1. Background
Celiac disease (CD) is a systemic immune disorder that impairs the absorption of nutrients. It is characterized by different clinical manifestations caused by the response of specific serum autoantibodies and various injuries to the small intestinal mucosa. The global prevalence of this disease is reported to be 0.6% - 1%, which is predicted to increase in developing countries, owing to factors such as westernization of people’s diets, increased awareness about this illness, and changes in wheat production and preparation (1). In a screening study in Sweden, 30 out of 1,000 children (approximately 3%) were shown to suffer from this disease (2). Because of its chronic nature, it requires long-term treatment and may involve long-term complications. Recent studies have indicated that CD can impose a high care burden on the inflicted patient. Initially, this disease shows itself through changes to the gastrointestinal tract, followed by increased HLA-A levels as diagnosed through serological tests or biopsy examination (3). Some of the clinical features of CD include iron deficiency, anorexia, bone pain, depression, diarrhea, infertility, asthenia, nausea, vomiting, recurrent abdominal pain, recurrent aphthous stomatitis, recurrent miscarriages, short stature, weight loss, and unexplained elevated liver enzymes (4). Because CD occurs in childhood, it can lead to mental, psychological, and personality problems alongside physical ones, hence negatively affecting all aspects of patients’ life and impairing their overall quality of life (5-7). The concept of quality of life dates back to Aristotle (385 BC), and it has been extensively studied in recent years as a result of the rise in chronic diseases in the last century and their adverse effects on this health variable (8). According to the World Health Organization, people’s quality of life is their perception of their place in life in terms of their culture, the value system they live in, as well as their goals, standards, expectations, and priorities; besides, it is completely personal and is based on people’s understanding of different aspects of life (1, 9, 10).
Since currently, the only known treatment for CD is dietary gluten restriction, patients’ normal social interactions are limited. Moreover, a gluten-free diet or restriction on gluten intake can impose adverse effects on the quality of life (11). Numerous studies have reported different levels of quality of life for patients with this condition (12-14). In this regard, Shull et al. found that the quality of life in children newly diagnosed with CD is lower than that of healthy children (15). Similarly, Deepak et al. suggested that people with CD experience a lower quality of life than do individuals who are not affected by this condition (16). As chronic illnesses affect patients’ quality of life and their personal, social, and emotional behaviors, identifying the factors that help improve quality of life is highly desirable (12). People’s quality of life and its related factors could be of interest in evaluating chronic diseases, implementing effective interventions, assessing the effectiveness and relative advantages of different therapies, promoting physician-patient relationship, evaluating health services, research, and policy-making, and finally studying economy and resource distribution (17-19). Various factors can negatively affect both CD and the quality of life of those involved. Because of its chronic nature, researchers regard dietary restriction, nutrient intake restriction, and medical follow-ups as the main determinants of quality of life in these patients (13). With this respect, Mager et al. reported that deficiencies in nutrients, including vitamin D, could jeopardize skeletal and hematopoietic status in people with CD (20). Special attention must be paid to the intake of these micronutrients, owing to the damage to the small intestine and the impaired absorption of these substances in patients with CD.
2. Objectives
This study aimed to investigate the quality of life and its key performance indicators (KPIs) in patients with CD admitted, in 2018, to the Celiac Association of Bouali Hospital in Zahedan.
3. Methods
After receiving the approval of the Ethics Committee of Zahedan University of Medical Sciences (IR.ZAUMS.REC.1397.195), we conducted this descriptive-analytical study on 60 patients with CD who were admitted to the Celia Association of Bouai Hospital in Zahedan in 2018. The inclusion criteria were age over 18 years, celiac diagnosis by a gastroenterologist, lack of communication problems (vision and hearing), and willingness to participate in the study. Alternatively, those who were reluctant to cooperate were excluded from the study.
Data collection tools consisted of a demographic form (age, gender, marital status, duration of illness, education, ethnicity, economic status, occupation, breastfeeding history, family history of CD, and vitamin D and iron supplementation), and the Quality of Life Questionnaire for patients with CD, designed by Winfried Hauser et al. (2007). The latter instrument consists of 28 items and 4 domains. These domains include emotions (7 questions), gastrointestinal symptoms (7 questions), concerns (7 questions), and social skills (7 questions). It is scored using a 5-point Likert scale (1 = never, 2 = sometimes, 3 = usually, 4 = often, 5 = always). Each domain is scored between 7 and 35, and the total score ranges from 28 to 140, with lower scores representing higher levels of quality of life. Pouchot et al. examined the validity of this questionnaire and confirmed its reliability at the Cronbach’s alpha of 0.79 for the four subscales and 0.94 for the entire questionnaire (21, 22). Similarly, in Iran, Barzegar et al. translated and validated this instrument and reported a Cronbach’s alpha of 0.73 - 0.92 for its subscales and 0.9 for the entire questionnaire (23). We sampled the eligible patients who referred to this center. Next, the aims of the study were explained to the participants and their written informed consent was acquired. Finally, data were analyzed by SPSS-21 using descriptive statistics at the significance level of less than 0.05.
4. Results
Overall, 60 participants completed the study. Specifically, 66.7% of the subjects were female, 76.7% were married, and 85.3% stated a family history of CD (Table 1).
| Variable | Mean ± SD or No. (%) |
|---|---|
| Age | 19.03 ± 8.6 |
| Mean duration of disease | 58.5 ± 4.6 |
| Ethnicity | 16 (26.7) |
| Balouch | |
| Sistani | 44 (73.3) |
| Financial status | 23 (55) |
| Acceptable | |
| Unacceptable | 27 (45) |
| Occupational status | 13 (21.7) |
| Housewife | |
| Employee | 8 (13.3) |
| Self-employed | 10 (16.7) |
| Unemployed | 29 (48.3) |
| Breastfeeding history | 53 (88.3) |
| Yes | |
| No | 7 (11.7) |
| Supplementation history | 39 (65) |
| Yes | |
| No | 21 (35) |
Personal Characteristics and KPIs of Study Subjects with Celiac Disease
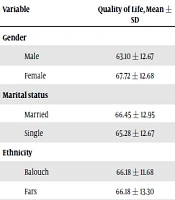
The results indicated that the lowest and highest scores of the quality of life were associated with concerns (51.81 ± 3.85) and social skills (8.31 ± 4.61), respectively (Table 2). There was no statistically significant difference between the quality of life scores and the demographic characteristics of the participants (Table 3), but a significant relationship was found between vitamin D supplementation and quality of life (Table 4).
| Quality of life dimensions | Mean ± SD | Minimum | Maximum |
|---|---|---|---|
| Emotions | 61.71 ± 3.57 | 10 | 24 |
| Social skills | 8.31 ± 4.61 | 6 | 26 |
| Concerns | 51.81 ± 3.85 | 10 | 27 |
| Gastrointestinal disorders | 71 ± 4.24 | 9 | 24 |
| Overall quality of life | 66.18 ± 18.33 | 44 | 92 |
Various Dimensions of Quality of Life of the Study Subjects with Celiac Disease
| Variable | Quality of Life, Mean ± SD | P Value | F |
|---|---|---|---|
| Gender | 0.19 | 0.2 | |
| Male | 63.10 ± 12.67 | ||
| Female | 67.72 ± 12.68 | ||
| Marital status | 0.7 | 0.53 | |
| Married | 66.45 ± 12.95 | ||
| Single | 65.28 ± 12.67 | ||
| Ethnicity | 0.9 | 1.4 | |
| Balouch | 66.18 ± 11.68 | ||
| Fars | 66.18 ± 13.30 | ||
| Income | 0.9 | 0.59 | |
| Acceptable | 66.33 ± 13.11 | ||
| Unacceptable | 66.00 ± 12.63 | ||
| Family history of celiac disease | 0.2 | 0.01 | |
| Yes | 67.94 ± 12.34 | ||
| No | 62.72 ± 13.25 | ||
| Supplementation history | 0.1 | 1.06 | |
| Yes | 64.23 ± 11.61 | ||
| No | 69.80 ± 14.33 | ||
| Breastfeeding history | 0.19 | 0.6 | |
| Yes | 65.46 ± 12.73 | ||
| No | 72.66 ± 12.54 |
Relationship Between the Mean Scores of the Quality of Life and Demographic Characteristics of the Subjects with Celiac Disease
| Dependent Variable | Variable | Non-Standardized Regression Coefficient | Standard Error | Standardized Regression Coefficient | Correlation | T | P Value |
|---|---|---|---|---|---|---|---|
| Quality of life | Vitamin D | 0.25 | 0.12 | 0.26 | 0.26 | 2.11 | 0.03 |
| Iron | 0.07 | 0.08 | 0.11 | 0.11 | 0.85 | 0.39 | |
| BMI | 0.02 | 5 | -0.07 | 0.11 | -0.05 | 0.95 |
Relationship Between Quality of Life and KPIs in the Subjects with Celiac Disease
5. Discussion
The results of the present study indicate that the quality of life of children with CD was lower than that reported by Deepak et al., who stated that quality of life is affected by the severity of complications and symptoms (16). We also found that quality of life was lower in men, single people, as well as people with a history of medication and no history of supplementation, but this difference was not statistically significant, which could be due to the low sample size [in our study]. In a study by Pratesi et al. in 2018, a significant relationship was observed between gender and quality of life in people with CD; however, the mean quality of life reported in this study is higher than that in our study (14). In the same vein, Hallert et al. noticed that men with CD enjoyed a better quality of life than women (24), which contradicts our results inasmuch as we observed a greater quality of life among women than men. Given that quality of life could be influenced by one’s culture and lifestyle, we may point to variations in the culture of participants in the two studies as one way of explaining this incompatibility. In this regard, Nachman et al. proposed that patients with atypical CD who showed no clear symptoms, experienced a better quality of life than people with intensified symptoms of CD, which was explained on account of the restricted gluten intake in the latter group (12). Similarly, Samasca et al. examined gluten-free diet and quality of life in patients with CD and found that quality of life of these people is likely to improve [only] if the disease is diagnosed early because the advanced stages of this illness seriously diminish patients’ quality of life (25). The findings reported by Tontini et al. (26) support those of Samasca et al. (25).
Since various factors such as nutrient intake could have a burden on the quality of life, it is essential to identify them and step up efforts to promote the quality of life of patients with CD. The results of our study suggest a significant relationship between vitamin D supplementation and the quality of life of people with CD. In this regard, numerous studies on patients with CD (2, 27-30) have displayed that these individuals, compared to other people with a regular diet, have low levels of micronutrients such as vitamin D, folate, and iron, and the increase in the intake of these micronutrients can help reduce the side effects of these substances and enhance patients’ quality of life. The reason for the disparity in the results of our study and those of other reports may be owing to the fact that our samples had restricted gluten intake and received dietary supplements, including vitamin D. In another study by Mager et al., it was also reported that vitamin D and vitamin K could have a considerable positive impact on bone mass in patients with CD (20). Furthermore, insofar as physical health can positively influence the quality of life, it is possible to help these individuals raise their awareness about micronutrient intakes in order to mitigate their complications.
5.1. Conclusion
The results of this study established that, among various key performance indicators, there is a significant relationship between vitamin D supplementation and quality of life of celiac patients. Considering dietary restrictions and digestive system disorders in these individuals and also because the quality of life is a multidimensional indicator that may be affected by physical health, it seems that increasing the awareness of patients with CD about micronutrient intakes can be tremendously helpful in improving their physical health and, consequently, quality of life.