1. Background
Novel improvements in the pathophysiology of pain have expressed that it is conceivable to exclude or reduce the central neural hyperexcitability that contributes to increased postoperative pain (1). Pregabalin is a constructive abduction of γ-aminobutyric acid, which displays analgesic, anticonvulsant, and anxiolytic effects. This drug is approved for neuropathic pain treatment in many countries (2).
Postoperative pain is a common and noticeable complication that causes analgesic use in about half of patients (3). Pain increases stress hormones, impairs hemodynamics by increasing respiration, blood pressure, and heart rate, and ultimately prolongs the hospitalization duration and healing process (4). Pain is the most common complication of the first night after elective laparoscopic cholecystectomy (4). Different methods are used to reduce pain, one of which is pain-reducing drugs (4). Pregabalin is an evolved form of gabapentin. This medication group regulates the entry and exit of calcium into the cell through the calcium channels. Pregabalin prevents the release of glutamate, the primary neurotransmitter involved in the pain transmission signal, thereby controlling seizures resistant to treatment and neuroleptic pain.
Pregabalin is used as a pain reliever after breast and spine surgeries and laparoscopy (5). Studies have demonstrated that 35 - 63% of patients have moderate abdominal and shoulder pain in the first 24 to 48 hours after surgery (6). Pregabalin is also used as an anxiolytic (7). For the characterization of whether a single preoperative accomplishment of two various doses of pregabalin (i.e., 75 and 150 mg) can reduce postoperative pain severity and opioid use following posterior lumbar interbody fusion surgery (8).
In most studies, gabapentin has been used after surgery. Various studies have been conducted on 75 - 600 mg of pregabalin before surgery for subsequent analgesia. The critical point is that the probability of side effects, including edema, dizziness, and nausea, increases with increasing doses. There is still no consensus on the minimum effective dose of pregabalin for postoperative analgesia. The present study assessed the analgesic effects of two different doses of pregabalin (i.e., 150 and 75 mg) 1 hour before the lumbar disc herniation surgery on postoperative pain.
2. Objectives
This study also evaluated the need for postoperative morphine to obtain the least effective dose of this drug, which is associated with reducing complications.
3. Methods
This clinical trial study was performed with a registration number (IRCT2017030132832n1) and based on a permit from the Ethics Committee of Zahedan University of Medical Sciences, Zahedan, Iran (ethics code: IR.ZAUMS.REC.1395.16). The current study was performed on 90 candidates for elective herniated disc surgery aged 20 - 60 years in Khatam Al-Anbia Hospital of Zahedan in 1395. The patients were included based on the American Society of Anesthesiologists I-II. The exclusion criteria were kidney and liver function disorders, a history of using alcohol or any drug, a history of uncontrolled internal diseases (e.g., diabetes and high blood pressure), a history of using nonsteroidal anti-inflammatory drugs 24 hours before the surgery, and the urgency of surgery.
After collecting patients’ demographics, the patients were randomly assigned to three groups, including high dose pregabalin (150 mg), low dose pregabalin (75 mg), and placebo. The method of randomized blocking used 10 nine-member blocks, each of which consisted of 3 patients from each group. Each member of the group was placed in the block based on the permutation state. One hour before the surgery, the placebo group received an oral capsule containing starch, the second group was given pregabalin (Lyrica) orally at a dose of 75 mg, and the third group received pregabalin (Lyrica) at a dose of 150 mg by a nurse unaware of the administrated drug. One surgeon operated on all the surgeries, and the duration of surgery was 3 hours. The induction of anesthesia was performed in all groups in a traditional manner.
Fentanyl was injected at a dose of 2 μg/kg body weight as an anesthetic drug. Anesthesia induction was performed with propofol at a dose of 2.5 mg/kg body weight. CisAtracurium was used as a muscle relaxant at a dose of 0.15 mg/kg body weight. Propofol was given as an anesthetic preservative with a dose of 200 μg/hour/kg body weight. All the patients were intubated with an appropriate trachea tube.
During the surgery, the patients were monitored for continuous heartbeat, continuous hemoglobin saturation, continuous exhaled carbon dioxide, and average blood pressure every 3 minutes. All the measurements were performed using a Siemens device (Germany). At the end of the surgery, neostigmine and atropine were used to antagonize muscle relaxant effects. Finally, the trachea tubes were removed, and the patients were transferred to the recovery.
After complete vigilance, the patient’s pain was evaluated using a 100-point visual assessment, in which 0 and 100 indicate no pain and unbearable pain, respectively. The nurse measured the pain 2 hours after the surgery and 4, 8, 12, and 24 hours later. Additionally, the nurse was informed about the study but had no information about the administrated drug. After entering the recovery, the morphine pump was inserted intravenously to control the pain, and if the grade of pain was higher than 4, the patients received 2 mg/hour of morphine for up to 12 mg per 4 hours of infusion. Confounding variables, including gender, age, and weight, were matched, and if they were not homogeneous, their effect was eliminated by appropriate statistical methods.
4. Results
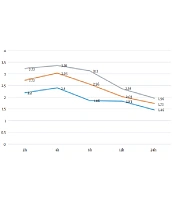
In this study, the analysis of variance with repeated measures demonstrated that the changes in pain score over time were significant, and a decreasing trend was observed in all the three groups over time (P < 0.001; Tables 1 and 2). On the other hand, the mean postoperative pain scores in the three groups were significantly different (P < 0.001; Tables 1 and 2). However, considering that the interaction between time and group was not significant (P = 0.33; Tables 1 and 2), it can be said that the pattern of pain score changes in the three groups studied over time was not significantly different (Figure 1). High and low doses of pregabalin and placebo did not have a different effect on reducing patients’ pain after the surgery. Therefore, intragroup and intergroup comparisons were not possible.
| Group or Time | Placebo | Pregabalin (75 mg) | Pregabalin (150 mg) |
|---|---|---|---|
| 2 h | 3.23 ± 1.73 | 2.73 ± 1.63 | 2.20 ± 1.54 |
| 4 h | 3.36 ± 1.32 | 3.03 ± 1.21 | 2.40 ± 1.37 |
| 8 h | 3.13 ± 1.13 | 2.56 ± 1.00 | 1.86 ± 0.77 |
| 12 h | 2.36 ± 0.71 | 2.03 ± 0.80 | 1.83 ± 0.83 |
| 24 h | 1.96 ± 0.85 | 1.73 ± 0.63 | 1.46 ± 0.62 |
a Values are expressed as mean ± SD.
| Source of Change | Sum of Squares | Degrees of Freedom | Mean | Test Statistics | Significance Level |
|---|---|---|---|---|---|
| Time | 73.38 | 1 | 73.38 | 47.20 | 0.001 |
| Group | 55.60 | 2 | 27.80 | 14.46 | 0.001 |
| Time and group interaction | 3.46 | 2 | 1.73 | 1.11 | 0.33 |
| Error | 167.18 | 87 | 1.92 |
5. Discussion
The present study demonstrated that the changes in pain scores over time were significant, and all three groups had a decreasing trend over time (P < 0.001). On the other hand, the mean pain scores in the three groups were significantly different (P < 0.001). However, considering that the interaction between time and group was not significant (P = 0.33), it can be said that the pattern of pain score changes in the three groups studied over time was not significantly different.
High and low doses of pregabalin and placebo did not have a different effect on reducing patients’ pain after surgery. In patients receiving 150 mg pregabalin, the mean postoperative pain was less than 75 mg pregabalin group. The pain level in both groups of pregabalin was significantly lower than in the placebo group. Therefore, the need for analgesics was also lower than that of placebo-treated patients. However, there was no significant difference in the incidence of complications.
Jiang et al. (2017) investigated the reducing effect of pregabalin on postoperative complications. They demonstrated that a high dose of pregabalin (< 300 mg/daily) could reduce the visual analog scale score significantly within 48 hours. Low- and high-dose pregabalin can reduce morphine consumption and complications, such as nausea, dizziness, headache, and visual impairment in the first 48 hours (9).
Furthermore, Ozgencil et al. (2011) evaluated the pain after lumbar disc surgery that was less in patients receiving pregabalin than those in the placebo group (10). Nevertheless, in a study conducted by Zarei et al. in 2016, postoperative pain in the lumbar region in patients receiving pregabalin was not significantly different from that of the placebo group, which is not consistent with the results of the present study. This discrepancy might be due to differences in the study methods; accordingly, the study by Zarei et al. continued for 2 weeks after the surgery, and patients were monitored for postoperative pain (11).
The effect of pregabalin on postoperative pain in other surgeries was also shown in a study by Li et al. in 2017 that examined the effect of pregabalin on acute pain and morphine need in patients undergoing laparoscopic cholecystectomy. Li et al. demonstrated that pregabalin was effective in reducing postoperative pain, morphine need, and morphine complications after laparoscopic cholecystectomy. In addition, high doses of pregabalin were more effective than low doses (12).
In 2008, Agarwal et al. conducted a study on patients undergoing laparoscopic cholecystectomy. They stated that the levels of postoperative pain and the need for fentanyl were significantly lower in the group receiving pregabalin compared to those reported for the placebo group (3). Similarly, Sarakatsianou et al. (2013) showed that the levels of postoperative pain after laparoscopic cholecystectomy and the need for morphine in the group receiving oral pregabalin were significantly lower, compared to those reported for the placebo group (4). However, in a meta-analysis performed by Mishriky et al. in 2015 on 55 studies on the effect of pregabalin on postoperative pain reduction in all doses (i.e., < 75, 100 - 150, and 300 mg), no significant difference was observed in the number of doses of analgesics or the reduction of postoperative pain, both in single-dose administration of pregabalin and the use of multiple doses. However, the data showed improved postoperative pain relief in pregabalin use, compared to that reported for placebo (13).
In addition, a study performed by Emadi et al. in 2015 evaluated the effect of a single dose and a low dose of pregabalin on pain control after abdominal hysterectomy. The difference in pain intensity between the groups was not statistically significant; nevertheless, the time to receive analgesic in the placebo group was less than pregabalin. However, the use of pregabalin in low doses did not affect the control of pain after abdominal hysterectomy (14). Another study was carried out by Eftekharian et al. in 2014 on 210 patients with impacted wisdom teeth on the effect of oral pregabalin on blood pressure after surgery. Eftekharian et al. showed that 75 mg of pregabalin significantly reduced systolic and diastolic pressures and was also effective in reducing postoperative pain scores (15). The limitation of the present study is the use of low-dose drugs. Therefore, it is suggested to perform further studies in this regard.
5.1. Conclusion
The present study showed that pregabalin significantly reduces postoperative pain and the required dose of analgesia. On the other hand, pregabalin complications are minor and can be neglected.