1. Background
Caused by a new type of coronavirus, COVID-19 often targets the respiratory system and is associated with mild pulmonary symptoms (such as cough and dyspnea) but with pneumonia and hospitalization in the intensive care unit in severe cases. Sometimes, the disease symptoms are digestive disorders, lack of sense of smell and taste, lethargy, and premature fatigue. The early prevalence of this disease was reported as a severe acute respiratory syndrome (CoV-SARS) and Middle East respiratory syndrome (CoV-MERS) with severe lower respiratory tract infection in humans (1). According to WHO, the latest confirmed COVID-19 cases were 260,079,122 persons, of whom 5,196,842 died. The COVID-19 incidence and mortality in Iran were 6,097,672 and 129,376, respectively (2). Initially, the mortality rate of COVID-19 patients was reported to be 3 to 5%, but recent reports indicate an increase up to 9% (3).
One of the most common problems in COVID-19 patients is fatigue and body aches (4), defined as a nursing diagnosis, with a feeling of weakness and reduced capacity to perform mental and physical activities (5). One study showed that two months after the incidence of COVID-19 in patients with a history of hospitalization, while none of them had a fever or signs of disease activity, half of them still complained of fatigue, and about 44% claimed the decreased quality of life (6). Chronic viral infection in the lungs, brain, and other tissues may be one of the mechanisms associated with fatigue. This is due to the increase in the basal level of two molecules, interleukin-6 (IL-6) and interleukin-10 (IL-10), which cause inflammation in the body and are predictors of chronic fatigue (7). An increase in these molecules is seen in patients with severe COVID-19 (3). In addition to fatigue and body aches, the most common symptom seen in COVID-19 patients is dyspnea. The patient becomes prematurely tired as the disease progresses, even with simple life activities. Fatigued people do not have their previous energy. Thus, they do less activity and try harder to minimize activities of daily living, so this will affect their quality of life and self-confidence (5). Woo showed that three indices of dyspnea, fatigue, and physical activity are interrelated, so higher fatigue and lower physical activity were reported in chronic obstructive pulmonary disease (COPD) patients (8).
A review study by Soleimanifar and Hazrati showed that according to the 2020 physiotherapy guidelines for COVID-19 patients, cardiopulmonary physiotherapy is focused on the treatment and rehabilitation of acute and chronic respiratory conditions that can have an influential role in respiratory therapy and physical rehabilitation of the patients (9-12). Pulmonary rehabilitation uses a mixed multidimensional approach that includes training and breathing exercises to influence activity levels, symptoms, and complaints in patients with respiratory problems, intending to create maximum patient performance independence. One of the rehabilitation approaches is home-based rehabilitation, with the active involvement of the patient and his/her family in identifying needs and training (13). Given that the focus of medical policies is currently on speeding up the patient's discharge from the hospital, reducing the stay length of the patient in medical centers and receiving care in the community and home-based health services as a care solution have received more attention, with features such as ease of access, low cost, client acceptance, and family involvement (14).
A literature review shows that no study has yet addressed the impact of pulmonary rehabilitation intervention in patients with COVID-19 respiratory symptoms. However, two review studies on the effect of pulmonary rehabilitation and physiotherapy management of respiratory systems in COVID-19 patients concluded that physiotherapy could play an influential role in respiratory and physical rehabilitation of the patients, and pursed-lip breathing exercise, diaphragmatic breathing, local dilation of the lungs, and chest volume exercises were the most important ways to improve respiratory function of COPD patients including COVID-19 patients (12, 15). Other researchers (Wang et al., Talman et al., Polastri et al., Demeco et al.) reviewed previous studies and recommended pulmonary rehabilitation as supportive care that could improve the respiratory function of patients with respiratory problems, especially patients with COVID-19 respiratory infection (16-19). Liu et al. also found that six-week respiratory rehabilitation was effective in respiratory function, lung capacity, and activities of daily living of older adults with COVID-19 (20).
Given that COVID-19 is a newly emerged disease, there are a few scientific and documented findings on the effectiveness of rehabilitation interventions on fatigue, respiratory indicators, and activities of daily living of the patients. One of the most important organs involved in COVID-19 is the respiratory system. Moreover, fatigue and acute dyspnea adversely affect COVID-19 patients’ activities of daily living. Thus, these patients need long-term breathing exercises to speed up patient recovery after hospital discharge. Accordingly, raising COVID-19 patients' awareness of effective pulmonary rehabilitation techniques seems to be effective in reducing the patient's respiratory problems (cough ‚dyspnea‚ and fatigue) and improving the function of this vital system during hospitalization and home quarantine (15).
2. Objectives
The present study aimed to examine the effect of home-based rehabilitation on fatigue, dyspnea, and activities of daily living of COVID-19 patients in teaching hospitals of Zahedan University of Medical Sciences in 2020.
3. Methods
This study was conducted using a quasi-experimental design with two groups. The study protocol was approved with the ethics code IR.ZAUMS.REC.1399.498 by the Ethics Committee of Zahedan University of Medical Sciences. The participants were COVID-19 patients admitted to the COVID-19 intensive care units of teaching hospitals in Zahedan, southeastern Iran, in 2020. The inclusion criteria were confirmed COVID-19, CT scan of the lung with minimal involvement, patient’s stable condition, no restrictions to participate in the pulmonary rehabilitation program according to the physician’s recommendation, age of 18 to 60 years, no chronic lung disease, no underlying disease (ischemic heart disease, congestive heart failure, uncontrolled high blood pressure, diabetes‚ cancer, and acute and chronic kidney disease), ability to communicate and speak in Persian, and residing in Zahedan. The exclusion criteria were exacerbating the disease and respiratory symptoms during the study, not participating in more than one training session, not performing the recommended rehabilitation program, leaving the study, and receiving care other than routine hospital care. The patients who met the inclusion criteria were selected using convenience sampling and randomly divided into intervention and control groups by drawing red and white cards (red cards for the intervention group and white cards for the control group). The sample size was estimated at 24.5 persons based on the mean and standard deviation of the fatigue score reported by Heidari et al. (21) with 95% confidence and 85% test power using the following formula:
However, taking a 20% dropout, a total of 60 patients (30 persons per group) were selected to participate in the study (21). The instruments used to collect data were a demographic information form (age, sex, marital status, education, occupation, ethnicity, and smoking), a self-report checklist for breathing exercises at home, the Fatigue Severity Scale (FSS), the Borg Dyspnea Scale, and the Barthel Index to measure activities of daily living.
The Fatigue Severity Scale (FSS) is a valid self-report tool developed by Krupp et al. to measure fatigue severity. This scale consists of nine statements, each scored 1 to 7 according to the severity of symptoms. In addition, five items measure the quality of fatigue, three items measure physical and mental fatigue and the effects of fatigue on a person's social status, and one item measures the severity of fatigue with other symptoms in the person. Each item is scored 0 to 7 (0 = strongly disagree to 7 = strongly agree). The total scale score is calculated as the sum of the scores for individual items. The higher the score, the more severe the fatigue in the respondent (22). The reliability of the instrument was measured using the test-retest method as 0.93, 0.91, and 0.78 by Zakeri Moghadam et al., Jokar et al., and Shahvaroughi Farahani et al., respectively (5, 9, 23). In this study, the instrument's reliability was estimated to be 0.81 using Cronbach's alpha.
3.1. Borg Dyspnea Scale
This scale is a standard numerical measure in which each number is associated with an attribute that describes respiratory status. Its reliability was reported to be 0.78 in the literature. Each number in this scale represents a description of the respiratory status, and each number is scored 0 to 10, with a score of 0 indicating the absence of dyspnea and a score of 10 indicating the maximum level of dyspnea (24). The reliability of this instrument was measured in this study as 0.75 using Cronbach’s alpha.
The Barthel Index was developed by Dorothy Barthel and Mahoney Florence in 1965 in the United States to measure the extent to which one can function independently and have mobility in their activities of daily living (ADL). The Barthel Index contains 10 items scored on a 0 - 15 Likert scale. The total score varies from 0 to 100. A score of 100 indicates complete independence, and a score of 0 indicates complete dependence of the person in activities of daily living. The items deal with activities such as feeding (0 - 10), bathing (0 - 5), personal toileting (0 - 5), dressing and undressing (0 - 10), controlling bladder (0 - 10), controlling bowel (0 - 10), getting on and off a toilet (0 - 10), moving from wheelchair to bed and returning (0 - 15), walking on a level surface (0 - 15)‚ and ascending and descending stairs (0 - 10) (24). Generally, this tool measures the individual's ability in different dimensions of daily performance on a scale of 0 - 100, and a higher score indicates a higher level of independence in performing activities of daily living (25). Psychometric properties of the short form of the Barthel Index were assessed by Tagharrobi and Sooky (26), and its internal consistency was reported to vary from 0.83 to 0.93. Jokar et al. reported the reliability index of the tool as 0.83 (9). In this study, the instrument's reliability was calculated to be 0.79 using Cronbach's alpha.
After obtaining the required permits to conduct the research project, the researcher referred to the COVID-19 intensive care units of Zahedan teaching hospitals. She explained the study's objectives and the research procedures and invited the patients to participate in the study if they were willing. After selecting the patients who met the inclusion criteria and assigning them to the intervention and control groups, the questionnaires were administered to the patients in both groups, and they completed the questionnaires' items. The pulmonary rehabilitation program was conducted individually for the patients in the intervention group in three 45-min face-to-face training sessions, using educational videos and training materials in full compliance with post-discharge health protocols according to the instructions provided by the National COVID-19 Control Center. After providing training on breathing exercises, the patients were asked to perform breathing exercises in the researcher's presence to ensure that they learned to perform the exercises correctly. At the end of the training sessions, an illustrated educational booklet prepared based on authoritative scientific texts under the supervision of experts in this field was given to each patient. Theoretical training included instructional materials related to the disease and home-based rehabilitation techniques (Table 1). After the discharge, the follow-up was conducted from the first week to the eighth week (once a week) using phone calls, and the patients were reminded to perform the breathing exercises. A self-report checklist for breathing exercises was also provided to the patient to mark the breathing exercises performed by them. Using the same checklist, the researcher monitored the patients' performance in telephone calls. Moreover, a contact number was provided to the patients to call the researcher if they had any questions or problems performing the exercises. The researcher also contacted the patients in the control group to ensure that they did not receive any training or intervention other than routine hospital care. To comply with ethical principles, we gave an educational booklet to each patient in the control group when completing the questionnaires on the posttest.
The Fatigue Severity Scale (FSS), the Borg Dyspnea Scale, and the Barthel Index were completed by the patients in the two groups two and eight weeks after completing the training sessions in the researcher's presence at the patient's home. After completing the questionnaires, all items were checked to ensure that the patients completed them. The collected data were entered in SPSS software (version 22), and their normality was checked using the Shapiro-Wilk test. The chi-square test was also run to compare the frequency of the qualitative variables between the two groups. The independent samples t-test was used to compare the mean scores for the research variables in the two intervention and control groups. Furthermore, a repeated measures analysis of variance (ANOVA) was run to compare the mean scores of the research variables before, two weeks, and two months after the intervention in the two groups. Assumptions such as the qualitative nature of the independent variable, equality of variances of the total scores, and the homogeneity of the variances were established. The intragroup and intergroup comparisons were made at a significance level of less than 0.05 (P < 0.05). Table 1 describes the content of the pulmonary rehabilitation training sessions.
| Sessions | Description |
|---|---|
| 1 | Stating the objectives of the study, presenting educational materials on the nature, symptoms, and complications of COVID-19, prognosis, supportive therapies, self-care, and training of pursed-lip breathing using educational videos and questions and answers to ensure the patients’ understood the materials and could respond to the questions |
| 2 | Reviewing the instruction provided in the previous session with the active participation of the patients, teaching diaphragmatic breathing and effective coughing using educational videos and their practice by the patient to ensure that they correctly performed the instructed techniques |
| 3 | Reviewing the instruction provided in the previous session with the active participation of the patients, encouraging the patients to take care-related challenges, teaching active respiratory cycle techniques using educational videos and an illustrated educational booklet containing practical and theoretical instructions presented during the sessions |
The Content of the Pulmonary Rehabilitation Training Sessions
4. Results
The results showed that 60% of the patients in the intervention group and 53.3% in the control group were employed. Moreover, 70% of the patients in the intervention group and 66.7% in the control group were Persians (an Iranian ethnic group that makes up over half the population of Iran). In addition, 83.3% and 66.7% of the control and intervention groups patients were married, respectively. The mean age of the patients in the intervention and control groups was 40.06 ± 10.54 and 41.33 ± 12.68 years, respectively. Moreover, the average educational years for the patients in the two groups were 9.53 ± 6.96 and 8.13 ± 6.57 years, respectively. There were no statistically significant differences between the two groups regarding demographic characteristics, including age, sex, marital status, education, occupation, ethnicity, and smoking habits (P < 0.05).
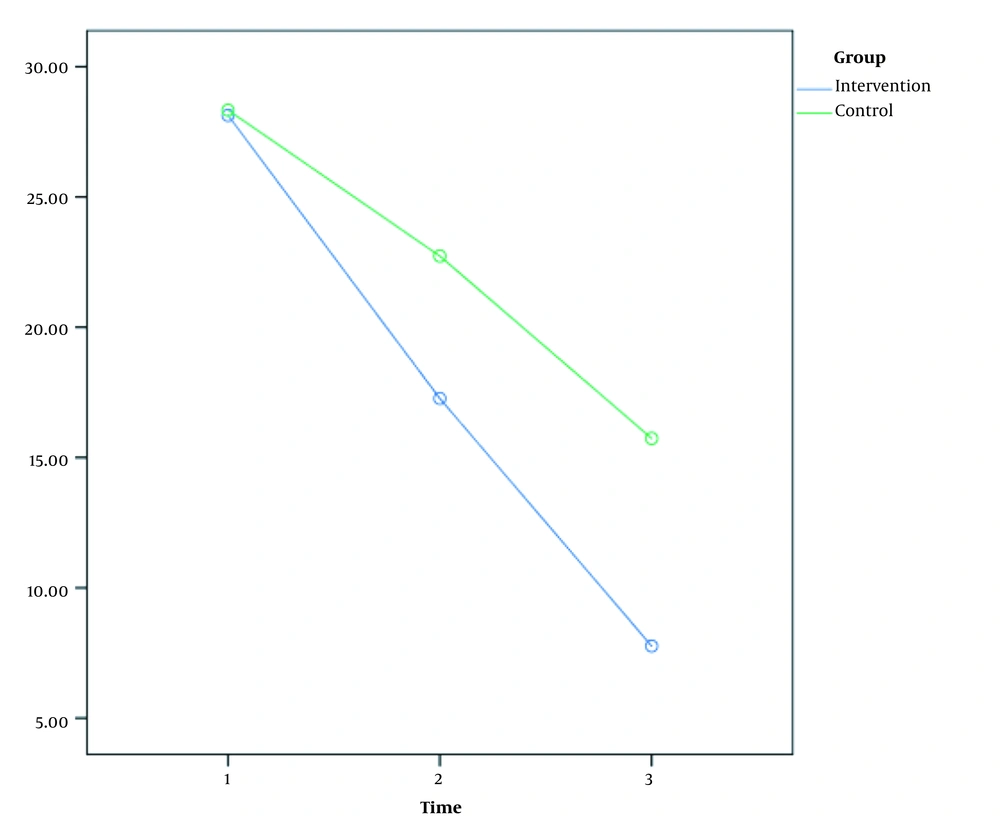
The mean fatigue scores for the participants in the intervention group before, two weeks, and two months after the intervention were 28.13 ± 12.78, 17.26 ± 9.50, and 7.76 ± 7.36, and the corresponding values in the control group were 28.33 ± 12.02, 27.33 ± 10.32, and 15.73 ± 8.61, respectively. The fatigue level in the intervention group significantly reduced two and eight weeks after pulmonary rehabilitation.
The repeated measures ANOVA (Figure 1) indicated that the changes in the fatigue scores over time were significant (P < 0.001), confirming a significant difference due to the effects of the intervention program (P = 0.04). In other words, the changes in the fatigue scores in the two groups were not the same, and the changes in the dyspnea score were more remarkable in the intervention group than in the control group. Given the significance of the group-time interactive effect, the comparisons were made point by point and with Bonferroni correction again by time and group. The results showed significant differences in the fatigue scores in the post-intervention (P = 0.03) and follow-up (P < 0.001) between the two groups. The comparison of the means of three measurements in each group showed that in the intervention group, the mean scores two weeks and two months after the intervention were significantly different from the pretest score (P < 0.001). In the control group, this difference was significant at these two points (P < 0.001) (Table 2).
| Variable | Sum of Squares | df | Mean Squares | F | P-Value |
|---|---|---|---|---|---|
| Time | 8151.008 | 1 | 8151.008 | 168.23 | 0.001 |
| Group | 929.339 | 1 | 929.339 | 3.53 | 0.04 |
| Group-time | 452.408 | 1 | 452.408 | 9.33 | 0.003 |
| Error | 15232.322 | 1 | 262.626 |
Results of Repeated Measures Analysis of Variance for Fatigue Scores
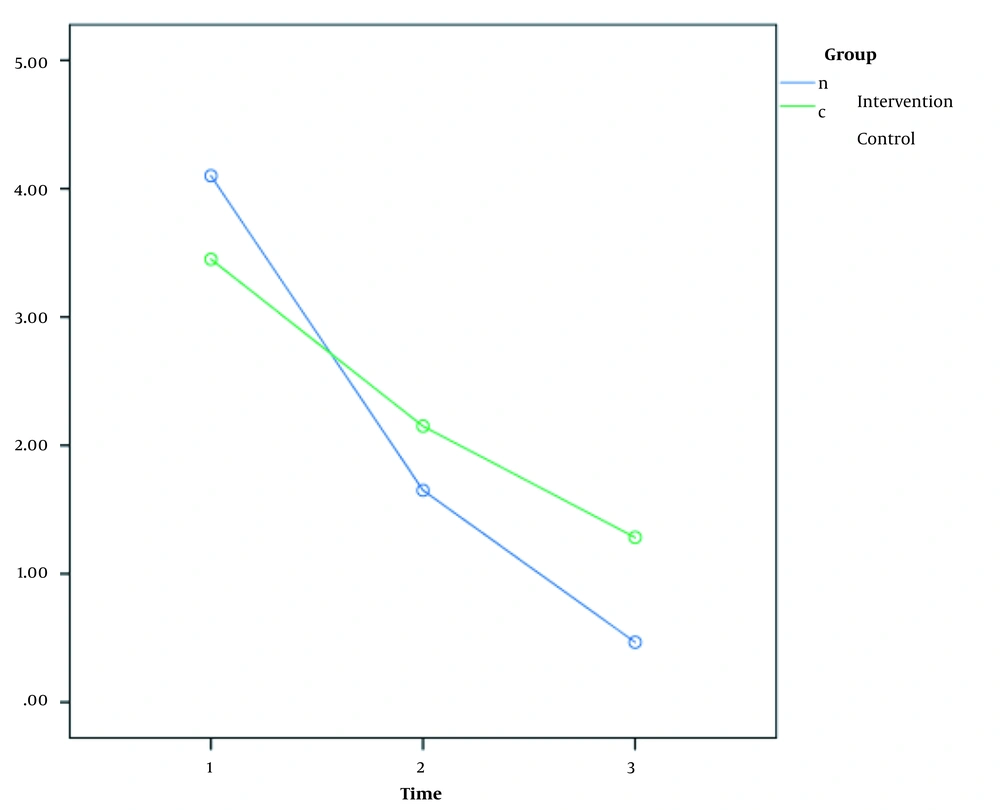
The mean dyspnea scores in the intervention group before, two weeks, and two months after the intervention were 4.10 ± 1.66, 1.65 ± 1.42, and 0.46 ± 0.66, and the corresponding values in the control group were 3.45 ± 1.73, 2.15 ± 1.21, and 1.28 ± 0.85, respectively. The dyspnea level in the two groups was significantly reduced two months after pulmonary rehabilitation compared to the pre-and post-intervention stages (P < 0.001). A significant difference was also observed in the control group (P < 0.001) (Figure 2). Moreover, the repeated measures ANOVA (Figure 1) indicated that the changes in the dyspnea scores over time were significant (P < 0.001), demonstrating a significant difference due to the effects of the intervention program (P = 0.04). In other words, the changes in the dyspnea scores were more remarkable in the intervention group than in the control group. Given the significance of the group-time interactive effect, the comparisons were made point by point and with Bonferroni correction again by time and group. The result showed that the mean score of the third stage had a statistically significant difference between the two groups (P < 0.001). The comparison of the means of three measurements in each group showed that in the intervention group, the mean scores two weeks and two months after the intervention were significantly different from the pretest score (P < 0.001). In the control group, this difference was significant in these two stages (P < 0.001) (Table 3).
| Variable | Sum of Squares | df | Mean Squares | F | P-Value |
|---|---|---|---|---|---|
| Time | 252.30 | 1 | 252.30 | 282.40 | 0.001 |
| Group | 2.22 | 1 | 2.22 | 0.53 | 0.04 |
| Group-time | 16.13 | 1 | 16.13 | 18.05 | 0.001 |
| Error | 240.728 | 58 | 4.150 |
Results of Repeated Measures Analysis of Variance for Dyspnea Scores
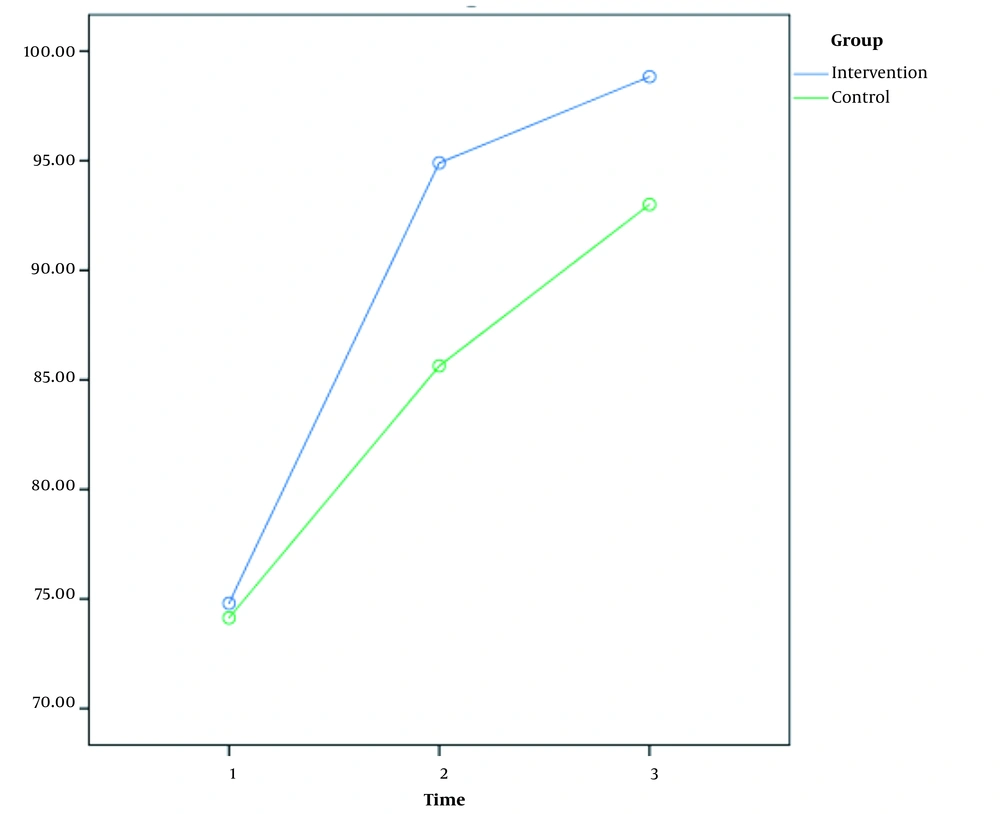
The mean scores of activities of daily living in the intervention group before, two weeks, and two months after the intervention were 74.80 ± 21.59, 94.90 ± 7.69, and 98.83 ± 2.32, and the corresponding values in the control group were 74.13 ± 27.45, 85.63 ± 18.57, and 93 ± 12.69, respectively (Figure 3). The repeated measures ANOVA (Figure 1) showed that the changes in the scores of activities of daily living over time were significant (P < 0.001), confirming a significant difference due to the effects of the intervention program. In other words, the changes in the scores of activities of daily living were more remarkable in the intervention group than in the control group (P = 0.03) (Table 4).
| Variable | Sum of Squares | df | Mean Squares | F | P-Value |
|---|---|---|---|---|---|
| Time | 13803.07 | 1 | 13803.07 | 63.40 | 0.001 |
| Group | 1242.93 | 1 | 1242.93 | 1.91 | 0.03 |
| Group-time | 200.20 | 1 | 200.20 | 0.92 | 0.34 |
| Error | 37589.611 | 58 | 648.097 |
Results of Repeated Measures Analysis of Variance for Activities of Daily Living Scores
5. Discussion
The results showed that home-based pulmonary rehabilitation reduced fatigue and dyspnea and improved the activities of daily living of COVID-19 patients. Accordingly, the levels of fatigue and dyspnea decreased in the intervention group. Moreover, the intervention group reported significantly higher levels of activities of daily living than the control group. Although the patients in both groups reported lower levels of fatigue and dyspnea after the intervention, the changes in the intervention group were more significant than in the control group. Thus, it can be suggested that the instructions provided through rehabilitation sessions helped patients learn rehabilitation and self-care skills and allowed them to participate in group discussions actively. Liu et al. evaluated the effects of six-week respiratory rehabilitation training on respiratory function in elderly patients with COVID-19 and found that the respiratory function was improved in the intervention group (20), in line with the results of the present study. Motaqi and Ghanjal (2020) and Soleimanifar and Hazrati reviewed previous studies on the effect of pulmonary rehabilitation and respiratory physiotherapy on the problems of COVID-19 patients. They showed that physiotherapy and respiratory rehabilitation could reduce respiratory problems in these patients (12, 15), confirming the present study results.
In their review study, Zhao et al. examined the effects of respiratory rehabilitation in adults with coronavirus disease. Respiratory rehabilitation treatment focuses on improving patients' lung function with coronavirus pneumonia. Contrary to the present study's findings, the results showed that due to the paucity of research in this field, there are still questions about the effect of respiratory rehabilitation treatment on improving lung function in patients with coronavirus pneumonia (27). Wang et al. conducted a review study on physical medicine and rehabilitation and pulmonary rehabilitation for COVID-19 and showed that pulmonary rehabilitation improved dyspnea, reduced anxiety, reduced complications, minimized disability, maintained function, and improved the quality of life in COVID-19 patients. There was a significant difference between pulmonary rehabilitation and routine care, and pulmonary rehabilitation effectively improved COVID-19 patients (16), confirming the results of the present study. Another review study by Abdullahi showed that chest physiotherapy could improve gas exchange and respiratory function, reverse pathological progression, and reduce the need for artificial ventilation in COVID-19 patients. However, there was limited evidence for the effectiveness of chest physiotherapy in COVID-19 patients, especially in the acute phase and in patients using ventilators. In contrast, chest physiotherapy in the form of respiratory muscle training, cough training, diaphragm training, stretching exercises, and home exercises in discharged patients improved FEV1 (L), FVC (L), FEV1/FVC%, lung capacity release for carbon monoxide (DLCO%), endurance, and quality of life and reduced the symptoms of anxiety and depression (28).
Demeco et al. conducted a review study on the rehabilitation of patients after COVID-19. They found that rehabilitation programs were effective in helping patients promote the quality of life, improve physical and respiratory function, and reduce anxiety and depression (19), as confirmed in the present study. A review study conducted in China examined the recommendations for respiratory rehabilitation in adults with coronavirus disease and showed that pulmonary rehabilitation could relieve the symptoms of dyspnea (27), similar to the present study. Moreover, Woo showed that three indices of dyspnea, fatigue, and physical activity were interrelated; thus, higher fatigue and lower physical activity were reported in COPD patients. This study, conducted on seven men and 15 women with chronic obstructive pulmonary disease, showed that the patients had more difficulty breathing with increasing dyspnea, leading to fatigue and decreased activity levels (8). Other studies (eg, Mahmoodi et al., Jokar et al., Heidari et al., Izadi et al. and Zakeri Moghadam et al.) showed that pulmonary rehabilitation of COPD patients was associated with significant positive effects on reducing complications such as fatigue and dyspnea and improving patients' activities of daily living (5, 9, 21, 29, 30).
One of the limitations of this study was the personal involvement of some patients, making it challenging to perform follow-up breathing exercises. Some of them could hardly devote time to their daily routine, and thus they could not answer the phone calls and follow the instructions given. Another limitation of this study was that the COVID-19 patients were not adequately cooperative in the training sessions due to weakness and lethargy caused by the disease. The other limitation of this study was the risk of disease transmission. Thus, some of the instructions were provided through educational video clips.
5.1. Conclusions
Home-based pulmonary rehabilitation measures were effective in fatigue, dyspnea, and activities of daily living of COVID-19 patients. Hence, using these respiratory rehabilitation programs by nurses can be effective in the treatment of chronic diseases.