1. Background
Cancer is a family of diseases that are caused by abnormal cell growth that can lead to an invasion or spread to other parts of the body (metastasis). The World Health Organization (WHO) estimated 18.1 million new cases of cancer and 9.6 million deaths in 2018 (1).
According to the WHO, the incidence of breast cancer in 2018 was 2 million new cases accounting for one-third of deaths (2). Breast cancer is more common in developed countries (3) and is the second most common cause of cancer death in women after lung cancer and the second most common cancer in women after non-melanoma skin cancer (4).
Chemotherapy and radiation therapy are used in most malignant cancers as the main or adjunctive treatment with various complications, including the destruction of epithelial cells, and its most common form is mucositis. Other complications following cancer treatments include infertility (5), immunosuppression, gastrointestinal disorders (6), anemia (7), secondary neoplasms (8), etc. Mucositis is a painful inflammation and mucosal ulcer that affects the upper gastrointestinal tract (9). Oral mucositis is a common complication and, in many cases, a debilitating symptom in the treatment of cancer (10). The prevalence of mucositis has been reported to be approximately 80 - 100% in high-dose chemotherapy, 40% in standard doses, and 10 - 15% in low-dose treatments (11-13).
Mucositis as a complication of chemotherapy and radiotherapy leads to impaired quality of life, reduced nutritional quality, and oral pain, eventually forcing the patient to use painkillers. Painful mucositis may lead to the rejection of the treatment and drastically reduce the prognosis (14, 15). Due to the functional problems caused by oral mucositis, developing a standard nursing approach for preventing and treating mucositis caused by chemotherapy or radiotherapy is essential. To date, various methods have been examined or used in some cases for the prevention and treatment of mucositis, including non-pharmacological treatments (e.g., laser and cryotherapy), topical drugs, antibiotics and antiseptics, antifungals, anti-inflammatory drugs, combined mouthwashes, hematopoietic growth factor, local anesthesia, systemic drugs, cellular protectors, immunosuppressants, and antiviral drugs. However, despite numerous studies, no definite and definitive treatment for mucositis has been introduced, and the existing treatments are not complete, and each has some advantages and disadvantages (13, 16-18). For instance, Ashktorab et al. (2010) found that mouthwash with peppermint essential oil can play a role in preventing chemotherapy-induced mucositis in cancer patients (19). In many studies, the use of honey is effective in reducing oral mucositis (20). However, studies have shown that the use of honey has only improved 30% of patients (in the treatment group) and is not significantly different from routine interventions (21). Thus, it can be argued that there is still a long way to develop compounds that can effectively lead to the prevention and definitive treatment of oral mucositis. As noted earlier, oral mucositis is more severe in certain treatment regimens and is found in all age groups with cancer (22). Complementary medicine is used to control pediatric mucositis, which has a limited effect. For example, a study found that the use of chamomile can be effective in preventing chemotherapy-induced stomatitis in children (23). Thus, further studies are needed to explore interventions in which patients play a more active role. One of these interventions is to engage patients in self-care behaviors. In other words, one of the determining and effective factors in maintaining health and preventing the aggravation of signs and symptoms of diseases, especially chronic diseases, is to perform self-care behaviors. The WHO defines self-care as the ability of individuals, families, and communities to promote health, prevent disease, maintain health, and restore health with or without the support of a healthcare provider (24). Self-care behaviors can reduce the complications of the disease by 80%, improve the abilities, promote the performance of daily activities, and contribute to the patient’s independence (25). Studies have shown that adherence to self-care behaviors leads to reduced readmission, improved quality of life, and reduced treatment costs for patients (26, 27).
Self-care behaviors for breast cancer include following a treatment regimen, healthy lifestyle, more mobility and physical activity, controlling risk factors (high blood pressure, smoking, and stress), seeing a doctor if there are any side effects, including mucositis, and performing timely medical tests (28).
Previous studies have suggested that adherence of patients to self-care behaviors, in addition to preventing the aggravation of symptoms, is effective in reducing patient mortality and feeling healthier (29, 30). Shahsavari et al. (2015) showed that self-care training leads to increasing and improving patients' quality of life. They also stated that adding self-care training to the routine care provided by nurses to patients could affect treatment outcomes and highlight the importance of nurses’ role (31). Therefore, the need to improve self-care ability through patient education and the importance of the role of nurses in managing complications and preventing them is undeniable as one of the principles of nursing in patient care and treatment is self-care training by nurses. Furthermore, the nursing policy relies on self-care for several reasons, and the quality of self-care is dependent on nurses (32). One of the important functions of nurses is to educate the patient. Thus, if the patient receives information about his/her illness and care process, he/she will be more willing to participate in the required care. On the other hand, the patient can participate in the process of recovery and accelerate it based on the training received in the hospital and after discharge by observing some instructions.
2. Objectives
To this end, this study sought to examine the effect of self-care training on the severity of oral mucositis in patients with breast cancer undergoing chemotherapy in the chemotherapy wards of teaching hospitals in Zahedan.
3. Methods
This study was a quasi-experimental study with two groups, and a pre-test-post-test design on 74 patients with breast cancer admitted for chemotherapy to Khatam Al-Anbia and Ali Ibn Abi Talib (AS) hospitals Zahedan, southeast Iran in 2020. The sample size was estimated as 33 persons per group based on the ratio formula and the percentage of oral mucositis incidence after chemotherapy (19) and considering the 95% confidence interval and 90% test power in each group. Nevertheless, taking into account the 10% dropout, the sample size in each group was estimated to be 37 patients (74 patients in total) (19).
Z1 – α/2 = 1.96; Z1 – β = 1.64; P1 = 0.15; P2 = 0.50;
The participants were patients who visited the ward with a diagnosis of breast cancer and met the inclusion criteria (attending the first chemotherapy session, the age range between 20 - 60 years, no metastasis, no oral malformation, no oral infections at the beginning of the study, and no diabetes). Before the start of the first chemotherapy session and after obtaining written consent, some information was provided to the participants about the objectives of the study, its duration, the research procedure, and the exclusion criteria. The presence of oral mucositis was checked using the WHO Oral Mucositis Grading Scale. The scale divides oral mucosa into four grades (0 - 4): No oral mucositis (grade 0), the presence of oral soreness and erythema (grade 1), the presence of oral erythema and ulcers with solid diet tolerated (grade 2), the presence of oral ulcers with liquid diet only (grade 3), and oral alimentation impossible (grade 4) (33). The scale has been validated for use in Iran (34), and its validity has been confirmed in many studies (35, 36). The reliability of the instrument was confirmed in the present study using inter-rater or inter-observer reliability with a Kappa coefficient of 0.8.
The participants were selected using convenience sampling and were then assigned to the two groups via simple random allocation. To this end, an envelope containing cards A and B equal to the total number of participants was used. Each patient who met the inclusion criteria was asked to choose one of the cards at random. If card A was selected, the patient was placed in the control group, and the patients who selected card B were assigned to the intervention group.
The participants in the intervention group attended four 30-minute training sessions with content approved by an oncologist. The instructions were provided face-to-face and individually with the use of manuals dental models to show the correct use of oral hygiene items, such as toothbrushes, dental floss, and mouthwash. The training sessions were conducted before the start of weekly chemotherapy for four consecutive weeks. In other words, four training sessions were held up to the first four weeks of chemotherapy, and mucosal evaluation was performed every two weeks, i.e., in the second, fourth, sixth, and eighth weeks. To control the bias in the study, a double-blind protocol was used. To this end, a trained nurse was used as a research assistant to fill out the Oral Mucositis Grading Scale and analyze the data. She did not know the group each participant belonged to. The training intervention began in the first chemotherapy session for the patients who met the inclusion criteria. Since the course of chemotherapy treatment was eight weeks, the intervention was performed in the first four sessions, and mucosal evaluation was performed by a trained researcher. Afterward, in the second, fourth, sixth, and eighth weeks during the chemotherapy sessions, the patients were evaluated for mucositis four times. At the end of the intervention, a training booklet was given to the participants in both intervention and control groups.
The collected data were codified and then analyzed using SPSS 26 software. The data were summarized using descriptive statistics, including percentage, mean, standard deviation, minimum, and maximum. Shapiro-Wilk test was run to evaluate the normality of the data. The chi-square test was used to compare the prevalence of mucositis in the two groups in different weeks. Independent samples t-test and Fisher’s exact test were used to compare intergroup means. Moreover, the generalized estimation equation (GEE) test was used. All statistical procedures were performed at the significance level of less than 0.05 (P < 0.05).
4. Results
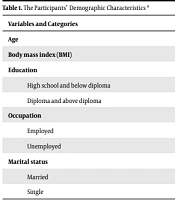
In the present study, 74 patients participated, but there was no statistically significant difference between the two groups in terms of demographic variables of age, education, occupation, and marital status (Table 1).
| Variables and Categories | Intervention Group | Control Group | P-Value |
|---|---|---|---|
| Age | 45.16 ± 8.20 | 45.52 ± 9.15 | 0.86 b |
| Body mass index (BMI) | 33.03 ± 3.7 | 23.10 ± 3.2 | 0.92 c |
| Education | 0.82 c | ||
| High school and below diploma | 18 (48.6) | 17 (48.6) | |
| Diploma and above diploma | 19 (51.4) | 20 (51.4) | |
| Occupation | 0.68 c | ||
| Employed | 11 (52.6) | 10 (47.7) | |
| Unemployed | 26 (47.4) | 27 (52.6) | |
| Marital status | 0.65 c | ||
| Married | 30 (80.6) | 28 (76.3) | |
| Single | 7 (19.4) | 9 (23.7) |
a Values are expressed as mean ± SD or No. (%).
b Independent samples t-test.
c Chi-square test.
As shown in Table 2, the only variable that plays a significant role in the occurrence of mucositis is the self-care intervention. Furthermore, the probability of developing mucositis is different in the two groups so that the group receiving the training intervention was significantly less likely to develop mucositis (OR = 0.02; P = 0.03), and other variables had no significant effect on the possibility of developing mucositis.
| Variables | OR | Standard Error | Confidence Interval (95%) | Sig. |
|---|---|---|---|---|
| Smoking vs. non-smoking | 0.267 | 1.71 | 0.009 - 7.68 | 0.44 |
| Intervention vs. control | 0.02 | 1.74 | 0.001 - 0.798 | 0.037 |
| BMI < 25 vs. BMI > 40 | 6.62 | 11.73 | 0.068 - 6.48 | 0.084 |
| BMI < 30 vs. BMI > 40 | 3.04 | 9.72 | 0.160 - 5.78 | 0.076 |
| Age | 0.94 | 0.064 | 0.827 - 1.07 | 0.352 |
At the end of the second week, 94.4% of the patients in the intervention group and 92.1% of patients in the control group had no oral mucositis. Moreover, 5.6% of the patients in the intervention group and 7.9% of patients in the control group reported oral soreness and erythema. However, the chi-square test indicated no statistically significant difference between the two groups (P = 0.6) (Table 3).
| Mucositis | Intervention Group | Control Group | Chi-Square |
|---|---|---|---|
| No mucositis | 35 (94.4) | 34 (92.1) | |
| Oral soreness and erythema | 2 (5.6) | 3 (7.9) | |
| Total | 37 (100) | 37 (100) | χ2 = 0.16; df = 1; P = 0.6 |
a Values are expressed as frequency (%).
According to Table 4, at the end of the fourth week, 94.4% of the patients in the intervention group and 81.6% of the patients in the control group had no mucositis. Furthermore, 5.6% of the patients in the intervention group and 13.2% of the patients in the control group reported soreness and erythema. However, only 5.3% of the patients in the control group reported oral erythema and ulcers with solid diet tolerated. In addition, there was no statistically significant difference between the two groups, as indicated by the chi-square test (P = 0.18).
| Mucositis | Intervention Group | Control Group | Chi-Square |
|---|---|---|---|
| No mucositis | 35 (94.4) | 31 (81.6) | |
| Oral soreness and erythema | 2 (5.6) | 4 (13.2) | |
| Oral erythema and ulcers with solid diet tolerated | 0 (0) | 2 (5.3) | |
| Total | 37 (100) | 37 (100) | χ2 = 3.37; df = 2; P = 0.18 |
a Values are expressed as frequency (%).
As shown in Table 5, at the end of the sixth week, 94.4% of the patients in the intervention group and 81.6% of the patients in the control group had no oral mucositis. Furthermore, 2.8% of the patients in the intervention group and 2.6% of the patients in the control group reported soreness and erythema. In addition, 2.8% of the patients in the intervention group and 15.8% of the patients in the control group reported oral erythema and ulcers with solid diet tolerated. However, the chi-square test indicated no statistically significant difference between the two groups (P = 0.16).
| Mucositis | Intervention Group | Control Group | Chi-Square |
|---|---|---|---|
| No mucositis | 35 (94.4) | 31 (81.6) | |
| Oral soreness and erythema | 1 (2.8) | 1 (2.6) | |
| Oral erythema and ulcers with solid diet tolerated | 1 (2.8) | 5 (15.8) | |
| Total | 37 (100) | 37 (100) | χ2 = 3.65; df = 2; P = 0.16 |
a Values are expressed as frequency (%).
As can be seen in the Table 6, 94.4% of the patients in the intervention group had no mucositis at the end of the eighth week, but 60.5% of patients in the control group reported no oral mucositis. No patient in the intervention group reported oral ulcers with liquid and solid diet, while 17.2 of the patients in the control group reported the presence of oral ulcers with solid diet only. Moreover, the results of the chi-square test indicated a statistically significant difference between the two groups (P = 0.005).
| Mucositis | Intervention Group | Control Group | Chi-Square |
|---|---|---|---|
| No mucositis | 35 (94.4) | 31 (81.6) | |
| Oral soreness and erythema | 1 (2.8) | 1 (2.6) | |
| Oral erythema and ulcers with solid diet tolerated | 1 (2.8) | 5 (15.8) | |
| Total | 37 (100) | 37 (100) | χ2 = 3.65; df = 2; P = 0.16 |
a Values are expressed as frequency (%).
5. Discussion
The present study results indicated that self-care training has a positive effect on the severity of oral mucositis in patients with breast cancer undergoing chemotherapy. Mucositis or inflammation of the oral mucosa is often found in almost all patients undergoing chemotherapy as well as radiation therapy in the mouth, which is caused by the cytotoxic effect of chemotherapy drugs or the local effect of radiation on the oral mucosa. The data also showed that a small number of patients had mucositis in the second week, while in the eighth week, there was a significant difference between the two groups, and patients who received self-care training were less likely to develop oral mucositis. The results of the GEE test also suggested that the only variable affecting the severity of mucositis was the self-care intervention, and other variables, such as age, smoking, and BMI, did not play a role in mucositis.
The prevalence of drug-induced oral mucositis varies in patients undergoing chemotherapy. Oral problems are more severe in patients with leukemia (37). Studies have shown that severe mucositis can cause a temporary or complete cessation of treatment in cancer patients (38).
A review of the literature revealed that there was no study similar in terms of methodology to the present study, and most of the studies were conducted using a descriptive design on a group of patients or compared the two stages of chemotherapy and radiotherapy treatments in terms of severity of oral mucositis.
Jajarm et al. (2015) examined the risk factors affecting the incidence of mucositis due to head and neck radiation therapy and chemotherapy and showed that mucositis was less prevalent in patients treated with chemotherapy (39). The authors used a descriptive methodology that differed from the procedure used in the present study. However, it was similar to the present study in terms of the frequency of mucositis. Moreover, another study investigated the prevalence of oral mucositis due to chemotherapy and the risk of its factors in children with malignancy and showed that oral health status and type of treatment regimen played a very important role in the development of oral mucositis (40). The patients in the present study followed the same diet and all received adriamycin, cyclophosphamide, and paclitaxel; hence, the difference in mucositis between the two groups was certainly not related to their medication regimen. Thus, the only factor influencing the severity of mucositis in both groups can be related to self-care training. The self-care training program in this study placed much emphasis on the participants’ oral hygiene. During four sessions of oral hygiene training, the researcher taught patients how to use mouthwash and floss using a model. Thus, given that the confounding variables were controlled and the drug regimens were similar for the patients in the two groups, the difference in oral mucositis between the two groups could be attributed to the observance of oral hygiene. In the present study, oral examination was performed for mucositis, but specific criteria for assessing oral health were not considered in this study. However, the empirical data revealed that the patients who developed oral mucositis in the control group were patients with poor oral health, and they did not receive special training offered to the patients in the intervention group. Other studies also have highlighted that poor oral health causes a high risk of developing mucositis (41, 42). Nevertheless, some studies have shown no relationship between oral health status and the prevalence of mucositis (43). The results of the present study also indicated that a limited number of patients in both groups had erythema mucositis at the end of the second week of chemotherapy. Studies have indicated that chemotherapy-induced mucositis can begin 5 to 7 days after the start of treatment (44). The severity of mucositis was not significant in the fourth and sixth weeks. However, at the end of the eighth week, the number of mucosal cases was generally low, but it was more prevalent in the control group than the intervention group. In other words, the intervention conducted in the present study showed that self-care training could be effective in preventing mucositis over time. Although studies have suggested that oral mucositis is one of the main problems in cancer patients, the type of cancer and therapeutic regimen are among the most influential factors in the severity of mucositis (45, 46). Accordingly, Curra et al. (2018) reviewed 547 articles and showed that the risk of developing oral mucositis was higher in patients receiving cytarabine and high-dose 5-fluorouracil (47). In the present study, all patients had the same treatment regimen and did not use this drug in their diet, and this accounts for a lower frequency of mucositis in both groups.
Yüce and Yurtsever (2019) examined the effect of education about oral mucositis given to cancer patients having chemotherapy on life quality and found that education can increase the quality of life and improve oral health in cancer patients. Furthermore, the researchers emphasized the role of education in preventing oral mucositis (48). Thailek et al. (2021) explored the impact of a mobile application for enhancing oral care self-efficacy on preventive behavior and occurrence of oral mucositis in school-aged children (7 - 12 years old) with cancer receiving chemotherapy and showed that oral mucositis score in the intervention group was lower than that of the control group on days 7, 14, and 21 of chemotherapy. Although there were some differences between this study and the present study, it can be argued that the use of different training methods can have a positive effect on self-care behaviors even in children (49).
Another review study showed that the use of zinc-containing compounds can play a very important role in the prevention of oral mucositis (50). In the present study, due to the economic and cultural conditions of patients, the use of supplements was not common. However, different studies have indicated that the use of supplements can affect the severity of mucositis. Thus, future studies can address the impact of the use of supplements on the severity of mucositis.
The main objective of the present study was to examine the severity of mucositis in cancer patients in the chemotherapy phase and then in the radiotherapy phase. The data in the present study revealed a small number of oral mucositis in patients. Since oral mucositis is aggravated and even more inflamed by radiotherapy, future studies need to focus more on patients who are undergoing radiotherapy, as was confirmed in the present study. A study examined mucositis incidence, severity, and associated outcomes in patients with head and neck cancer receiving radiotherapy with or without chemotherapy, and the results showed that none of the patients in the chemotherapy group reported mucositis, but 80% of patients with radiation therapy had mucositis from grade I to IV (51). However, the methodology used in this study was different from that of the present study. The participants in the mentioned study were 90 patients with cancer, but the patients were not normalized in terms of factors affecting mucositis because the type of cancer and treatment regimens and the course or stage of treatment could affect the severity of mucositis. In contrast, in the present study, it was attempted to normalize the participants in terms of the severity of mucositis. Thus, a group of patients with the same treatment regimen and treatment phase were included in the study; therefore, the results of the present study could be more accurate than other studies.
This study evaluated oral mucositis in patients in the chemotherapy phase, and the results indicated a small number of oral mucositis in patients. Since oral mucositis is aggravated and even more inflamed by radiotherapy, future studies need to examine this group of patients during expanded follow-up periods.
5.1. Conclusions
The results of the present study revealed that the implementation of the self-care training program promotes oral health and the prevention of oral mucositis. Thus, following these findings and given adverse consequences of mucositis on the treatment of patients, it can be argued that self-care training as a low-cost and simple method can affect the patient’s oral health and prevent oral mucositis.
Following the results of the present study and considering the role of self-care training in the prevention of oral mucositis, similar studies can examine the severity of oral mucositis by type of cancer, especially in patients receiving diets prone to mucositis. The results of the present study indicated that the incidence of mucositis is less likely in patients undergoing chemotherapy. Accordingly, future studies need to focus on patients who are more susceptible and have a higher chance of developing mucositis, such as patients with head and neck malignancies undergoing radiotherapy.