1. Background
Childbirth is one of the most amazing and special experiences in a women’s life and a transition to the maternal stage (1, 2). In the present era, for different reasons, such as the marriage age rising, the cesarean section has become one of the most common surgeries (2), and it incredibly is growing all over the world (3). Approximately 1.8 million cesarean sections occur annually worldwide (4). In our city, cesarean sections have been reported as 40% in Fasa in 2011 (5). Due to complications such as hemorrhage, surgical site infection, pulmonary embolism, aspiration, atelectasis, and thrombophlebitis, which are major causes of maternal death, cesarean section is riskier than vaginal delivery (6). Delay in scar healing is of other complications (7).
Although sterile tips or preoperative skin preparation and the use of appropriate surgical techniques play roles in reducing site infection, surgical site infection is one of the most common nosocomial infections associated with hematoma, serous, and scar opening, which is also one of the most common causes of post-cesarean deaths (8, 9), leading to mother’s hospitalization and frequent referral to doctors. It also imposes enormous economic and emotional burdens on the family and society (10) and causes emotional separation between mother and baby (9). It has been reported that the post-cesarean section infection rate is 3 - 18%. Therefore, scar (surgery site) healing is the main goal of post-surgery care (11). Given the increasing cost of health care in surgical scar complications, the use of empowerment and self-care methods for scar healing is important and significant (12).
The self-care strategy is one of the main goals of the health care system to improve performance and increase the quality of life, but increasing self-care knowledge that improves the quality of life has to be provided through training. Patient training is one of the main parts of treatment that helps the patient participate in self-care (13). Studies have shown that patient training is very effective in reducing risky behaviors and increasing healthy behaviors (14), which is done by the care team, especially the nurses (15). In recent years, the nurses’ role as the main members of the health care system has experienced historic changes and goes toward empowering patients to self-care and become healthy.
Patient awareness and his/her participation in self-care reduce the hospitalization duration and referral to the hospital (16). The main goal of self-care training for patients who undergo an operation is to reduce surgery-related complications (17). In a study done by Chan et al. (2014) concerning the effect of training using the telephone on clean scar healing in patients, the results showed no significant difference between patients whose scar was dressed by nurses and patients who changed their wound dressing at home based on telephone training. Chan also stated that patients, like professional personnel, can control acute and anti-infectious scars at home using sterile wound dressing (18).
2. Objectives
Given that the effect of a self-care training program on cesarean section site healing has not been investigated so far, and considering the results of studies on the prevalence of complications associated with surgical site incision in cesarean section patients and their lack of knowledge of self-care related to surgical site incision healing, this study was done to determine the effect of a self-care training program on cesarean section site healing in women.
3. Methods
A quasi-experimental clinical trial was performed in 72 women undergoing cesarean section in 2017 at one of the medical centers of Sarpol-e Zahab. The statistical population of the study included all nulliparous and multiparous women with a history of the last cesarean section in the last two years and those who were referred to the hospital in 37 weeks of pregnancy, meeting the inclusion criteria. Random allocation in clinical trial studies refers to the process of dividing participants into different groups at random. Randomization gives each participant an equal chance of being in each of the groups. Successful randomization requires that researchers and study participants be able to predict the type. Sampling was based on inclusion criteria: 18 to 35 years of age, pregnancy age later than 37 weeks, ability to read and write, ability to see and hear and understand the Persian language, BMI < 30, not taking psychiatric drugs and vitamins, and not having psychological illness and chronic diseases according to medical records. The exclusion criteria were unwillingness to continue the study and refusal to attend the training session.
Based on the inclusion criteria, the subjects were randomly assigned to control or intervention groups. Written informed consent was obtained from all participants. The sample size was determined at a confidence level of 95% and a test power of 90%, and given that the effect size of the self-care training program on surgical site healing compared to the control group had to be at least d-1 (degrees of freedom) to consider the effect of the educational program as statistically significant, the calculated sample size in each group was 35 subjects. In addition, due to the possibility of sample drop-out, a 10% was added to the above sample size. Finally, the sample size in each group was determined to be 38 people (4).
The instruments of this research included a questionnaire on demographic characteristics, which contained items on personal characteristics (age, education level, economic status, and mother's job), four questions on midwifery factors (body mass index, cesarean section length, gestational age, and reason for cesarean section), and three questions on factors after cesarean delivery (time to starting daily activities). This questionnaire was completed by interviewing mothers at the time of enrollment, 24 hours after the cesarean section, and nine days after the cesarean section. The second instrument was the REEDA cesarean scale, which was used to measure redness, edema, bruising, discharge from the wound, and edge adhesion. The mother was asked to lie down; then, a paper strip was placed vertically on the site of the cesarean section in a way that the midpoint of the tape was logically cut on the cesarean section site. Finally, a score from zero to three was given to each of the five criteria: Redness: no redness score 0 and a redness 0.5 cm from each side of surgery site score 3; Edema: no edema sore 0, edema less than 1 cm from the site score 1, edema 1 - 2 cm from the site score 2, and edema more than 2 cm from the site score 3; Ecchymosis: no edema sore 0, ecchymosis 0.25 cm from both sides or 0.5 to 2 cm from one side score 1, ecchymosis 1 cm from both sides or 0.5 to 2 cm from one side score 2, and ecchymosis more than 1 cm from both sides or more than 2 cm from one side score 3, Secretions: no discharge score 0, serous secretion score 1, hydro rhea and bloody secretion score 2, and bloody and purulent secretion score 3; Continuity: two edges of the scar are closed score 0, the distance between two edges of skin is less than or equal to 3 mm score 1, the skin and under-skin of both edges are separated score 2, and the fascia layer is separated score 3.
Scores obtained from all five criteria were summed; score 0 represented complete healing, and score 15 represented low healing. The REEDA index is a tool introduced in 1974 by Davidson to investigate the scar by assessing the redness, edema, ecchymosis, discharge, and continuity (19). Malekpor et al. confirmed the validity of the scale for investigating episiotomy healing (20). Amani et al. (2015) also investigated its reliability, which was 0.85 (21).
In this research, the content validity method was used to determine the validity of data gathering tools. Therefore, the researcher prepared the tool considering the research goal and by studying books, related theses, and valid papers. After the tutors confirmed it, the statistics consultant developed the questionnaire, and then the prepared tool was investigated by 10 professors of the Iran School of Nursing and Midwifery. Next, the tool was modified using the comments and suggestions, and to obtain the final approval, it was sent to the research committee to assess and confirm the content of the questionnaire. The final modification was done using the research experts’ opinions.
The observation method (by the researcher and his/her trained fellow) was used to investigate the reliability of the research tool that 0.87 Pearson correlation coefficient (For the reliability of Reeda instrument, the observation method (by the researcher and the trained companion) was used, the coefficient of which was obtained based on Pearson correlation.) was obtained. After approval of the research plan by the Ethics Committee of Iran University of Medical Sciences, the researcher referred to the research setting and after explaining the research goal and methods to the authorities and receiving permission, presented at the Gynecology Department and invited nulliparous and multiparous women who were candidates for cesarean section and had the inclusion criteria to participate in the study. First, the research method was completely explained to the patients, and they signed informed consent forms. A continuous sampling method was used, and the subjects were randomly assigned to control or intervention groups via a coin. A pretest was done, and then a training booklet was taught by the researcher during a 45 - 60 min training session using the face-to-face method. The booklet was about surgical scar care, including nutrition, health observance, how to change wound dressing, movement, and activity. A posttest was also done to assess the learning process. The reason for doing the pretest and posttest was to insure the patient learning. At the end of the session, the booklet was given to the patients, and both intervention and control groups received routine care services. The assessment of surgery site healing was done after 24 hours and nine days of cesarean section in the surgery ward of the clinic by the researcher using the REEDA tool. Data were analyzed by IBM SPSS software version 20. The statistical indices (frequency, percentage, standard deviation, and mean) and tests (independent t-test, Fisher's exact test, Wilcoxon, and Friedman tests) were used to investigate the significance. The normality of data was evaluated using the Kolmogorov-Smirnov test. The significance level of the study was set at P < 0.05.
4. Results
The results of the independent t-test showed no significant difference in age between the two groups (P < 0.71). About 40% of people in the experimental group had a moderate economic status of 54.4%, and in the control group, they had a weak economic situation. Besides, 41.7% in the intervention group had high school education, and 29.7% in the control group had intermediate education. Also, 10% of the intervention group subjects and 89.2% of the control group subjects were housewives. More than 97% of the subjects in both groups were not trained before. There was no significant difference between the groups in terms of Body Mass Index (BMI) (P < 0.39). The mean BMI was 28.45 in the intervention groups and 27.88 in the control group.
The results related to obstetrics and neonatal factors showed that the two groups had no statistically significant difference in terms of gestational age according to the first day of the last menstrual period (P < 0.61). There was no statistically significant difference between the two groups in terms of gestational age according to the ultrasound of the first trimester of pregnancy (P < 0.15). There was no significant difference in pain intensity and wound healing gestational age in terms of ultrasound using Pearson correlation. The rest of the individual characteristics is shown in Table 1.
Demographic Characteristics of Mothers in Two Groups and Comparison of Means
Comparing patients in the wound healing score 24 hours and nine days after the cesarean section showed that there was no significant difference between the two groups 24 hours after cesarean section (P < 0.28). Besides, 24 hours after cesarean, there was no significant difference between the two groups concerning edema (P < 0.69), and continuity was seen among 80.6% of the intervention group and 51.4% of the control group. Nine days after the cesarean section, there was no significant difference between the two groups concerning redness (P < 0.5), and there was no significant difference between the two groups in terms of ecchymosis (P < 0.30). Also, 86.1% of the intervention group and 73% of the control group had no secretions. After nine days of cesarean section, the two groups had no statistically significant difference (P < 0.16). Besides, 94.4% in the experimental group and 70.3% in the control group had their wounds closed. There was a statistically significant difference between the two groups (P = 0.007) (Table 2).
| Criteria for Wound Healing Over Time and Signed Rank | Group, No. (%) | Pa | |
|---|---|---|---|
| Intervention | Control | ||
| 24 hour after cesarean section (Redness) | 0.28 | ||
| There was no redness (0) | 30 (81) | 27 (73) | |
| Redness 0.25 cm from each side of surgery site (1) | 4 (10.8) | 4 (10.8) | |
| Redness 0.5 cm from each side of surgery site (2) | 3 (8.1) | 6 (16.2) | |
| Nine days after cesarean section (Redness) | 0. 5 | ||
| There was no redness (0) | 32 (88.9) | 26 (70.3) | |
| Redness 0.25 cm from each side of surgery site (1) | 4 (11.1) | 11 (29.7) | |
| Redness 0.5 cm from each side of surgery site (2) | |||
| Pb | 0.18 | 0.24 | |
| 24 hour after cesarean section (Edema) | 0.69 | ||
| There was no edema (0) | 30 (81) | 31 (83.8) | |
| Edema less than 1 cm from site | 4 (10.8) | 6 (16.2) | |
| Edema 1-2 cm from site | 3 (8.1) | 0 | |
| Nine days after cesarean section (Edema) | 0.01 | ||
| There was no edema (0) | 32 (88.9) | 23 (62.2) | |
| Edema less than 1 cm from site | 3 (8.3) | 14 (37.8) | |
| Edema 1-2 cm from site | 1 (2.8) | 0 (0) | |
| Pb | 0.19 | 0.96 | |
| 24 hour after cesarean section (Ecchymosis) | 0.39 | ||
| There was no ecchymosis | 28 (77.8) | 25 (67.6) | |
| Ecchymosis 0.25 cm from both sides or 0.5 to 2 cm from one side (1) | 6 (16.6) | 11 (29.7) | |
| Ecchymosis 1 cm from both sides or 0.5 to 2 cm from one side (2) | 2 (5.6) | 1 (2.7) | |
| Nine days after cesarean section (Ecchymosis) | 0.30 | ||
| There was no ecchymosis | 33 (91.7) | 31 (83.8) | |
| Ecchymosis 0.25 cm from both sides or 0.5 to 2 cm from one side (1) | 3 (8.3) | 6 (16.2) | |
| Ecchymosis 1 cm from both sides or 0.5 to 2 cm from one side (2) | 0 | 0 | |
| Pb | 0.08 | 0.06 | |
| 24 hour after cesarean section Secretion | 0.97 | ||
| There was no secretion | 26 (72.2) | 27 (73) | |
| Serous | 4 (11.1) | 4 (10.8) | |
| Hydrorrhea and bloody | 6 (16.7) | 5 (13.5) | |
| Bloody and purulent | 0 (0) | 1 (2.7) | |
| Nine days after cesarean section (Secretion) | 0.16 | ||
| There was no secretion | 31 (86.1) | 27 (73) | |
| Serous | 5 (13.9) | 10 (27) | |
| Hydrorrhea and bloody | 0 (0) | 0 (0) | |
| Bloody and purulent | 0 (0) | 0 (0) | |
| Pb | 0.05 | 0.94 | |
| 24 hour after cesarean section (Continuity) | 0.01 | ||
| Two edges of the scar are closed | 29 (80.6) | 19 (51.4) | |
| The distance between two edges of skin are less than or equal to 3 mm | 6 (16.6) | 18 (48.6) | |
| Skin and under-skin of both edges are separated | 1 (2.8) | 0 (0) | |
| Nine days after cesarean section (Continuity) | 0.007 | ||
| Two edges of the scar are closed | 34 (94.4) | 26 (70.3) | |
| The distance between two edges of the skin are less than or equal to 3 mm | 2 (5.6) | 10 (27) | |
| Skin and under-skin of both edges are separated | 0 (0) | 1 (2.7) | |
| Pb | 0.08 | 0.13 | |
Comparison of Wound Healing Scores 24 Hours and Nine Days After Cesarean Section in Control and Intervention Groups
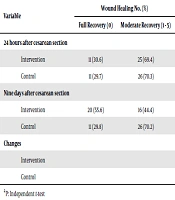
The independent t test showed that both groups had no significant differences 24 hours after cesarean section in wound healing (P < 0.13). The mean and standard deviation of wound healing were 1.1 ± 39.38 in the intervention group and 1.1 ± 92.60 in the control group, such that 69.4% of the intervention group and 70.3% of the control group had a moderate wound healing (Table 3).
| Variable | Wound Healing, No. (%) | Mean ± SD | Pa | |
|---|---|---|---|---|
| Full Recovery (0) | Moderate Recovery (1 - 5) | |||
| 24 hours after cesarean section | 0.13 | |||
| Intervention | 11 (30.6) | 25 (69.4) | 1.1 ± 39.38 | |
| Control | 11 (29.7) | 26 (70.3) | 1.1 ± 92.60 | |
| Nine days after cesarean section | 0.001 | |||
| Intervention | 20 (55.6) | 16 (44.4) | 0.0 ± 53.65 | |
| Control | 11 (29.8) | 26 (70.2) | 1.1 ± 43.28 | |
| Changes | 0.001 | |||
| Intervention | - 0.1 ± 86.38 | |||
| Control | - 0.1 ± 49.79 | |||
Numerical Indices of Wound Healing 24 hours and Nine Days After Cesarean Section in Both Groups
The independent t test results also showed a significant difference between the two groups nine days after cesarean section in wound healing (P = 0.001) so that 55.6% of the studied sites in the intervention group had complete improvement and 67.6% of the control group had moderate improvement (Table 3).
5. Discussion
This study was done to determine the effect of a self-care training program on cesarean section site healing in women. The independent t test results showed significant differences between the two groups nine days after cesarean section in wound healing. More than half of the intervention group had complete or moderate wound healing. Razmjoo et al. (2013) evaluated the effect of early nutrition after the cesarean section on wound healing. In this study, although the process of cesarean section wound healing was better in the early feeding group, this difference was not statistically significant. The researchers concluded that early feeding had no effect on cesarean section healing but reduced the severity of postoperative pain and bloating (22). Mohamad (2012) examined the effect of personal perineal care instructions on episiotomy pain and wound healing in postpartum women. The researchers concluded that clients who were trained and practiced perineal care instructions experienced less pain with daily postpartum activities such as walking, sitting, urinating, and defecating, and the healing of epithelial wounds speeded up in them. Episiotomy repair was also faster (23). The results of a quasi-experimental study of 60 primiparous women at Al-Balady Maternity Hospital in Baghdad showed that patients in the intervention group benefited from the implementation of instructions, and there was a significant change in personal care awareness of their episiotomy and perineum (24).
A study by Chan et al. (2014) also showed no significant difference between patients whose scar was dressed by nurses and patients who changed their wound dressing at home based on telephone training (18). These results are consistent with our study. The studies have shown that the patients’ lack of awareness of self-care is one of the most important reasons for prolonged hospitalization, readmission, and experiencing related complications. Therefore, training self-care behaviors with proper and effective methods can be effective in improving life quality, individual health, and community health and reduce costs (25).
Nurses as people who have close and constant contact with patients have enough time and ability to become familiar with patients and can choose the best method to train health behaviors and self-care content(26). Patients are more intended to receive information from their nurses concerning self-care (27). Nurses at health centers can make more efforts to research and implement best practices for wound care. Training programs are one of the important factors in health care and scar control (28). One of the limitations of the study was that the study population was small.
5.1. Conclusions
Given that the mother health is an index of the country’s health system, which is achieved through the development of health care services, developing the cesarean section site and preventing post-cesarean complications are of the goals of the health system, which will be followed by the mother and baby health. Besides, nurses play an important role in maintaining and improving the mothers’ health. Therefore, it can be concluded that implementing training programs is beneficial in increasing self-care of the cesarean section site, and implementing such programs has an effective role in increasing the scar healing rate.