1. Background
Childbirth is one of the gifts of God for the reproduction of the human race on earth. It is a spontaneous process without the need for any external intervention (1). Currently, two modes of delivery are available: vaginal and cesarean section (C-section). Vaginal delivery is known as the best mode of delivery (2). C-section, as a surgical intervention, should be limited to cases with maternal or fetus risk during pregnancy or childbirth (3). For mothers, unnecessary C-section is associated with increased risk of some complications, including bleeding, infection, postpartum hemorrhage, wound infection, and endometritis. Also, for fetus, it may cause complications such as fetal injury, respiratory problems, and low Apgar scores (4). A large cross-sectional study conducted by the World Health Organization (WHO) from 2004 to 2008 reported that C-section is associated with an increased risk of death, intensive care unit admission, and hysterectomy for mothers (5). A study has estimated that years of life lost (YLL) due to C-section is nearly 26.6 per 1000 deliveries, due to both premature mortality or disability. While for the vaginal delivery it’s 8.8 (6).
In addition to negative health outcomes for mother and fetus, C-section is also costly for both families and the health system (7). For example, consequences such as death, infection, long hospital stay, heavy expenditures, and injury to the fetus are more likely in C-section (8-10). Also, several studies have reported that C-section is associated with reduced fertility (11). Due to these complications, WHO emphasized that only 10% - 15% of deliveries should be undertaken through C-section (12).
C-section rates are on the rise worldwide, particularly in developing countries that are experiencing dramatic rates. For example, in Chile, China, and Brazil, the C-section rate is more than 40% (6). The situation is even more alarming in Iran. So that a study conducted in 2016 on pregnant women in Tehran reported a rate of 72% for C-section (4). As most of the C-sections in Iran are not based on clinical indications, it can be argued that many of them are unnecessary. The International Federation of Gynecology and Obstetrics emphasized that it is not ethical to undertake C-section without a medical reason (13, 14). Recent population policies of Iran are intended to increase the fertility rate, and since women who give birth by C-section prefer to have fewer children, the rate of C-section is an important challenge for these policies (13). According to the policies of the Ministry of Health, the rate of C-section in public and private hospitals of Iran should decrease to 20% and 25%, respectively (14). In this line, it seems reasonable to identify and examine factors contributing to women’s tendency to C-section to provide information for developing appropriate strategies to reduce its rate. According to the literature, several factors affect the choice of C-section over vaginal delivery, for example, obstetric risk factors such as having a history of C-section or miscarriage, blood pressure disorders, multiple pregnancies, and maternal obesity (15, 16).
Additionally, demographic and social characteristics of mothers and cultural factors such as age, education, occupation, and place of residence are also reported to have a strong correlation with the delivery mode (17).
Also, according to the literature, cognitive factors such as lack of proper knowledge about the complications of C-section and incorrect information, as well as a negative attitude toward natural delivery, heavily influence mothers’ tendency to C-section (2). Moreover, it’s confirmed that socioeconomic status affects the utilization of health care services, including C-section (4). Two studies conducted in China and Brazil reported that socioeconomic status is associated with women’s tendency to choose C-section (7, 18). Furthermore, psychological factors such as fear of labor pain heighten women’s tendency to C-section (19-21), so that nearly 6% - 10% of women fear of labor pain, which can disrupt the labor process (22-24). The results of a study performed on pregnant women in Tehran indicated that 74.3% of participants chosen C-section due to fear of labor pain (25).
Regarding the impact of various factors affecting the women’s tendency to C-section and the alarming rise of unnecessary C-section and its associated harmful consequences for both mother and child, the current study aimed to investigate the main factors contributing to women’s tendency to choose C-section among pregnant women in 2019. It is hoped that the findings be valuable for policy-makers to develop policies/programs intended to reduce C-sections in Iran based on the socio-cultural and economic context of the country.
2. Methods
This cross-sectional descriptive-analytical study investigated factors contributing to women’s tendency to C-section as opposed to vaginal delivery in Lorestan province of Iran in 2019. After obtaining the approval of the Ethics Committee of the Lorestan University of Medical Sciences (IR.LUMS.REC.1398.247), the multi-stage sampling technique was used to select the participants. It worth noting that all cities of the province were considered as distinct clusters. After randomly selecting a number of cities, their health centers were identified and mapped. Then, using systematic sampling, the desired centers of each city were determined for recruiting participants. Afterward, using the random sampling technique, participants were randomly chosen based on the number of their medical records in local health centers. Cochran formula was used to estimate the sample size, which yielded a sample size of 196.
Where
P = 0.48, q = 0.52, d = 0.07, α = 0.05, and 1.96 Z1-α/2 (1).
Since to observe the study design effects, the cluster sampling technique was used, the minimum sample size had to be 196 × 1.5 = 294. However, in total, 320 women aged 15 to 49 years in the second and third trimesters of pregnancy were recruited to participate in the current study. The inclusion criteria were as follow being in the second or third trimesters of pregnancy, willingness to participate, lack of medical and obstetric problems in the current pregnancy, and indication for C-section. Data were collected using a demographic form, Fear of Pain Questionnaire (FPQ), and Knowledge and Attitude about Delivery Methods scale. Personal characteristics were categorized into three categories: demographic and socio-cultural information (age, occupation, mother’s education, spouse’s education, and fetal gender), economic information (monthly income and type of health insurance), and medical records (history of abortion, history of previous C-section, and body mass index (BMI)). The FPQ consists of 14 questions that are scored using a 4-point Likert scale (never, very low, medium, and very high). The total FPQ score ranges from 14 to 56. Accordingly, a score of 28 or more indicated the fear of labor pain. The reliability of the FPQ is investigated by international and internal studies, that in the latter, it’s reported as 0.75 (using Cronbach’s alpha), by Khorsandi et al., and in the former, it’s reported as 0.80 (26-28). To measure mothers’ knowledge and attitude toward delivery mode, a pre-designed questionnaire was used. The knowledge questionnaire consists of 10 items. That each correct answer has a score of one, while for incorrect answers, it’s zero. Mothers’ knowledge score was classified into three categories (good = 7 - 10, moderate = 4 - 6, and poor = 0 - 3). The attitude questionnaire consists of twenty items (8 questions on vaginal delivery and 12 on C-section) that are rated on a 5-point Likert scale: completely agree = 1, agree = 2, no idea = 3, disagree = 4, and completely disagrees = 5 (29). Respectively, a score of 8 - 16, 17 - 24, and 25 - 40 indicates a positive attitude, neutral attitude, and negative attitude toward vaginal delivery. On the other hand, a score of 12 - 24, 25 - 36, and 37 - 60 represent a positive attitude, neutral attitude, and negative attitude toward the C-section, respectively. The validity of this instrument is supported by 10 obstetricians; the reliability of the knowledge subscale of this instrument is also approved using a Kuder-Richardson coefficient of 0.67, and the reliability of the attitude subscale is confirmed using a Cronbach’s alpha of 0.7 (29, 30). First, the objectives of the research were explained to the participants, then, if they agree, written informed consent was obtained. All participants were assured about the confidentiality of the data. We also provided the participants with some explanations about the questionnaires, and then they were asked to complete them as self-reports.
Descriptive and analytical statistics were used to analyze the data. First, the relative frequency, mean, and standard deviation of each of the variables were calculated. Then, the univariate analysis and multivariate logistic regression model were used to analyze the data. Independent variables that had a P value lower than 0.3 in the univariate analysis were included in the multivariate logistic regression model. All analyses were performed using Stata version 14 at the significance level of P < 0.05.
3. Results
Based on the results, 48.44% of pregnant women preferred C-section, which 34.19% of them had a history of C-section. The mean (standard deviation) age of participants was 29.35 ± 5.93. Women in the vaginal delivery group were significantly younger than those in the C-section (P < 0.001). Also, employment was higher in the C-section group than the vaginal delivery (P < 0.001). In terms of education, the number of women with a university degree was significantly higher in the C-section group (56.13%) than the vaginal delivery group (27.22%) (P < 0.001). The C-section group had a better economic status (P < 0.001) and a lower BMI than the other group (P < 0.001). In terms of insurance coverage, 4.85% of the vaginal delivery group and 23.87% of the C-section group had supplementary insurance coverage. The mean score of fear of labor pain in the C-section group was significantly higher than the vaginal delivery group (P < 0.001). Women in the vaginal delivery group had a significantly better attitude toward vaginal delivery (P < 0.001). Conversely, women in the C-section group had a better attitude toward C-section (P < 0.001). The chi-square test revealed no significant difference between the two groups concerning the knowledge about delivery modes (P = 0.64) (Table 1).
| Category/Variable | Total (N = 320) | Vaginal Delivery (N = 165) | C-Section (N = 155) | P Value |
|---|---|---|---|---|
| Demographic, Social, and Cultural Factors | ||||
| Mother’s agea | 29.35 (5.93) | 28.32 ± 6.28 | 30.45 ± 5.34 | 0.001 |
| Mother’s occupationb | < 0.001 | |||
| Housewife | 287 (89.69) | 158 (95.76) | 129 (83.23) | |
| Employed | 33 (10.31) | 7 (4.24) | 26 (16.77) | |
| Mother’s educationb | < 0.001 | |||
| Non-academic | 224 (70) | 130 (78.78) | 94 (60.65) | |
| Academic | 96 (30) | 35 (21.22) | 61 (39.35) | |
| Father’s educationb | < 0.001 | |||
| Non-academic | 188 (58.75) | 120 (63.83) | 68 (43.87) | |
| Academic | 132 (41.25) | 45 (27.27) | 87 (56.13) | |
| Fetus genderb | 0.002 | |||
| Male | 168 (53.44) | 74 (44.85) | 97 (62.59) | |
| Female | 149 (46.56) | 91 (55.15) | 58 (37.41) | |
| Economic Factors | ||||
| Household monthly incomeb | < 0.001 | |||
| Below 2,000,000 | 50 (15.63) | 34 (20.61) | 16 (10.32) | |
| 2,000,000 - 3,000,000 | 165 (51.56) | 107 (64.85) | 58 (37.42) | |
| Above 3,000,000 | 105 (32.81) | 24 (14.54) | 81 (52.26) | |
| Insuranceb | < 0.001 | |||
| None | 59 (18.44) | 39 (23.64) | 20 (12.9) | |
| Basic insurance | 216 (67.5) | 118 (71.51) | 98 (63.23) | |
| Basic & complementary insurance | 45 (14.06) | 8 (4.85) | 37 (23.87) | |
| Medical Factors | ||||
| History of abortionb | 0.244 | |||
| Yes | 50 (15.63) | 22 (13.33) | 28 (18.06) | |
| No | 270 (84.38) | 143 (86.67) | 127 (81.94) | |
| History of C-sectionb | < 0.001 | |||
| Yes | 55 (17.19) | 2 (1.21) | 53 (34.19) | |
| No | 265 (82.81) | 163 (98.79) | 102 (65.81) | |
| Mother’s BMI (kg/m2)a | 25.34 (3.64) | 25.85±4.26 | 24.8±2.74 | 0.0098 |
| Cognitive Factors | ||||
| Knowledge of delivery methodsb | 0.64 | |||
| Poor (3 - 0) | 15 (4.69) | 9 (5.45) | 6 (3.87) | |
| Moderate (6 - 4) | 224 (70) | 112 (67.88) | 112 (72.26) | |
| Good (10 - 7) | 81 (25.31) | 44 (26.67) | 37 (23.87) | |
| Attitude to vaginal deliveryb | < 0.001 | |||
| Negative (40 - 25) | 47 (14.69) | 1 (0.60) | 47 (30.32) | |
| Neutral (24 - 17) | 120 (37.5) | 44 (26.67) | 75 (48.39) | |
| Positive (16 - 8) | 153 (47.81) | 120 (72.73) | 33 (21.29) | |
| Attitude to C-sectionb | < 0.001 | |||
| Negative (60 - 37) | 52 (16.25) | 47 (28.48) | 5 (3.23) | |
| Neutral (36 - 25) | 177 (55.31) | 93 (56.36) | 84 (54.19) | |
| Positive (24 - 12) | 91 (28.44) | 25 (15.16) | 66 (42.58) | |
| Physiological Factors | ||||
| Fear of labor paina | 38.16 (8.5) | 36.46 ± 8.62 | 39.98 ± 8.21 | < 0.001 |
aT-test
bChi-squared test
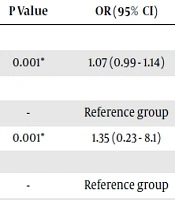
Based on the results of univariate analysis, the tendency to C-section is positively associated with the following factors: increased age of the mother, increased level of education of the mother and her husband, employment of the mother, increased level of household income, having supplementary insurance coverage, improved attitude toward C-section, previous C-section, and increased fear of labor pain (P = 0.01). On the other hand, increased BMI (P = 0.01) and the female gender of the fetus (P = 0.002) were negatively associated with the women’s tendency to C-section. Knowledge about delivery modes and having a history of abortion did not show a significant association with the tendency to C-section (P = 0.25). The results of multivariate logistic regression analysis showed that increased maternal age (OR = 1.07) and increased level of education of the spouse (OR = 2.62) are associated with more tendency to C-section. Moreover, it was found that an improved attitude toward vaginal delivery reduces the tendency to C-section, but an improved attitude toward C-section exerts a positive effect on the tendency to undertake this type of delivery. Also, the higher the income of the pregnant women, the more was the tendency to C-section (OR = 6.24). Fear of labor pain (OR = 1.04) and having a history of C-section were positively associated with the tendency to C-section. Besides, the female gender of the fetus (OR = 0.36) and the increase in BMI (OR = 0.74) had a decreasing effect on women’s tendency to C-section (Table 2).
| Category/Variable | Univariate Analysis | Multivariate Analysis | ||
|---|---|---|---|---|
| OR (95% CI) | P Value | OR (95% CI) | P Value | |
| Demographic, Social, and Cultural Factors | ||||
| Mother’s age | 1.06 (1.02 - 1.1) | 0.001* | 1.07 (0.99 - 1.14) | 0.09 |
| Mother’s occupation | ||||
| Housewife | Reference group | - | Reference group | |
| Employed | 4.55 (1.91 - 10.8) | 0.001* | 1.35 (0.23 - 8.1) | 0.73 |
| Mother’s education | ||||
| Non-academic | Reference group | - | Reference group | - |
| Academic | 2.41 (1.47 - 3.94) | < 0.001* | 2.3 (0.8 - 6.4) | 0.12 |
| Father’s education | ||||
| Non-academic | Reference group | - | Reference group | - |
| Academic | 3. 41 (2.14 - 5.44) | < 0.001* | 2.79 (1.06 - 7.29) | 0.036* |
| Fetus gender | ||||
| Male | Reference group | - | Reference group | - |
| Female | 0.49 (0.31 - 0.76) | 0.002* | 0.36 (0.15 - 0.86) | 0.023* |
| Economic Factors | ||||
| Household monthly income | ||||
| Below 2,000,000 | Reference group | - | Reference group | - |
| 2,000,000 - 3,000,000 | 1.15 (0.59 - 2.26) | 0.68 | 1.3 (0.37 - 4.45) | 0.68 |
| Above 3,000,000 | 7.17 (3.4 - 15.2) | < 0.001* | 5.9 (1.25 - 27.7) | 0.024* |
| Insurance | ||||
| None | Reference group | - | Reference group | - |
| Basic insurance | 1.61 (0.89 - 2.95) | 0.12 | 1.03 (0.29 - 3.7) | 0.97 |
| Basic & complementary insurance | 9.02 (3.5 - 22.98) | < 0.001* | 1.99 (0.34 - 11.7) | 0.44 |
| Medical Factors | ||||
| History of abortion | ||||
| Yes | Reference group | - | Reference group | - |
| No | 0.69 (0.38 - 1.28) | 0.25 | 0.53 (0.18 - 1.5) | 0.23 |
| History of C-section | ||||
| Yes | Reference group | - | Reference group | - |
| No | 0.024 (0.006 - 0.1) | < 0.001* | 0.001 (0.0001 - .018) | < 0.001* |
| Mother’s BMI (kg/m2) | 0.91 (0.84 - 0.98) | 0. 01* | 0.75 (0.64 - 0.88) | 0.000* |
| Cognitive Factors | ||||
| Knowledge of delivery methods | ||||
| Poor | Reference group | - | Reference group | - |
| Moderate | 1.5 (0.52 - 4.35) | 0.45 | ||
| Good | 1.26 (0.41 - 3.87) | 0.68 | ||
| Attitude to vaginal delivery | ||||
| Negative | Reference group | - | Reference group | - |
| Neutral | 0.036 (0.005 - 0.27) | 0.001* | 0.04 (0.003 - 0.38) | 0.01* |
| Positive | 0.006 (0.0008 - 0.044) | < 0.001* | 0.007 (0.0006 - 0.08) | < 0.001* |
| Attitude to C-section | ||||
| Negative | Reference group | - | Reference group | - |
| Neutral | 8.49 (3.22 - 22.35) | < 0.001* | 12.3 (2.2 - 69.1) | 0.004* |
| Positive | 24.8 (8.85 - 69.54) | < 0.001* | 33.8 (5.4 - 211.8) | < 0.001* |
| Psychological factors | ||||
| Fear of labor pain | 1.05 (1.02-1.08) | < 0.001* | 1.04 (0.988 - 1.09) | 0.13 |
Abbreviations: CI, confidence Interval; OR, odds ratio
aValue is given as mean ± standard deviation or number (percentage).
4. Discussion
The current study aimed to investigate factors contributing to the women’s tendency to C-section in the Lorestan province, which was 48.44%, which is higher than the global average (18.6%) (31). In a cross-sectional study conducted on pregnant women admitted to Imam Khomeini Hospital in Tehran, the tendency for C-section is reported as 45%, which is close to the findings of the present study (32). In another study conducted in 2016 on pregnant women in Tehran, the rate of C-section was 72%, which was significantly higher in private than public hospitals (4). Dadipour et al. examined the trend of C-section in Iran and some selected countries. They reported that, in Iran, this rate increased from 16% in 1985 to 64% in 2013 (33). As could be inferred from the above discussion, the tendency to C-section is strong and has been increasing over time. Therefore, health policymakers and healthcare providers should focus their efforts on reducing unnecessary C-sections and facilitating vaginal delivery.
The results of the present study showed that maternal age is a predictor for the increased tendency to cesarean delivery. Several studies have indicated that the chance of cesarean delivery is higher among older women (34, 35). In a study conducted in 2010, it was found that the overall prevalence of C-section in mothers over 35 years was about twice more than that of mothers younger than 20 years (36). In their cross-sectional study, Moosavi et al. concluded that the older the women during pregnancy, the higher would be the tendency to C-section (2). Older women are believed to be more likely to develop pregnancy-related complications, which necessitates the cesarean delivery (37). While Safari-Moradabadi et al. argued that the tendency to C-section was higher in women younger than 20 years. In this study, age was the strongest predictor of vaginal delivery (20). This discrepancy can be attributed to the differences in the samples of these two studies, that in the present study, the participants included mothers who experienced their first pregnancy. Since the tendency to cesarean delivery grows with mothers’ age, it is recommended that healthcare providers educate and encourage the community not to postpone pregnancy to older ages.
In the present study, the mother’s higher level of education was not significantly associated with the tendency to C-section (OR = 2.24), but the husband’s education level was positively associated with the tendency C-section (OR = 2.62). A study performed in Tehran (2016) reported that the couple’s education level had a significant association with C-section (4). The results of other studies have also revealed that a mother’s high level of education is one of the factors associated with an increased inclination toward C-section (2, 3). Tang et al. reported a significant relationship between preference for C-section and the level of mother’s education. They argued that women choose cesarean delivery because of factors such as fear of labor pain, delivery on a particular day, protection of the baby’s brain, and concerns about sexual life after vaginal delivery, all of which are more common among educated women (38). Another reason why more educated women are more likely to prefer cesarean delivery is that they are usually employed, and they often can afford the costs more easily. Also, more educated people are usually ignored by health educators when it comes to raising their awareness about the advantages and disadvantages of different delivery modes. If such an argument is true, it is crucial to pay more attention to training these people. However, a study conducted in Bandar Abbas noted that the tendency to C-section is inversely related to the level of education of pregnant women because people with lower levels of education are more likely to have less knowledge and awareness about the adverse effects of C-section (20).
This study showed that the higher the income, the more would be the tendency to C-section. In another cross-sectional study, after adjusting for mothers’ demographic characteristics, the economic status of participants was associated with an increased tendency to C-section (4). Klemetti et al. found that household income was a strong predictor of cesarean delivery in rural China (39). Several studies have reported that mothers with higher socioeconomic status have more tendency to C-section (2, 13, 17, 20). Indeed, mothers with higher socioeconomic backgrounds are more likely to have sufficient financial resources to pay for C-section. Having a high economic status is associated with modern ways of living, and C-section is considered a symbol of high social status. Therefore, the dominance of such stereotypes in society greatly inhibits efforts to reduce the rate of C-section.
The results of the present study also showed that an improved attitude toward vaginal delivery decreases the tendency to C-section, but improved attitude toward C-section causes a positive impact on the tendency to C-section. In a cross-sectional study conducted on pregnant women in Isfahan in 2017, the authors reported that attitudes can determine the delivery mode in 81.9% of cases (14). Yosefvand et al. reported that people who intended to have vaginal delivery had a more positive attitude toward this kind of delivery, and there was a significant difference in attitudes of the two groups who were going to undergo vaginal delivery or C-section. The results of this study confirmed that having a negative attitude toward natural delivery increases the women’s fear (40), highlighting the importance of fostering a positive attitude in pregnant women toward this method of delivery. In this regard, it is necessary to design comprehensive training programs and integrate them into routine pregnancy programs.
This study also showed that about 70% of the study population had moderate knowledge about delivery modes. However, other studies (2011, 2013) have substantiated the effect of educational interventions and increasing mother’s knowledge on delivery mode and reducing the rate of C-section (41, 42). Consequently, it is imperative to encourage pregnant women to raise their knowledge about delivery modes and to obtain accurate information.
Fear of labor pain (OR = 1.04) strengthens the tendency to C-section. In studies by Moosavi et al. and Ghotbi et al., fear of labor pain is reported as the most important reason for choosing C-section (2, 29). Johanson et al. stated that most of the pregnant women agreed that cesarean delivery is easier than vaginal delivery (43). Several studies indicated that women who are willing to give birth by C-section are more afraid of labor pain (1, 44-46). Experiencing lower pain, as the most remarkable advantage of this delivery mode, is the most important reason for C-section popularity. It seems that organizing delivery preparation classes by prioritizing women who more afraid of labor pain can be an effective measure to mitigate such fear. Pirdadeh Beiranvand et al. found that the fear of labor pain in women who did not attend childbirth preparation classes was twice as much as those who took part in such classes (47). Since the most frequently mentioned reason for fear of labor pain in Iranian women is related to hospital equipment and low quality of care (48), it seems that promoting and implementing new low pain methods of vaginal delivery, such as the introduction of water birth, can be effective in reducing C-section rates. The present study showed that having a history of C-section increases the tendency for this mode of delivery, which is consistent with the results of some other studies (16, 49). A study performed in Dutch reported a success rate of 60% - 80% for vaginal delivery after C-section (19, 50). Increased BMI (OR = 0.74) is negatively associated with women’s tendency to C-section, such that people who preferred C-section had a lower BMI than people who preferred vaginal delivery. In the study by Amini et al. in Tehran and another study in Mongolia, the authors reported that the baby’s head circumference and the mother’s BMI are positively associated with more tendency to C-section (51, 52), which is not in line with the results of the present study. This discrepancy can be attributed to the fact that in the present study BMI of participants was in the normal range. Since obesity is a risk factor for pregnant women and increases the likelihood of C-section (52), it is recommended that further studies be performed to determine the association between the mother’s BMI and the tendency to C-section. The current study had limitations that should be considered when interpreting its results. Although it should be reminded that the results are not generalizable to all pregnant women. Also, the self-report method of completing the questionnaires is an important limitation of the present study.
5.1. Conclusion
The results of this study showed that although vaginal delivery is popular among pregnant women in Lorestan province, but the tendency to C-section is strong. This corroborates the need to develop and implement appropriate interventions intended to reduce unnecessary C-sections. Increased level of education of mother and husband, high income, negative attitude toward vaginal delivery, fear of labor pain, and old age were the main factors contributing to the women’s tendency toward C-section in this study. Considering the various factors that raise the tendency to C-section, one can take a number of measures to curb unnecessary cases of this mode of delivery, including training families, particularly pregnant women, about the advantages and disadvantages of various modes of delivery, empowering mothers to overcome fears of labor pain through mass media and health care providers, promoting and using new low pain techniques of vaginal delivery, and encouraging women’s participation in childbirth preparation programs.