1. Background
Hypertension is one of the leading global health problems (1). It is the most critical risk factor for cardiovascular disease (2) and the leading cause of 70% of coronary artery stenosis cases (3). As a silent killer, hypertension is the most common cause of death globally (4) and the second cause of death in Iran (3). Hypertension not only causes different physical problems but also is associated with mental health problems, so 50% of hypertensive patients suffer from anxiety and depression (5). Hypertension and mental problems aggravate each other and cause higher levels of disability (6). Hypertension, depression, anxiety, and stress are among the most common risk factors for coronary artery disease (7), stroke, myocardial infarction, and atrial fibrillation (8). Therefore, timely interventions are needed to manage these disorders effectively.
Lifestyle is a significant factor contributing to hypertension. An unhealthy lifestyle such as low levels of physical activity, cigarette smoking, unhealthy eating, and weight gain can cause stress and anxiety, significantly increase the risk of hypertension and coronary artery disease, and slow down patient recovery. Therefore, lifestyle modification may help manage hypertension and reduce the risk of these problems (5). It is essential to pay attention to lifestyle modification during HTN management because after coronary artery angioplasty, the permanence of risk factors, especially HTN, could result in the recurrence of coronary artery stenosis or decrease the success rate of treatment (9, 10). Studies show that lifestyle modifications can manage hypertension, such as weight loss, adherence to dietary regimens, limited salt intake, increased physical activity (11), stress management, smoking cessation, and alcohol abstinence (12). Moreover, lifestyle modification can significantly contribute to effective stress management (13). However, patients may have inadequate knowledge about healthy lifestyle behaviors.
Family support is a significant factor behind lifestyle modification (14). Family support also has significant correlations with engagement in physical activity (15), weight loss, healthy eating (14), depression, anxiety, stress management (14, 16), and hypertension self-management (17). Nevertheless, most family members of patients with chronic illnesses have limited knowledge of illnesses, their manifestations, treatments, and behavior reinforcement (16). Thus, educational programs are needed to enhance the health and lifestyle-related knowledge of patients and their family members. Nurses can play significant roles in lifestyle modification through education (18) and are more potent than other healthcare providers in hypertension management (19).
Some studies reported that educational interventions positively affect lifestyle modification (20) and management of depression, anxiety, and stress (21). Lifestyle modification, in turn, was reported to help manage hypertension and cardiovascular disease (20). However, there are controversies over the effects of lifestyle education on depression, anxiety, stress, and family support among patients with cardiovascular disease. For instance, a study reported that four-week group education about physical exercise, medications, diet, weight control, stress management, and relaxation had no significant effects on depression, anxiety, and stress among open-heart surgery candidates (13). Another study showed that 16-week group education had no significant effects on stress among hypertensive patients (22). Moreover, a study showed that 12-week group cognitive-behavioral education about coronary artery disease did not significantly reduce depression and anxiety (23). In another study, face-to-face patient and family education about physical activity, smoking cessation, alcohol abstinence, physical activity, medication, dietary regimens, depression, anxiety, and stress management was ineffective in reducing stress among patients with myocardial infarction (24). Several studies in different parts of the world also showed the significant effects of different educational interventions on blood pressure (13, 21), depression, anxiety, and stress (24-26) among patients with cardiovascular disease. These contradictory results about the effectiveness of educational interventions highlight the necessity of further studies to produce firm evidence. In addition, as hypertension and its associated mental health problems are multifactorial, multi-component educational interventions are needed for their management (7, 27). However, there are limited studies, if any, in Iran into the effects of multi-component educational interventions. The present study was conducted to narrow these gaps.
2. Objectives
This study aimed to evaluate the effects of lifestyle education on depression, anxiety, stress, and perceived family support among hypertensive patients undergoing coronary angioplasty.
3. Methods
This randomized clinical trial was conducted from November to April 2015 in the Cardiac Specialized Hospital of Isfahan, Iran. The study population comprised hypertensive patients hospitalized in coronary care units who had undergone coronary angioplasty in the study setting. Eligible subjects were recruited based on the following criteria: age more than 40, basic literacy skills, hypertension history of systolic blood pressure more than 140 mmHg and diastolic blood pressure of more than 90 mmHg, good clinical status as determined by a cardiologist, residence in Isfahan city, having an accompanying family member, having angioplasty history, no weight-reducing or weight-gaining dietary regimen, no use of relaxation techniques such as yoga or meditation, no history of acute cardiovascular disease (such as secondary hypertension), type I or II diabetes mellitus, hormonal or renal disorders and mental illnesses, no history of participation in hypertension-related educational programs, and no limitation in doing physical activity. The patients were excluded if they experienced acute and severe stress, experienced wide blood pressure fluctuations that needed medication changes, and had two or more absences from educational sessions. Recruited patients were randomly allocated to control and intervention groups to use a table of random numbers.
The subjects were selected based on inclusion criteria using a convenience sampling method and were then randomly allocated to two intervention and control groups. For this purpose, Card No. 1 and Card No. 2 were placed in a closed pocket. People who selected Card No. 1 were placed in the intervention group, and people who selected Card No. 2 were placed in the control group.
The sample size was determined to be 30 patients in each group; however, we recruited 35 patients to compensate for possible dropouts. The sample size was calculated based on the findings of a former study (28). Sample size calculation parameters were a confidence level of 0.95, a power of 0.80, and a change in depression, anxiety, and stress total mean score as much as 0.80 of its standard deviation.
Z1 = 1.96, Z2 = 0.84, d = 0.8 S
3.1. Instruments
Three instruments were used to collect the study data before, immediately, and one month after the study intervention. The first instrument was a demographic questionnaire with items on age, educational level, marital status, employment status, financial status, and blood pressure.
The second instrument was the 21-item Depression, Anxiety, and Stress Scale. This scale is the short version of the 42-item Depression, Anxiety, and Stress Scale developed by Lovibond and Lovibond in 1995. The 21 items of this scale are responded as “Never,” “Somewhat,” “Moderately,” and “Mostly," scored 0 – 3, respectively. Therefore, the scale's total score ranges 0 – 63, and the possible total scores of its seven-item depression, anxiety, and stress domains range 0–21. The domain scores are interpreted as 0 – 4: Normal, 5 – 11: Moderate problem, and more than 12: Severe problem. An earlier study confirmed the content validity and reliability of the Persian version of this scale with Cronbach’s alpha values of 0.80, 0.83, and 0.87 for its depression, anxiety, and stress domains, respectively (21). This scale was completed by participating patients and/or their family members through the self-report method.
The third study instrument was a researcher-made family support questionnaire developed based on a literature review (14-17, 24, 25, 28, 29) and consulting with several experts to obtain adequately qualified family support. A primordial version of the instrument was developed and presented to 10 experts in the Schools of Nursing & Midwifery and Medicine for advice regarding the instrument's content validity and a revised questionnaire based on viewpoints. For reliability assessment, 25 eligible patients completed the questionnaire, and then, its Cronbach’s alpha was calculated to be 0.723. Blood pressure was also measured using a calibrated mercury sphygmomanometer at a sitting position from the right hand based on the standard procedure. Each of the 25 items of this questionnaire was scored from 0 (Never) to 4 (Always). The total score of this questionnaire could range from 0 to 100, which was interpreted as follows: 0 – 25: weak family support, 26 – 50: moderate family support, 51 – 75: good family support, and 76 – 100: strong family support.
3.2. Intervention
Subjects in the intervention group were divided into two eight-person and two seven-person groups. Then, the intervention group was provided with the educational program in six sessions during three successive weeks, each lasting 45 - 60 min, and then follow-ups were done weekly by phone calls (30). During educational sessions, teaching methods such as lecture, question-and-answer, group discussion, scenario and video presentation, and educational booklet were used to provide the patients and their family members with education about hypertension, its risk factors and complications, dietary modification, increasing physical activity, management of depression, anxiety, and stress, and minimizing alcohol consumption, smoking, and drug abuse. Educational materials were produced based on hypertension prevention and management guidelines (13, 31). Moreover, the importance of family support in hypertension management was highlighted, and the methods for supporting hypertensive patients were addressed. At the beginning of each session, an educational booklet was also given to each participant, which contained educational materials on the same topic addressed in that session. Before each session, personal telephone contact was made to remind each participant of the time of the session. After the educational program, follow-up telephone contacts were made with the patients and their family members to assess their problems,
help them find and analyze solutions, and provide them with feedback (Table 1).
| Sessions | Educational Content |
|---|---|
| First session | Definition of high blood pressure, sorting and diagnosing high blood pressure, the number of follow-ups and referring to the physician, complications and risk factors of high blood pressure, methods of treating and controlling high blood pressure, describing coronary angioplasty. |
| Second session | DASH diet, the importance of diet and its effect on controlling blood pressure, foods that could lower blood pressure, foods that could increase blood pressure, the proper method of cooking foods and its importance, the advantages of low-salt and DASH diets. |
| Third session | Appropriate duration, repetition, and type of exercise for subjects, the importance of increasing physical activity, inappropriate exercises, how to lose weight and its effect on controlling blood pressure, the risks of weight gain, the effect of an increase in the waist, abdomen size, and hip on blood pressure, the advantages of an increase in physical activity. |
| Fourth session | The importance of regular drug treatment, different blood pressure-lowering drugs, drug interactions, the proper consumption method of drugs based on their dose and timing, and considering drug interactions and side effects. |
| At the end of this session, a scenario about some patients who have experienced acute complications due to a lack of control of their blood pressure was given to the subjects, and they were asked to study it before the subsequent sessions. | |
| Fifth session | Reviewing scenarios in groups, presenting a video about a patient with high blood pressure, stress-coping methods, the advantages of stress management, the effect of stress and tension on blood pressure, relaxation, and muscle releasing methods. |
| Sixth session | The role of family involvement in patient support, effective communication skills to increase the patient's emotional support, practicing and repeating the skills using supportive strategies and conversations. Questions and answers with examples with their families about educational content. |
| Phone follow-up | Reviewing topics and obstacles, helping subjects remove the obstacles, answering subjects’ questions, and encouraging feedback. |
For patients in the control group, two group discussions were held on their hypertension experiences, dietary regimen, physical activity, and weight loss, while they were not provided with any positive or negative feedback.
The posttest was performed after the end of the educational sessions, and the final test was done one month after the sessions for both groups.
3.3. Ethical Considerations
This study was approved by the Ethics Committee of Isfahan University of Medical Sciences, Isfahan, Iran (code: IR.MUI.REC.1395.2.108). It was also registered in the Iranian Registry of Clinical Trials (IRCT2015062420912N3). Written permissions for the study were obtained from the authorities of Isfahan Nursing & Midwifery Faculty, Isfahan, Iran, and provided to the authorities of the study setting. The study's objectives were explained to the study sample and the authorities of the study setting. Written informed consent was obtained from all patients, and they were assured of the confidentiality of data management and their freedom to withdraw from the study voluntarily.
3.4. Data Analysis
Data were analyzed using SPSS software (v. 16). Between-group comparisons respecting categorical demographic characteristics (such as gender, marital status, and educational and financial status) were made through the chi-square and the Mann-Whitney U tests. Moreover, between-group comparisons respecting age, blood pressure, depression, anxiety, stress, and family support were made through the independent-sample t test or the repeated-measures analysis of variance, followed by the Least Significant Difference post hoc test. On the other hand, within-group comparisons were made using the paired-sample t test, the repeated-measures analysis of variance, and the Least Significant Difference post hoc test. For all statistical analyses, the significance level was P < 0.05.
4. Results
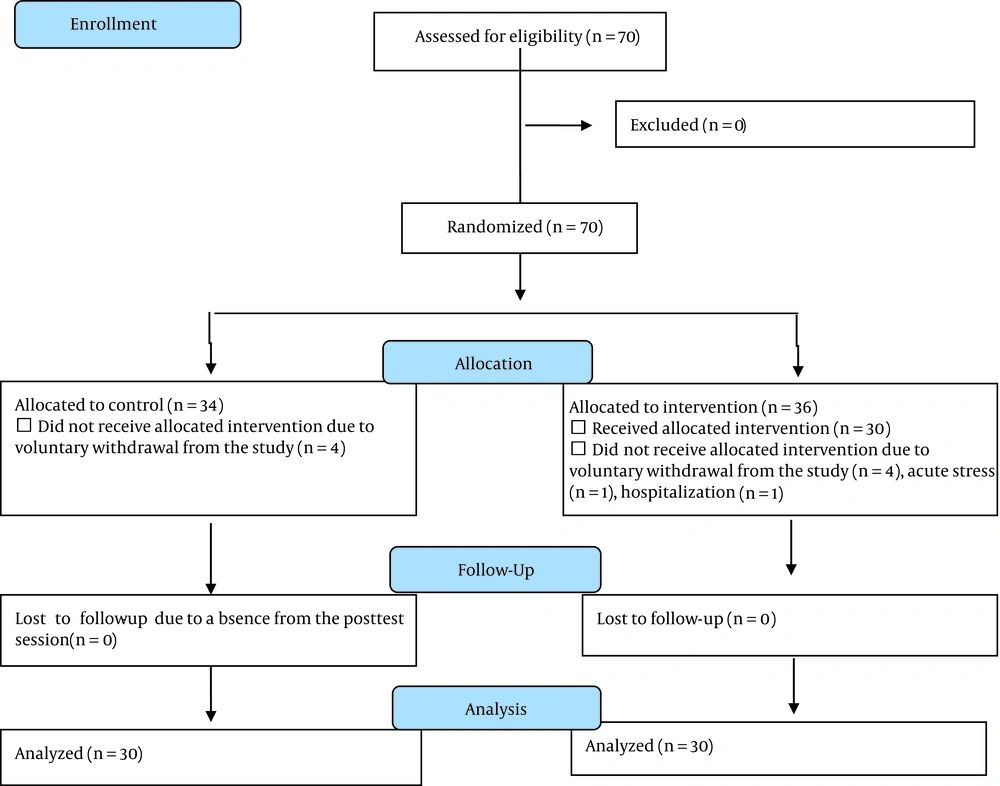
In total, 70 patients were recruited in the study. However, 10 patients were excluded due to either unilateral withdrawal (n = 8), experiencing acute stress (n = 1), or hospitalization (n = 1) during the study. Accordingly, the study was completed with 60 patients (n = 30 in each group) (Figure 1).
All subjects in both groups were married, and most of them were males (86%), had moderate financial status (56%), and had basic literacy skills (75%). The mean age in the intervention and control groups was 58.4 ± 6.5 and 55.6 ± 6.5, respectively. The groups did not significantly differ respecting their background characteristics (P > 0.05; Table 2).
| Characteristics | Group | P Value | |
|---|---|---|---|
| Intervention | Control | ||
| Age (y) | 58.4 ± 6.5 | 55.6 ± 6.5 | 0.114b |
| Systolic blood pressure | 144.4 ± 18.1 | 142.5 ± 15.2 | 0.673b |
| Diastolic blood pressure | 84.3 ± 9.01 | 84.9 ± 10.7 | 0.815 b |
| Length of suffering from hypertension (y) | 3.5 ± 3.4 | 3.3 ± 3.1 | 0.820 b |
| Marital status | 0.754 c | ||
| Married | 29 (96.7) | 29 (96.7) | |
| Widowed | 1 (3.3) | 1 (3.3) | |
| Employment status | 0.286 c, 0.315, Z = 0.934 | ||
| Employee | 1 (3.3) | 0 | |
| Housewife | 4 (13.3) | 4 (13.3) | |
| Retired | 7 (23.4) | 11 (36.7) | |
| Worker | 2 (6.7) | 5 (16.7) | |
| Businessman | 16 (53.3) | 10 (33.3) | |
| Financial status | 0.421d, Z = 0.81 | ||
| Poor | 12 (40) | 9 (30) | |
| Medium | 16 (53) | 18 (60) | |
| Good | 2 (7) | 3 (10) | |
| Educational level | 0.880 d, Z = 0.15 | ||
| Primary school | 21 (70) | 24 (80) | |
| Pre-diploma | 3 (10) | 3 (10) | |
| Diploma | 6 (20) | 3 (10) | |
aValues are expressed as mean ± SD or No. (%).
b The results of the independent-sample t test
c Fisher’s Exact Test
d The results of the Mann-Whitney U test
The results of the repeated-measures ANOVA showed that the mean scores of depression, anxiety, stress, and family support in the control group did not significantly change across the three measurements (P > 0.5; Table 3). However, with downward trends, the variations of the mean scores of depression, anxiety, and stress in the intervention group were statistically significant. The same finding was also observed with an upward trend respecting the variations of the mean score of family support in the intervention group (P < 0.05; Table 3). The Least Significant Difference post hoc test revealed that the mean scores of depression, anxiety, and stress at the first and second posttests in the intervention group were significantly lower than their corresponding pretest values. Moreover, the mean score of family support at the first and second posttests was significantly greater than its pretest value. In addition, there were significant differences between the two posttests respecting the mean scores of anxiety, stress, and family support in the intervention group (P = 0.001). However, there was no significant difference between the two posttest mean scores of depression (P = 0.057).
| Outcomes | Before | After | One Month After | P Valuea | P Valueb |
|---|---|---|---|---|---|
| Depression | 0.001 | ||||
| Control | 9.7 ± 1.8 | 9.4 ± 2.0 | 9.7 ± 2.0 | 0.27 | |
| Intervention | 9.6 ± 1.9 | 7.1 ± 2.1 | 6.4 ± 1.4 | 0.001 | |
| P valuec | 0.85 | 0.001 | 0.001 | - | |
| Anxiety | 0.001 | ||||
| Control | 10.3 ± 1.8 | 9.5 ± 2.0 | 9.6 ± 2.0 | 0.10 | |
| Intervention | 9.9 ± 1.8 | 7.6 ± 1.5 | 6.7 ± 1.6 | 0.001 | |
| P valuec | 0.40 | 0.001 | 0.001 | - | |
| Stress | 0.001 | ||||
| Control | 13.3 ± 1.7 | 12.5 ± 2.1 | 12.3 ± 2.0 | 0.09 | |
| Intervention | 13.4 ± 1.54 | 9.2 ± 1.9 | 8.0 ± 1.57 | 0.001 | |
| P valuec | 0.90 | 0.001 | 0.001 | - | |
| Family support | 0.001 | ||||
| Control | 30.29 ± 4.3 | 33.5 ± 4.7 | 32.4 ± 5.2 | 0.21 | |
| Intervention | 31.0 ± 4.0 | 52.2 ± 5.5 | 57.2 ± 6.1 | 0.001 | |
| P valuec | 0.98 | 0.001 | 0.001 | - |
a The results of repeated-measures analysis of variance for the effects of time
b The results of repeated-measures analysis of variance for the effects of group
c The results of independent-sample t test for between-group comparison
The independent-sample t test showed no significant between-group differences respecting the pretest mean scores of depression, anxiety, stress, and family support (P > 0.05; Table 3). However, at both posttests, the mean scores of depression, anxiety, and stress were significantly lower in the intervention group than in the control group, and the mean score of family support was significantly greater in the intervention group than in the control group (P < 0.05; Table 3).
5. Discussion
The study findings implied the effectiveness of the lifestyle education intervention in reducing depression, anxiety, and stress and improving family support. In line with these findings, an earlier study found that multimedia nursing education for patients in the coronary care unit had significant effects on their depression, anxiety, and stress (32). Similarly, a study showed that positive thinking training significantly reduced depression, anxiety, and stress in coronary heart disease patients (33).
We also found a significant decrease in the mean score of depression immediately after the study intervention. Similarly, a study showed that an educational program on mindfulness-based stress reduction effectively reduced depressive symptoms among patients with coronary artery disease and hypertension (34). In addition, Rezapour et al. (2016) showed that the implementation of collaborative care could be associated with lower depression, anxiety, and stress in patients after coronary angioplasty (34). However, our findings showed that though the mean score of depression at the second posttest was lower than the mean score of depression at the first posttest, the difference was not statistically significant. This finding may be because a longer follow-up period is needed to observe the long-term effects of educational interventions on mood status.
The study findings also indicated a significant decrease in the mean score of anxiety and stress between the first and second posttests. These findings are in line with the findings of several former studies. For instance, a study showed that face-to-face and written lifestyle education (about smoking cessation, physical activity, adherence to treatment and dietary regimens, and blood pressure and stress management) effectively reduced anxiety among patients with cardiovascular problems, even four months after the intervention (34, 35). Another study found the significant effects of an eight-session educational program (mindfulness-based stress reduction) on anxiety and stress, which lasted three months after the intervention (32). Moreover, a study on patients with special diseases (such as multiple sclerosis, thalassemia major, hemophilia, and renal failure) reported that three months after a seven-session group education (about problem-solving, stress management, physical activity, and relaxation), patients had significantly lower levels of anxiety and stress compared with before the intervention (34). These findings highlight the positive effects of multi-component lifestyle education on anxiety and stress among patients with chronic conditions.
Another study finding was a significant increase in the mean score of perceived family support from the first to third measurements. In other words, lifestyle education for our subjects and their family members significantly improved their perceived family support. Family support can facilitate the management of hypertension, depression, anxiety, and stress because family members can support and reinforce patients’ attempts for behavior modification (36). The education of family members about how to support their patients was also reported to be a significant factor behind the improvement of self-care ability among patients with heart failure (31). Two earlier studies also reported that patient and family education about healthy lifestyle and lifestyle-related factors behind hypertension significantly reduced blood pressure among hypertensive patients (37, 38). Lifestyle is affected by family members, and hence, lifestyle modification necessitates family education and modifications in the whole family. For effective behavior modification, family members need to receive education to obtain the ability to identify and understand their patients’ needs, support their treatment plans, and help them properly adhere to medical and nursing recommendations.
Unlike our findings, a study reported the ineffectiveness of a four-week group education program (related to physical activity, treatment and dietary regimens, weight control, relaxation, and stress management) in significantly reducing depression, anxiety, and stress among the candidates of open-heart surgery (13). Another study also reported that a 16 -week lifestyle education program (focusing on weight loss, limiting alcohol and salt intake, regular physical activity, and relaxation techniques) had no significant effects on stress among hypertensive patients (21). Similarly, a study showed the insignificant effects of a 12 -session group lifestyle education on depression and anxiety, although it significantly reduced stress (23). Another study also found that face-to-face patient and family education significantly reduced depression and anxiety while not significantly affecting stress among myocardial infarction patients (24). Disagreements between the findings of the mentioned studies and ours could be attributed to factors such as the characteristics of samples and instructors, environmental factors, teaching methods, personal attitudes, and the length of educational courses. Education in our study was provided by a nurse, while psychologists or traditional medicine therapists had provided education in those studies. Nurses have closer relationships with patients and a better understanding of their educational needs and hence, can play significant roles in the modification of patients’ lifestyles through offering them quality education (18). Moreover, our subjects were patients with hypertension and angioplasty, and the study intervention was a multi-component face-to-face lifestyle education program accompanied by follow-up telephone contacts, while those studies dealt only with some aspects of lifestyle. Multi-component lifestyle modification has greater effects on patients' knowledge, attitudes, and practice with hypertension and angioplasty (38). Besides, our study intervention included scenario presentation and group discussion, with the active participation of study subjects and their family members.
These differences in the results of the present study and previous studies could be due to the use of different educational methods (lecture, question-and-answer, group discussion, reviewing scenarios, videos, and booklets), and the use of an educational program for all aspects of the subjects’ lifestyles, supporting the family and following up the participants.
The short follow-up period and small sample size were among the study limitations. Therefore, studies with longer follow-up periods and larger samples are recommended to evaluate the effects of lifestyle education and family support on blood pressure, stress, anxiety, and depression.
5.1. Conclusions
This study showed that multi-component lifestyle education provided to patients through lecture, question-and-answer, group discussion, scenario and video presentation, and the educational booklet effectively reduced depression, anxiety, and stress and improved perceived family support among patients with hypertension and angioplasty. Therefore, nurses can integrate multi-component lifestyle education into their care plans to improve patient outcomes. As professional members of the health system, the nurses have essential roles in educating and supporting patients with chronic diseases such as blood pressure. They also can play a role in lifestyle modification through suitable patient education approaches, such as lifestyle education used in this study. Moreover, nurses are recommended to educate and encourage family members to support their patients and follow a healthy lifestyle.