 64 questions, including 21 items on having self-care ability and 43 items on practicing self-care behaviors. In this study, we used the 21 questions related to self-care behaviors. The answer to each item in this tool is scored on a five-point Likert scale (0 = never; 1 = rarely; 2 = sometimes; 3 = most often; and 4 = always). Due to their negative aspect, questions 16, 17, 19, 20, and 21 are scored in the opposite direction. The self-care score is divided into three levels of good (76% - 100%), moderate (51% - 75%), and poor (less than 50%). Thus, higher scores indicate greater self-care ability. The validity and reliability of this instrument have been established in various studies, including in France, on patients with heart disease. Nahcivan reported the efficacy of this instrument for the Turkish community (32, 33). In Iran, the content validity of the tool was ascertained by 10 faculty members of Islamic Azad University, Tehran Medical Branch, who also applied their comments and suggestions to the scale. Mohammad Hassani et al. (34) conducted a pilot study before sampling to assess the face validity of the questionnaire. They presented the scale to 30 qualified patients with CAD. After 10 days, the researchers recruited the same 30 subjects to complete the instrument. The reliability of the tool was reported with Cronbach’s alpha of 0.92 (34). In the present study, the reliability of this questionnaire was established with Cronbach’s alpha of 0.89.
After submitting their informed consent, eligible participants completed the demographic information form and the self-care questionnaire. Patients received routine instructions during the hospital stay and upon discharge. After discharge, they were divided into three intervention groups using permuted-block randomization. According to the sample size, they were assigned to 10 blocks of 12 members. In the telephone follow-up group, training was conducted at pre-arranged times twice a week (each lasting 15 to 20 minutes) for four weeks. In the SMS group, training was carried out by texting the patients daily for four weeks. In the booklet group, the instruction was provided upon discharge through a booklet containing approved guidelines. The educational content, designed based on the patients’ respective type of follow-up, was identical in all the three groups. The subjects in the telephone group were allowed to call at any time they felt necessary. However, the SMS group could raise their questions and received answers just through texting. However, this was not possible for the educational booklet group (Table 1).
| Row | Educational Content |
|---|---|
| 1 | Disease definition |
| 2 | Signs and symptoms |
| 3 | Introducing risk factors for the disease |
| 4 | Explaining medical and pharmaceutical treatments |
| 5 | Discussing individual and professional activities aiming at promoting psychosocial well-being |
| 6 | Introduction to a healthy diet |
| 7 | Treatment follow-up |
| 8 | Summarizing previous discussions |
4. Results
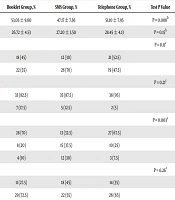
Finally, 120 people completed the study. The results showed no significant difference between the three groups in terms of gender, body mass index, role (in the family), tobacco consumption, family history of heart disease, and history of underlying diseases such as diabetes, hypertension, and renal failure. An exception in this respect was age (P = 0.008), which differed significantly between the booklet and SMS groups (P = 0.007); however, the booklet and telephone groups (P = 0.9) and the telephone and SMS groups (P = 0.1) were not significantly different in this regard. Similarly, the level of education varied significantly between the three groups (P = 0.003) (Table 2).
| Variable | Booklet Group, % | SMS Group, % | Telephone Group, % | Test P Value |
|---|---|---|---|---|
| Age | 53.05 ± 9.60 | 47.17 ± 7.56 | 51.10 ± 7.95 | P = 0.008b |
| BMI | 26.72 ± 4.53 | 27.20 ± 3.50 | 28.45 ± 4.13 | P = 0.15b |
| Gender | P = 0.11c | |||
| Female | 18 (45) | 12 (30) | 21 (52.5) | |
| Male | 22 (55) | 28 (70) | 19 (47.5) | |
| Marital status | P = 0.21c | |||
| Married | 33 (82.5) | 35 (87.5) | 38 (95) | |
| Single | 7 (17.5) | 5 (12.5) | 2 (5) | |
| Education | P = 0.003c | |||
| Under high school diploma | 28 (70) | 13 (32.5) | 27 (67.5) | |
| High school diploma | 8 (20) | 15 (37.5) | 10 (25) | |
| Associate degree or higher | 4 (10) | 12 (30) | 3 (7.5) | |
| Tobacco consumption | P = 0.26c | |||
| Yes | 11 (27.5) | 18 (45) | 14 (35) | |
| No | 29 (72.5) | 22 (55) | 26 (65) |
aValues are expressed as No. (%) or mean ± SD.
bANOVA.
cChi-square.
The results revealed no significant difference in the mean scores of self-care between the three groups before the intervention (P = 0.91), but significant changes occurred in this regard at the end of the study (P = 0.0001). The post hoc tests indicated a significant difference in the mean score of self-care between the booklet and SMS groups (P = 0.0001) and between the booklet and telephone groups (P = 0.0001). Meanwhile, the self-care scores did not vary significantly between the SMS and telephone groups after the intervention (P = 0.19). Thus, the highest self-care score after the intervention was obtained for the SMS group, and the lowest self-care score was achieved in the booklet group (Table 3).
aValues are expressed as mean ± SD.
bt-test.
cANOVA.
Once we adjusted for the effects of age and education level (which were significantly different between the three groups), the analysis of covariance showed that the mean score of self-care in the three groups increased significantly, thanks to the interventions (P = 0.0001). More specifically, pairwise comparisons demonstrated a significant difference between the booklet and SMS groups (P = 0.0001) and between the booklet and telephone groups (P = 0.0001). In contrast, the difference between the SMS and telephone groups was not significant (P = 0.11) (Table 4).
| Source of Changes | Sum of Squares | Degree of Freedom | Mean of Squares | F | Significance Level | Effect Size | Power |
|---|---|---|---|---|---|---|---|
| Pretest | 387.159 | 1 | 387.159 | 6.92 | 0.01 | 0.05 | 0.74 |
| Age | 56.95 | 1 | 56.95 | 1.01 | 0.31 | 0.009 | 0.17 |
| Education | 0.35 | 1 | 0.35 | 0.006 | 0.93 | 0.000 | 0.51 |
| Group | 5208.597 | 2 | 2604.299 | 46.58 | 0.000 | 0.45 | 1 |
| Error | 6372.810 | 114 | 55.902 | ||||
| Total | 526825.000 | 120 |
5. Discussion
The results of this study showed that after discharge, all the three follow-up methods, including texting, telephone education, and educational booklet, improved self-care ability in patients with ACS. Meanwhile, texting appeared to be more effective than the other two methods. Several studies have reported similar results. Moradi et al. (35) observed that SMS follow-up could enhance the lifestyle of patients with ACS. Studying patients with ACS, Chow et al. (36) also found that text messaging was effective in raising medication adherence and secondary prevention. Passaglia et al. (37) proposed that text messaging was effective in enhancing and controlling the risk factors in patients with ACS. Herring et al. (38) confirmed the effect of SMS-based training on the physical activity of CHD patients. Also, in keeping with the present study, Safaie et al. (39) suggested that texting could help promote adherence to treatment regimens among hypertensive patients.
Education and treatment follow-up have also been investigated in the case of other diseases, and the results are generally in good agreement with the present study. In this regard, Goodarzi et al. (40) supported the impact of SMS-based training on the knowledge and awareness of male patients with type 2 diabetes. Hovadick et al. (41) found that SMS-based follow-up could boost self-care in patients with type 2 diabetes. In a 2017 study by Abaza and Marschollek (42), educating diabetic patients through texting could ameliorate their health and self-management skills.
In the present study, the telephone follow-up, although not as effective as SMS-based follow-up, outperformed educational booklets in increasing the self-care ability of patients. In the same vein, Kamrani et al. (43) addressed the impact of training and telenursing via telephone follow-ups on diet compliance in patients with ACS, and they highlighted the positive outcome of their intervention. O’Neil et al. (44) reported the positive impact of telephone follow-ups on the quality of life of anxious patients after myocardial infarction. Shojaee et al. (5) observed that education and telephone follow-ups by nurses raised hope in patients with heart failure. Najafi et al. (6) noted that telephone follow-ups increased medication and dietary adherence in MI patients. Exploring the effect of telephone follow-ups on metabolic parameters in patients with type 2 diabetes, Lashkari et al. (45) concluded that their intervention could help better control blood glucose and maintain a more favorable BMI.
All of the above reports are consistent with the present study. On the other hand, some studies have reached opposite conclusions. For instance, Holst et al. (46) probed the effect of telephone follow-ups on the self-care status of patients with heart failure, but they found no improvement in the quality of life of the subjects, which was explained on account of the low number of phone calls or insufficient training. More recently, Jalali et al. (47) compared the effects of three follow-up methods (SMS, telephone, and routine) on the quality of life of patients with heart failure; the results showed that the quality of life score varied dramatically before and after the intervention in the SMS and regular groups, but this difference was not significant in the telephone group, which is not consistent with the present study.
The effectiveness of telephone follow-ups could be impaired by several factors, including mental status, physical condition, occupational concerns, psychological problems, and the oral manner of delivering instructions. The lowest score of self-care achieved in the case of booklet-based follow-up could be justified if one considers that Iranians are not avid readers, booklets are not available everywhere, and patients using this approach were not daily reminded to review the materials. Conversely, SMS-based follow-up, in addition to reminding subjects of their tasks daily, provided the opportunity to review the messages at appropriate time and place as needed to act according to the recommendations.
The level of education exerts a positive effect on one’s knowledge and performance. Although the subjects in the current study were randomly divided into three groups, the level of education was higher in the SMS group than in the other two groups. This difference was statistically significant, which could have affected the results. Another limitation of the present study concerns participants’ variations in terms of personal characteristics, physical status, mental state when answering questions, previous hospitalization experience, and motivation/interest.
5.1. Conclusions
Although any kind of follow-up after discharge could more or less amplify the self-care capacity of patients with ACS, the SMS-based follow-up showed to be more effective in this study. The results of this study can be used to boost the self-care ability of patients with other chronic diseases, as well. It is suggested that health centers integrate short texting service in their follow-up programs for patients with chronic diseases.