1. Background
The physiological process of childbirth is the same for everyone, but women have a different perception of this event. This perception is influenced by cultural beliefs, traditions, and other variables (1). The psychological stress of the mother during difficult childbirth is a negative and unpleasant experience for them. Although it may decline over time, it sometimes lasts up to five years after childbirth (2). Mothers’ perception of events during childbirth is crucial in causing traumatic childbirth and does not deal with the views of others, including health care providers. The childbirth process may be normal for caregivers, but it may seem traumatic to the mother. Beck describes several important factors as factors influencing the psychological trauma of childbirth (3), which leads to the different prevalence of traumatic childbirth in different countries so that it has been reported to be 7% in Sweden, 9.3% in Canada, 34% in Atlanta, and 31.8% in Israel (4). However, in general, its prevalence in the world is 20% - 40% (5), and it has been reported up to 48.3% in Iran (6).
The experience of traumatic childbirth can negatively influence a woman’s emotional health (7). Severe nausea and vomiting during pregnancy, stressful childbirth events, fear of childbirth, pregnancy-related problems, previous traumatic childbirth, instrumental childbirth, gestational depression, history of mental health problems, insufficient support, older mothers, domestic violence, unwanted pregnancy, and hospitalization of infants in the intensive care unit are among the risk factors for traumatic childbirth (6, 8). Traumatic childbirth has a negative impact not only on women’s lives and health but also on childbearing, pregnancy, and subsequent childbirths, so that 38% of women with a history of traumatic childbirth, compared to 17% of women who had a positive experience of childbirth, no longer wanted to give birth (2). The negative experience of traumatic childbirth includes symptoms, such as re-experiencing the accident or event in various forms, annoying thoughts, avoidant behaviors, negative mood and cognition, arousal, emotional numbness, nightmares, feelings of shame, anger, and fear. The range of negative consequences of traumatic childbirth varies from low self-esteem to sexual problems, fear of childbirth, the decision to choose a cesarean section, and breastfeeding problems in subsequent pregnancies (9). Severe labor pain, inadequate response to analgesia during labor, instrumental delivery, elective cesarean section, fear of injury and death, loss of self-control, and feelings of powerlessness and helplessness during the stages of childbirth are among the consequences of traumatic childbirth in women (10).
Several studies have shown the effectiveness of different interventions in preventing or reducing stress during and after pregnancy, including social support, indirect counseling and debriefing, individual counseling by midwives, and cognitive-behavioral counseling (11-13). Cognitive-behavioral counseling has attracted more attention to different types of counseling. The cognitive-behavioral approach is based on the fundamental assumption that people’s interpretation of an event determines the way they feel and behave. In this method, the main emphasis is on changing attitudes to change behavior (14, 15). In this therapeutic approach, the client is helped to identify distorted patterns and dysfunctional behavior. In this regard, Abdollahpour et al. (11) showed that cognitive-behavioral counseling is effective in preventing and reducing the symptoms of post-traumatic stress disorder (PTSD), and especially in a long time affects unwanted thoughts. Psychological education had a positive effect on the anxiety of mothers with a history of stillbirth and significantly reduced their anxiety score (16). Other studies conducted by San Lazaro Campillo et al. (17), Gokce Isbir et al. (18), Asadzadeh et al. (19) also reported the effectiveness of midwifery counseling and prenatal training in reducing stress, anxiety, depression, and symptoms of PTSD.
Based on the common belief in each society, childbirth is considered a positive experience. The complications and symptoms of post-traumatic stress due to traumatic childbirth have long been remained unknown to many professionals, and they have not been considered seriously. Due to the high prevalence of traumatic childbirths from a women’s perspective, most previous studies have focused on the prevalence, clinical consequences, risk factors, and predictor variables, and less attention has been paid to interventional studies, especially pregnancies after experiencing traumatic childbirth. Pregnancy is a stressful and critical period that due to trauma and negative experience in previous pregnancies and deliveries, it has more psychosocial dimensions and negative clinical consequences for the mother, fetus, and delivery during pregnancy and even after childbirth. Thus, it is necessary to design and implement interventions with a psychological approach to reduce stress, especially the symptoms of post-traumatic stress, to increase the mental health of the mother during pregnancy and after childbirth to facilitate the childbirth process, and consequently provide the health and development of infants. Hence, the aim of this study was to evaluate the effect of cognitive-behavioral therapy (CBT) on the severity of post-traumatic stress symptoms in pregnant women with a history of traumatic childbirth.
2. Objectives
The current study was done to determine the effect of CBT on PTSD in pregnant women with a history of traumatic childbirth.
3. Methods
This study was a quasi-experimental intervention with a pretest-posttest design. The study population included pregnant women with a history of traumatic childbirth, referring to Comprehensive Health centers in Zahedan in 2020. The sample size was estimated to be 24 people in each group based on the mean and standard deviation of the post-traumatic stress score in the study conducted by Gokce Isbir et al. (18) with a 95% confidence interval and 95% statistical test power using the following formula. To ensure the sample size and to consider the possibility of dropout in samples in each group, 40 people and a total of 80 people were determined for each group.
Z1-α/2 = 1.96; S1 =7/8;
Inclusion criteria of the study included being married, the age of between 18 and 35 years, gestational age of 22 - 26 weeks, having the skill of reading and writing, no history of infertility before the current pregnancy, lack of known medical diseases, lack of a known mental disorder, no addiction or taking drugs, no hospitalization history in the current pregnancy, single pregnancy, having a healthy fetus, and the lack of stressful events during the 6 months before the start of the study. Also, the exclusion criteria of the study included the absence of more than one session in training sessions, the experience of major stress during the intervention, and the death of the fetus during the research.
Data were collected using questionnaires. The first scale assessed personal information, such as age, job, education, ethnicity, and type of pregnancy. The second scale was the PTSD questionnaire. It is a 20-item self-report tool that matches with the diagnostic criteria for PTSD in the DSM-V (16). This tool includes four subscales that exactly match the four symptoms of the disorder in DSM-V. Respondents can give their answers to each item on a five-point scale, ranging from zero (no complications) to 4 (severe complications) (the total score ranges from 0 to 80). PCL-5 consists of four subscales of intrusion, avoidance, negative mood changes, and hyper-arousal, which are placed on clusters of PTSD symptoms in the DSM-V. The Cronbach’s alpha for the English version of this tool was 0.95. Convergent validity for the English version of this scale was 0.89 (20). In the study conducted by Varmaghani et al. (21), Cronbach’s alpha coefficient for the whole scale was 0.92. In the present study, the reliability for the whole questionnaire was 0.82 using Cronbach’s alpha.
Traumatic Delivery questionnaire was developed based on the definition of criterion A of PTSD (DSM-V) of a traumatic event and consists of four items. The first two items examine threats, and the next two items assess the mother’s emotional response. If one case in any of the two questions is positive, childbirth is considered traumatic. Asking questions about the characteristics of a traumatic event in accordance with the DSM for screening traumatic childbirth has also been performed in the study conducted by Gamble et al. (12). The validity of the items was confirmed by a group of psychiatrists in Taghizadeh and Abdollahpour’s study, and the scale has been used in many studies (11-24).
After obtaining permission from the Ethics Committee of the University and receiving an official letter of introduction from the Deputy of Health Department, the researcher attended the Zahedan Health Center and the Comprehensive Health centers of Zahedan. First, among the pregnant women who attended to receive prenatal care, those who had a history of traumatic childbirth in previous pregnancies were identified using the Traumatic Delivery questionnaire and were selected using a convenience method. After obtaining informed written consent to participate in the study, the pre-test was implemented by completing the PTSD Questionnaire. The samples were divided into two groups of intervention and control using random allocation. Specifications, telephone numbers, and addresses were obtained from the control group members to collect post-test information at home or at the clinic. The intervention group members were also contacted and coordinated in terms of the time of holding the classes. Based on the number of samples and due to the coronavirus crisis, educational sessions were held in accordance with health protocols. Hence, the number of pregnant women participating in each educational class varied from 1 to 3 cases. The women in the intervention group received four sessions of CBT for four weeks, based on the content specified in Table 1. In the fifth week, the research questionnaires were completed again as a post-test, by referring to the participants’ homes or the centers. During this period, the control group did not receive any educational program and only received routine pregnancy care. To observe the ethical issues after the intervention, the educational content was provided to the control group.
| Session | Educational Content of the Sessions |
|---|---|
| Session 1 | Introduction, familiarizing, group rules, psychological dimensions of pregnancy following traumatic childbirth, stating individual experience of pregnancy after traumatic childbirth, design of fears and worries related to traumatic childbirth, the impact of previous unpleasant experience on pregnancy and current childbirth, normal pregnancy physiology, the natural process of childbirth and reassurance. |
| Session 2 | Coping strategies in traumatic postpartum pregnancy, teaching the concept of avoidance and the skill of real and gradual exposure, training in muscle relaxation to reduce the symptoms of fear and arousal, imaging and breathing exercises. |
| Session 3 | Identifying the cycle of thought-emotion-behaviors, explaining and practicing the ABCD model, identifying automatic thoughts about pregnancy and childbirth, common mental errors in childbirth and pregnancy, especially after traumatic childbirth, and correcting and changing these errors. |
| Session 4 | Identifying and teaching techniques for tracking common mental images during pregnancy until they are complete, deliberately remembering and narrating of the experience of traumatic childbirth, facilitating and practicing cognitive processing and conscious and intentional rumination, expressing emotions in a safe and protected environment, and normalizing emotional reactions in pregnancy following a traumatic childbirth. |
To prepare the content of the CBT package, after studying books, articles, and information sources adapted from the studies of Abdollahpour et al. (11), Asadzadeh et al. (19), Gokce Isbir et al. (18), and Gamble et al. (12), the initial structure of the intervention was designed and prepared. Then, the experts in clinical psychology, counseling, obstetrics, and midwifery education were surveyed. The CBT was presented by a master’s degree student in midwifery counseling with clinical experience, under the supervision of a person with a PhD in counseling.
Data were collected, coded, and analyzed using SPSS 22 software. The Shapiro-Wilk test was used to evaluate the normality of data. First, frequency, percentage, mean, and standard deviation were determined using descriptive statistics. Also, to compare the pre-test and post-test means in each group, the paired t-test was used. The independent t-test and chi-square test were used to compare the frequencies of qualitative variables of two groups. The significance level in this study was considered at 0.05.
4. Results
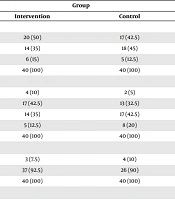
Independent t-test showed that the two groups were not significantly different in terms of mean age, the time interval between current pregnancy and last delivery, number of pregnancies, mean age of marriage, number of live children, and wanted or unwanted pregnancy. Also, Fisher’s exact test was used to examine two groups in terms of frequency of addiction, history of cesarean section in previous deliveries, pregnancy and delivery complications, and history of stillbirth, and employment status of the spouses and the results showed that there was no significant difference between the two groups (P < 0.05). Also, the differences in educational status, history of abortion, and sex of the fetus in the two groups were no significant (P < 0.05) (Table 2).
| Variable | Group | Test Result | |
|---|---|---|---|
| Intervention | Control | ||
| Education | 0.65b | ||
| Under diploma | 20 (50) | 17 (42.5) | |
| diploma | 14 (35) | 18 (45) | |
| Higher than diploma | 6 (15) | 5 (12.5) | |
| Total | 40 (100) | 40 (100) | |
| Spouse’s educational | 0.55c | ||
| Illiterate | 4 (10) | 2 (5) | |
| Under diploma | 17 (42.5) | 13 (32.5) | |
| diploma | 14 (35) | 17 (42.5) | |
| Higher than diploma | 5 (12.5) | 8 (20) | |
| Total | 40 (100) | 40 (100) | |
| Spouse’s job | 0.99d | ||
| Non-employed | 3 (7.5) | 4 (10) | |
| Employed | 37 (92.5) | 26 (90) | |
| Total | 40 (100) | 40 (100) | |
| Pregnancy type | 0.77b | ||
| Unwanted | 7 (17.5) | 8 (20) | |
| Wanted | 33 (82.5) | 32 (80) | |
| Total | 40 (100) | 40 (100) | |
| Caesarian section history | 0.99d | ||
| Yes | 3 (7.5) | 4 (10) | |
| No | 37 (92.5) | 36 (90) | |
| Total | 40 (100) | 40 (100) | |
| Type of last delivery | 0.87c | ||
| Vaginal delivery with rupture | 23 (57.5) | 25 (62.5) | |
| Vaginal delivery without rupture | 14 (35) | 13 (32.5) | |
| Caesarian section | 3 (7.5) | 2 (5) | |
| Total | 40 (100) | 40 (100) | |
| History of stillbirth | 0.67d | ||
| Yes | 2 (5) | 4 (10) | |
| No | 38 (95) | 36 (90) | |
| Total | 40 (100) | 40 (100) | |
| Fetus sex | 0.66c | ||
| Male | 24 (60) | 21 (52.5) | |
| Female | 13 (32.5) | 17 (42.5) | |
| Unknown | 3 (7.5) | 2 (5) | |
| Total | 40 (100) | 40 (100) | |
| History of abortion | 0.59b | ||
| Yes | 8 (20) | 10 (25) | |
| No | 32 (80) | 30 (75) | |
| Total | 40 (100) | 40 (100) | |
| Age, y | 27.73 ± 5.14 | 28.55 ± 4.89 | 0.46e |
| Gestational age | 23.28 ± 1.26 | 23.20 ± 1.3 | 0.79e |
| Number of pregnancies | 3.00 ± 1.26 | 3.10 ± 1.17 | 0.71e |
| Interval pregnancy | 4.17 ± 2.42 | 4.22 ± 2.45 | 0.92e |
aValues are expressed as mean ± SD or No. (%).
bChi-square.
cMonte Carlo.
dFisher exact test.
eIndependent t-test.
According to Table 3, the mean score of post-traumatic stress severity in pregnant women with a history of traumatic childbirth in the intervention group (15.25 ± 4.08) was significantly lower compared with the control group (26.25 ± 11.56) after the intervention. The paired t-test showed that this change before and after the intervention was significant in the intervention group (p = 0.001) and non-significant in the control group (P = 0.07). Also, the mean changes in the post-traumatic stress score of pregnant women in the intervention group (-12.65 ± 10.96) were significantly higher compared with the control group (1.05 ± 4.20) (P = 0.0001).
| Group | Time | Changes | Paired t-test | |
|---|---|---|---|---|
| Before Intervention | After Interventions | |||
| Intervention | 27.90 ± 10.91 | 15.25 ± 4.08 | 12.65 ± 10.96 | 0.0001 |
| Control | 24.97 ± 14.85 | 26.25 ± 11.56 | 1.05 ± 4.20 | 0.07 |
| Independent t-test | P = 0.31 | P = 0.001 | P = 0.0001 | |
aValues are expressed as mean ± SD.
5. Discussion
Given the high rate of f traumatic childbirth, and subsequently PTSD in Iran and the positive effects of CBT, the present study aimed at investigating the effect of CBT on the severity of post-traumatic stress symptoms in pregnant women with a history of traumatic childbirth. The research results showed that the mean score of severity of PTSD in pregnant women with a history of traumatic childbirth after CBT in the intervention group was significantly lower compared with the control group.
Studies have been conducted on the role of counseling as a solution to reduce mood and mental disorders during pregnancy or after childbirth. The results of the study conducted by Andaroon et al. (25) showed that three sessions of individual counseling by midwives using the Gamble et al. (12) strategy in pregnancy can reduce anxiety during pregnancy and the level of reduction of anxiety in the intervention group compared with the control group was statistically significant. The results of the mentioned study are consistent with those of the present study. In the present study, CBT during pregnancy could reduce the mean score of post-traumatic stress of pregnant women. Wienereb et al. (26) also showed in his study that psychosocial education during pregnancy is effective in reducing the symptoms of PTSD, which is consistent with the results of our study. In his study, women were screened in terms of PTSD before the study, but in our study, the women were not screened (26). Seyed Kaboli et al. (27) conducted a randomized clinical trial to investigate the effect of group counseling based on CBT on pregnancy-specific anxiety and stress in 62 pregnant women in Karaj. The results of the study showed that CBT-based counseling reduced maternal stress and anxiety in the intervention group. However, the mean scores of stress and anxiety between the two groups were statistically significant (27). Their results are also consistent with those of the present study; however, the content and approach of counseling and the counseling method in their research were different from those of the present study. Khanzadeh et al. (28) also obtained results in line with those of the present study.
The difference between the present study and the mentioned studies is that we used CBT to prevent PTSD for mothers who were expected to be at higher risk of PTSD compared with other mothers.
Another study in line with the present study was the research conducted by Abdollahpour et al. (11), who showed that cognitive-behavioral counseling improved post-traumatic stress symptoms. Azizi et al. (24) also examined the effect of midwifery counseling interventions on the rate of traumatic postpartum anxiety in nulliparous women and concluded that midwifery counseling reduces the rate of traumatic postpartum anxiety in women. Ayers et al. (29) also showed that cognitive-behavioral counseling could reduce PTSD. The results of these studies are consistent with those of the present study. Although in these studies, counseling was performed shortly after experiencing traumatic childbirth, in the present study, counseling was provided before childbirth; thus, it can be concluded that this counseling is preventive.
In contrast to the results of the present study, Gamble et al. (12) and Taghizadeh et al. (22) in their study on women with traumatic childbirth concluded that postpartum counseling could not make a statistically significant difference between the two groups 4 - 6 weeks after childbirth. However, at follow-up, three months after childbirth, women in the intervention group had less severe PTSD than the women in the control group. The results of their study are not consistent with those of the present study, because the present study could make a statistically significant difference between the two groups in the short term. The results of a study conducted by Ryding et al. (30) also showed that group counseling had no effect on the level of fear and symptoms of PTSD and depression in women 6 months after delivery, which is inconsistent with the results of the present study. The reason might be the difference in the number of therapy sessions and counseling time and method. Rouhe et al. (31) also showed that psychological education during pregnancy had no effect on symptoms of PTSD.
In general, it can be concluded that CBT is effective in reducing the symptoms of PTSD. Providing information using group sessions made mothers have a more positive evaluation of pregnancy and childbirth, and finally, less stress, which in turn reduces the number of traumatic childbirths and PTSD.
Also, providing group training classes and free interactions between the members make mothers enjoy each other's experiences, knowledge, and support. Talking freely in a homogeneous group leads to the emotional catharsis of pregnant women with a history of traumatic childbirth because, for most of these women, it is difficult to talk about childbirth. Accordingly, talking with other people who have a similar problem provides a unique opportunity for pregnant women to get a more realistic picture of their situation through direct interaction with each other. Complex emotional interactions in the group provide an opportunity to model successful behaviors. It also allows pregnant mothers to help each other realize their worth, usefulness, and uniqueness and experience a better feeling. Such a situation will give mothers self-confidence that enables them to cope better with the new experience of childbirth. Since traumatic childbirth puts mothers at a potential psychological risk during pregnancy and the postpartum period, this issue should be considered by health professionals, especially midwives, to screen all women in terms of predisposing factors and mental problems immediately at the first prenatal visit, and should take the necessary measures for prevention and treatment, and if necessary, refer them for specialized psychiatric centers.
This study faced some limitations. These limitations include the lack of a support system in the CBT program. Also, the intervention did not start in the first weeks of pregnancy and did not continue for a longer period during pregnancy and the postpartum period.
5.1. Conclusions
The results of the present study showed that the CBT had a positive and significant effect on reducing the mean score of PTSD symptoms in pregnant women with a history of a traumatic delivery. However, an active approach to prevent or treat PTSD symptoms at an early stage can also lead to fewer or less severe cases of PTSD. Screening women who are at high risk of developing PTSD following childbirth is effective in increasing the efficacy of preventative interventions. Considering the high prevalence of PTSD following childbirth in Iran, it is recommended to consider a screening program and include this type of educational intervention in the care program of pregnant women with a history of a traumatic delivery.