1. Background
As the most prevalent and debilitating neurological lesion in adults, stroke is the leading cause of death worldwide. In Iran, stroke is the third leading cause of death after heart disease and cancer (1, 2). According to the World Health Organization, the incidence rate for stroke ranged between 2.7 to 7.4 per 1,000 people; in European countries, its annual prevalence is nearly one million per year (3, 4). In Iran, approximately 139 to 149 per 100,000 per year suffer a stroke, which is significantly higher than the rate reported for developed countries. Moreover, it is expected to increase as the proportion of the elderly population rises (5).
The survival rate of hemorrhagic stroke and ischemic stroke is about 30% - 40% and 70%, respectively, and are associated with some degree of disability (6). In the acute stage of the disease, depending on the location and extent of the lesion, these patients suffer from visual, motor, sensory, verbal, and cognitive defects (2, 3). Of the stroke survivors, 75% experience residual disability, who 15% - 30% of them report a high degree of disability (4). Tink and Tink and Kessler (7) reported that more than 50% of stroke patients suffer from long-term disabilities and inability to perform daily life activities, hence a reduction in their quality of life (Qol).
In those stroke patients who suffer from severe disabilities and need continuous care for up to three months after stroke, the risk of mortality is approximately seven times higher than other patients (4). Although the acute phase of the disease lasts only for a few days, the recovery process is slow and gradual (8).
Most often, patients that passed the acute phase experience severe physical and mental disability; at best, for up to six months, they require continuous care in daily activities and self-care programs (9, 10). By damaging the sensory, motor, perceptual, visual, and cognitive systems, stroke impairs patients’ ability to perform daily life activities (11). Due to sored hospital expenditures, the hospital stay of stroke patients has now been reduced. Besides, now families are responsible for post-discharge care, that often are not equipped with sufficient knowledge and skills (12).
Long-term complications of stroke include: rebleeding or hematoma, cerebrovascular spasm and subsequent cerebral ischemia, seizure, acute hydrocephalus, severe headache, decreased consciousness, aphasia, hemiparesis, dehydration, increased ICP, hypertension, loss of swallowing reflex, urinary or fecal incontinence, impaired blinking and dry eyes, immobility, impaired skin integrity and pressure ulcer, muscle wasting, insomnia, and stress (13, 14).
Therefore, as the main cause of disability, stroke negatively affects the daily activities and reduces the QoL of patients (15, 16). Salarimehr et al. (6) and Laurent et al. (14) showed that stroke is associated with a significant reduction of QoL. Based on the evidence, despite advances in therapeutic modalities, most of discharged stroke patients require intensive care in their daily activities such as dressing, eating, and bathing (17, 18). According to the estimates, 62% of stroke surviving patients will depend on others support. The main therapeutic options of stroke include rehabilitation, nutrition, and medication. Based on the aforementioned, stroke patient’s treatment adherence is an important challenge that can affect the process of daily activities, continuation of care, and follow-up consultations. Which, in turn, influences their QoL. Studies have suggested families’ low level of awareness about adherence to treatment is partly associated with higher rates of long-term complications and readmission (19, 20).
Various programs are available to prevent the potential complications of the disease and to raise patients’ QoL, such as proper methods of medication, family therapy, and rehabilitation measures (18). The latter is a set of processes in which people with a disability are helped to regain their ability after an event, illness, or injury that has resulted in their functional limitation (21). In this regard, an important therapeutic goal is to promote patient independence, avoid readmission, and reduce staggering costs (22). Since stroke causes severe complications and the long hospital staying of patients, it causes various problems for both patients and their families. Some of these problems are due to sudden exposure to the disease, adopting a new role as a caregiver, lack of sufficient information about the disease and how to care for the patient, lack of pre-discharge rehabilitation programs, and lack of social support. Home-based rehabilitation (HBR) is an effective method that aims to increase the engagement of patients and families in identifying the needs and to provide the necessary education (23). HBR intends to maintain and restore patients’ health and independence as well as reducing the disability caused by chronic illnesses (8, 24). Such services are very useful in meeting the health demands of people requiring rehabilitation and are considered extremely valuable thanks to their low cost, feasibility, providing the client’s comfort, reducing frequent hospitalizations, and establishing a link between the hospital and the community.
Benefits of HBR services include the client’s interaction with the family, direct and immediate education of the client and family, further promotion of the client’s independent performance, and increased level of authority of rehabilitation nurses. Previous studies found that continuous and long-term care for people with chronic diseases, including stroke, has a significant effect on improving both their adherence to the treatment and their QoL. Nevertheless, most of these studies were focused on institution-based rehabilitation services and rarely addressed the effectiveness of community-based programs, especially home-based models (8, 18).
Therefore, using home-based rehabilitation models, as an effective solution, would help provide services related to chronic diseases (24, 25). Numerous studies are conducted in this field. Jokar et al. (26) proposed that the implementation of home-based pulmonary rehabilitation programs is an effective step to enhance daily life activities, maximize patients’ independence, and mitigate complications for patients with obstructive pulmonary disease. Thanks to their functional role, including training, nurses are the best members of the health team to provide patients with a suitable plan to adhere to the treatment. To continue care, health personnel should make regular appointments or telephone calls with patients and their families, monitor the patients’ adherence to treatment, identify barriers to non-compliance and promote patients’ QoL, and assist patients in overcoming and managing the obstacles (8, 18).
2. Objectives
Considering the importance of continuity of care, long duration of stroke, the possibility of development and/or aggravation of complications, and the need to adhere to treatment, the current study aimed to investigate the effect of HBR on treatment adherence and QoL of stroke patients.
3. Methods
In this study, 60 stroke patients admitted to the Internal Medicine and Neurology Department of hospitals affiliated to the ZUMS, southeast of Iran, during the 2019 are studies. Subjects were selected by convenience sampling and then were randomly assigned to intervention and control groups. The inclusion criteria included having ischemic stroke for the first time; acute phase passage (48 to 72 hours); not receiving alteplase; having a rate of 3 or 4 as measured 48 hours after stroke based on the Rankine scale (an instrument intended to assess the degree of functional disability following the stroke, in which the score of disability ranges from 0 to 5) (8); being literate (patient or the main caregiver); no underlying diseases such as spinal cord injuries, disabilities, and Alzheimer’s disease; no cognitive impairment (a score of 8 or higher based on the Abbreviated Mental test) (27); requiring post-discharge care; and the possibility of making telephone calls to the primary caregiver or patient. Refusing to continue the study, developing critical symptoms, readmission, receiving services other than those provided by HBR programs, and the death of the patient during the study were considered as the exclusion criteria. The current study is confirmed by the Ethics Committee (code: IR.ZAUMS.REC.1398.238) of the Zahedan University of Medical Sciences (ZUMS).
The sample size was calculated as 25.91, based on the mean and standard deviation of the QoL score reported by Azimi et al. (18), considering a 95% confidence interval and 95% power. The sample size was calculated using the following formula:
To account for attrition or loss to follow up (assuming a 20% attrition), the sample size was increased to 30 subjects for each group.
Data were collected using a demographic form, the Adherence to Treatment Regimen questionnaire, and Stroke Specific Quality of Life scale. The demographic form included age, gender, marital status, education, occupation, main caregiver, disease history, smoking, and complications of the stroke.
The adherence to treatment regimen is a researcher-made questionnaire introduced by Dehghan Nayeri et al. (8), which has 45 items in three sections. The first part contains 28 items about following the rehabilitation regimen. This part measures how the family cares for the patient concerning the following items: Improving the patient’s motor status; preventing deformities and limb pain; correcting the thinking process; achieving a proper method of communication; overcoming sensory, perceptual, and cognitive limitations; skin health; preventing respiratory infections, and bladder and bowel management. The second part includes 11 items on adherence to regimens and assesses how the family cares for the patient regarding following up the prescribed regimen in addition to the patient’s nutritional care. The third part includes 6 items intended to assess how the family cares for the patient in terms of drug use program, attention to side effects, and the importance of regular consumption of drugs. Each item is scored using a three-point Likert scale: Always = 3, sometimes = 2, and never =1. Two items of the questionnaire have a negative connotation, and their scores should be calculated inversely. The total score of adherence to treatment regimen ranges from 45 to 135; the higher the score, the greater the adherence to the treatment regimen is. The face validity and content validity of this instrument are confirmed, and its content validity index (CVI) was > 0.8 in all items. The reliability of this questionnaire is evaluated using Cronbach’s alpha (0.86) (8). In the present study, Cronbach’s alpha was equal to 0.84.
The stroke-specific quality of life (SS-QOL) scale is designed by Williams et al. (28), consisting of 49 items. The questions are rated based on a 5-point Likert scale. The total score ranges from 49 to 245, and higher scores indicate better QoL. The 12 domains of SS-QOL include personality (3 items), self-care (5 items), social roles (5 items), mood (5 items), upper extremity function (5 items), vision (3 items), work and productivity (3 items), mobility (6 items), energy (3 items), language (5 items), family roles (3 items), and thinking (3 items). The answers range “strongly disagree” to “strongly agree” (in the domains of energy, family roles, mood, personality, and social roles), “I had no problem” to “I could not at all” (in the domains of mobility, thinking, upper extremity function, vision, language, and work and productivity), and “I was independent” to “I am completely dependent” (in the domain of self-care). Higher scores indicate better QoL. Williams et al. (28) reported that the reliability of various domains of SS-QOL is above 0.75. In Iran, Azimi et al. (18) confirmed the internal consistency of this questionnaire, based on Cronbach’s alpha (0.95), and its test-retest reliability (0.68). In the present study, the reliability of this tool was established based on Cronbach’s alpha (0.81).
Before beginning the study, it was approved by the ethics committee of the ZUMS. Then, researchers referred to the internal medicine and neurology department of hospitals affiliated to ZUMS. Eligible patients were selected using convenience sampling. Then, they were randomly allocated to either the intervention or control group. Color card methodology was used for random allocation of participants, such that the white and red cards determined that the patient in question was to be assigned to the intervention or control group, respectively. The objectives of the study were explained to the participants, and, if they were agreeing, informed written consent was taken from them. Afterward, first, the disability of participating patients was evaluated using the Rankine scale. Also, to assess cognitive impairment, Abbreviated Mental test (AMT) was used. Subsequently, the demographic form (including items on age, gender, marital status, level of education, occupation, main caregiver, medical history, smoking, and complications following stroke) was given to either the patient or caregiver in both groups. Since subjects were newly diagnosed with stroke, it was not possible to assess their QoL and adherence to treatment before the intervention. Before providing rehabilitation training to the patients in the intervention group, information on how to follow the experiment were provided to them. Then, the intervention was provided after the acute phase passage (48 to 72 hours) in three 45-minute sessions to the patient and the main caregiver in the patient’s room. The main focus of the intervention was knowledge about the disease and HBR. The content was prepared using scientific texts, while the process was supervised by experienced experts (2, 13). A booklet was provided to the participants at the end of the intervention (Table 1). To avoid ambiguity, caregivers were asked to apply the content in the presence of the trainer (who was a nurse) and to repeat the training during the hospital stay. The patients were also encouraged to actively participate in the exercises. After discharge, the HBR was monitoring twice a week for two weeks (four times) using phone calls or in-person conversations. Besides, in the case of any problem, caregivers could call the research team whenever needed.
| Session | Topic |
|---|---|
| First | Stroke and its causes, post-stroke complications, rehabilitation regimen (physical activity, change of position, range of motion exercises, personal hygiene, bed sores) |
| Second | Diet education (proper nutrition, nutritional care, oral hygiene) |
| Third | Medication regimen education (type of medication, how and when to take drugs, side effects) |
In the control group, one month after the start of the intervention, the caregivers were contacted to ensure that patients did not receive any training other than the usual hospital instructions. The questionnaires were completed in two stages, one and three months after the intervention, by visiting patients in their homes. (The Adherence to Treatment Regimen and the Stroke-Specific Quality of Life scale should be completed by the caregiver and the patient, respectively).
To observe ethical considerations, the educational booklet was provided to the control group at the end of the study. Data were analyzed in SPSS-22 using repeated measures ANOVA, independent t-test, and chi-squared test at the significance level of P < 0.05.
4. Results
Shapiro Wilk test showed that the data are distributed normally, so parametric tests were used. The mean age of patients in the intervention and control groups was 60.70 ± 7.33 and 60.20 ± 4.35, respectively. In terms of ethnicity, 40% of the intervention group and 60% of the control group were Fars. For those in the intervention group, caregivers were mostly (70%) children of the patient, while in the control group, mostly spouse was the caregiver (60%) (P = 0.02). For other demographic characteristics, the two groups were similar, and there was no significant difference, except for the level of education (P = 0.03), occupation (P = 0.04), and underlying disease (P = 0.02) (Table 2).
| Variable | Intervention Group | Control Group | Result |
|---|---|---|---|
| Age | 60.70 ± 7.33 | 60.20 ± 4.35 | 0.74b |
| Years of education | 2.50 ± 3.19 | 5.10 ± 5.56 | 0.03b |
| Gender | 1c | ||
| Female | 15 (50) | 15 (50) | |
| Male | 15 (50) | 15 (50) | |
| Ethnicity | 0.12c | ||
| Baloch | 18 (60) | 12 (40) | |
| Fars | 12 (40) | 18 (60) | |
| Occupation | 0.04c | ||
| Employed | 12 (40) | 9 (30) | |
| Unemployed | 18 (60) | 21 (70) | |
| Main caregiver | 0.02c | ||
| Spouse | 9 (30) | 18 (60) | |
| Child | 21 (70) | 12 (40) | |
| Underlying disease | 0.02c | ||
| Yes | 21 (70) | 27 (90) | |
| No | 9 (30) | 3 (10) | |
| Smoking | 0.11c | ||
| Yes | 9 (30) | 15 (50) | |
| No | 21 (70) | 15 (50) | |
| Numbers of complications | 0.07c | ||
| Two | 9 (30) | 12 (40) | |
| More than two | 21 (70) | 18 (60) |
aValues are expressed as mean ± SD or No. (%).
bIndependent t-test.
cChi-squared test.
Comparing the mean scores of various domains of adherence to treatment regimen one and three months after providing the intervention revealed a significant difference between the two groups (P = 0.001); for the intervention group, the mean adherence score had a rising trend in the second stage in all three areas and was higher than the control group (Table 3). The results of repeated measures ANOVA regarding adherence to treatment regimen and its dimensions reinforced that the score changes were not the same in the two groups and changes were higher in the intervention group than the control. The mean score of adherence and its dimensions are affected by intervention and time variables. Besides, there was a significant difference in the measured time intervals (P < 0.001).
| Dimension of Treatment Adherence | Group | |||
|---|---|---|---|---|
| Intervention Group | Control Group | Pb | Pc | |
| Rehabilitation | < 0.001 | |||
| 1 month after intervention | 72 ± 3.24 | 52.1 ± 4.15 | < 0.001 | |
| 3 months after the intervention | 77.1 ± 4.75 | 53.26 ± 5.94 | < 0.001 | |
| Diet | < 0.001 | |||
| 1 month after intervention | 29.8 ± 1.49 | 24 ± 2.4 | < 0.001 | |
| 3 months after the intervention | 31.26 ± 1.91 | 24.5 ± 3.07 | < 0.001 | |
| Medication | < 0.001 | |||
| 1 month after intervention | 16.66 ± 1.32 | 15.76 ± 0.56 | 0.001 | |
| 3 months after intervention | 17.76 ± 0.5 | 15.20 ± 1.37 | < 0.001 | |
| Total score | < 0.001 | |||
| 1 month after intervention | 118.46 ± 4.65 | 91.86 ± 5.35 | < 0.001 | |
| 3 months after the intervention | 126.13 ± 25.17 | 92.96 ± 7.57 | < 0.001 | |
aValues are expressed as mean ± SD.
bIndependent t-test.
cRepeated measures ANOVA.
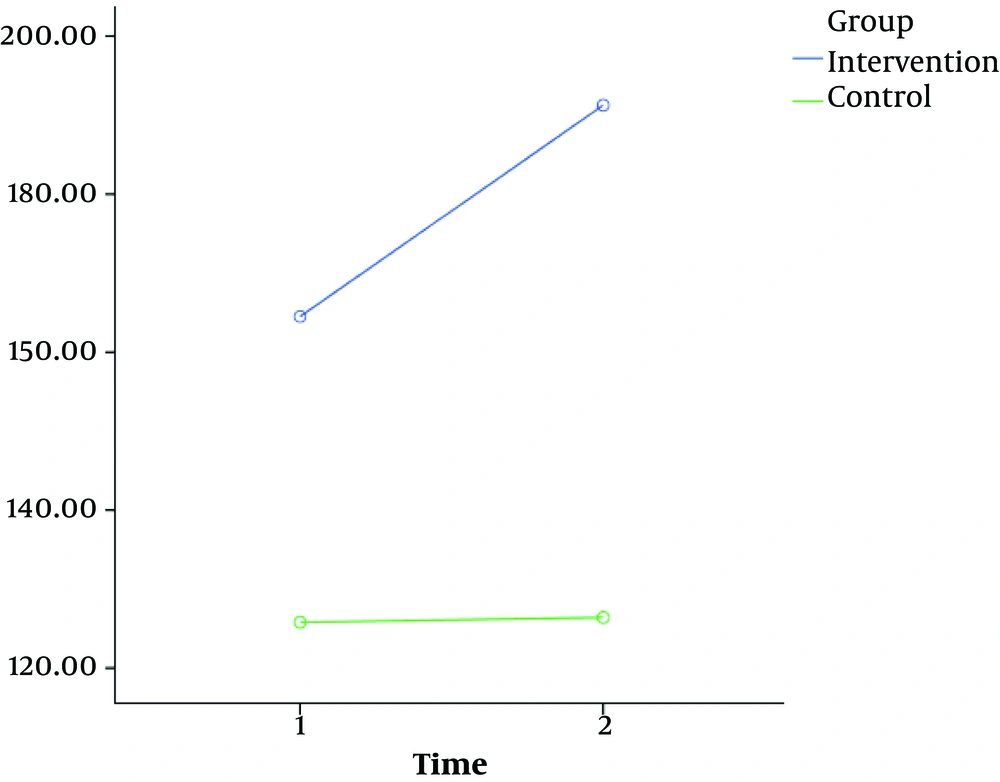
Comparing the mean total score of QoL in stroke patients demonstrated a statistically significant difference between the two groups in the two evaluation stages (P < 0.001), such that the mean score for the intervention group was higher than the control group in both stages. The results of repeated measures ANOVA illustrated QoL scores didn’t change similarly in both groups (P < 0.001) (Figure 1 and Table 4).
aValues are expressed as mean ± SD or No. (%).
bRepeated measures ANOVA.
cIndependent t-test.
Comparing the scores of the two groups showed that HBR could effectively increase both adherence to the treatment regimen and QoL of stroke patients.
Regarding the rehabilitation regimen (the first domain of adherence to treatment), the intervention group showed more adherence in the two stages than the control group, which is consistent with the findings of previous studies.
5. Discussion
Research supports the effect of family-centered empowerment programs on adherence to the treatment regimen in stroke patients (8) and the effect of the family-centered empowerment model on the level of family cooperation in following the treatment regimen in patients undergoing coronary artery bypass graft surgery (23).
Shyu et al. (10) reported that the quality of patient care and adherence to rehabilitation programs was better in the intervention group than the control group. The authors attributed the success of such programs to the implementation of care and education programs according to specific care needs and complications of each patient and condition of the family (10). Similarly, we performed the rehabilitation program for each patient and main caregiver separately and based on the patient's needs, which may be one of the reasons for the success of this program in raising patients’ adherence to the rehabilitation regimen.
Based on the findings, the HBR receiving was more successful in diet adherence (the second domain of adherence to treatment regimen) than the control group that received routine care, which is consistent with findings of previous studies, including those about the effect of family-centered empowerment programs on adherence to the treatment regimen in stroke patients (8) and the effect of the family-centered empowerment model on the level of family cooperation in following the treatment regimen in patients undergoing coronary artery bypass graft surgery (23). Sanaie et al. (23) found a statistically significant difference concerning the level of diet adherence between the two groups. This variation is attributed to factors such as holding training sessions, providing an educational booklet, and raising sensitivity after continuous follow-up programs (e.g., by phone calls (23)), which are also the case in the present study.
Chien et al. (11) found that knowledge and awareness about the low-fat diet were significantly higher among those who received nutrition training (both the patient and family) than the control group. However, the authors reported no statistically significant difference between the actual adherence of the two groups to the diet (11). This ineffectiveness could be explained by the fact that patients received just one educational session, and no other post-discharge instruction is provided.
The findings of the present study revealed that patients in the intervention group better adhered to the medication (the third dimension of adherence to treatment regimen) than the control group. This finding is in good agreement with the study by Kamal et al. (29), who suggested that reminding the dose of the drug by SMS could be effective in the recovery process of stroke patients and their adherence to medication.
Although the mean score of adherence to the drug regimen between the two groups was statistically significant in the present study, in the intervention group after three months, it increased to a lower extent than the rate of adherence to diet and rehabilitation. Conversely, Dehghan Nayeri et al. (8) reported a significant increase in adherence to medication, unlike adherence to diet and rehabilitation. Johnson et al. (25) also demonstrated a similar rate of adherence to medication (87% - 100%) in the two periods (the first six weeks and six months) after stroke.
Most patients and their caregivers consider the medication regimen as the most important intervention to cure the disease and to prevent its non-recurrence; hence, they may substitute other therapeutic interventions, as rehabilitation and diet, with medication and assume that sole medication can cure the disease. Besides, they consider medication to be much simpler and less costly than other therapeutic measures like rehabilitation.
Gance-Cleveland (12) argued that family-centered educational programs on medication regimen can effectively promote patients’ adherence to treatment as well as their interactions with their family. Employing simple tools and methods in providing education assists both patients and families to better understand the medication regimen. Besides, providing practical and necessary instructions plays an important role in improving adherence to this regimen. Accordingly, we carried out the intervention with an emphasis on presenting essential and understandable points for patients and caregivers.
Another important finding of the present study was improved QoL of stroke patients three months after providing the HBR, which is consistent with the studies by Azimi et al. (18) and Jokar et al. (26). Providing several face-to-face training sessions for patients and caregivers, as well as following them after discharge from the hospital and using educational booklet, are among the most important causes of HBR effectiveness in the present study.
Oh (15) reported that rehabilitation measures could significantly boost exercise tolerance of patients with chronic lung disease. Hui-Chan et al. (16) reported that the HBR program improved lower extremity function in patients who had a stroke a year earlier. Through rehabilitation, the patient learns to modify his/her lifestyle to some extent, which in turn improves his/her daily activities and QoL.
In the present study, the control group received the usual hospital care, and their rate of adherence to the treatment regimen was lower than the intervention group. In the latter, by raising patient’s and families’ awareness, HBR could improve adherence to the treatment regimen. Therefore, based on the findings, the HBR program not only increased adherence to treatment regimen in three areas of rehabilitation, diet, and medication but also improved the QoL of patients with stroke.
5.1. Conclusions
This study showed that HBR not also can increase adherence of stroke patients to the treatment regimen in three areas of rehabilitation, diet, and medication, but also improves their QoL. Therefore, the authors strongly recommend the administration of this approach by nursing staff to better involve patients with chronic diseases and their families in the continuum of care.