1. Background
An outbreak of a viral disease was reported in Wuhan, China, in December 2019. This disease was caused by a novel and genetically modified virus from the coronavirus family known as severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), which was termed coronavirus disease 2019 (COVID-19) (1). Unfortunately, due to its tremendous transmission capacity, the virus spread quickly over the world, infecting nearly all countries in a short time (less than 4 months) (2, 3). On March 11, 2020, the World Health Organization declared this disease as a pandemic (4). The COVID-19, caused by an RNA virus, affects the majority of individuals’ respiratory systems (5). The most common cause of death in COVID-19 patients is respiratory failure caused by pneumonia (6). As a result, COVID-19 is likely to be more common and severe in individuals with chronic lung disease, and therapies for these patients should be continued as much as possible by telehealth methods, including e-mails or phone calls (5).
Pulmonary fibrosis is frequent following severe acute respiratory syndrome (SARS) and Middle East respiratory syndrome, and the evidence suggests that it can worsen infection with SARS-CoV-2 (7). In SARS patients, pulmonary dysfunction implies the need for progressive rehabilitation from months to years (8). Pulmonary fibrosis is known as a possible outcome among virus survivors and is associated with a significant decrease in quality of life. Old age, disease severity, length of intensive care unit stay and mechanical ventilation, smoking, and chronic alcoholism are all risk factors for pulmonary fibrosis. In the absence of proven targeted treatment for pulmonary fibrosis, steps should be taken to lessen disease severity and protect the lung from further incidental injuries (9). Furthermore, due to the pathogenicity of the virus, this disease might affect the mental health of individuals at various levels of society, including patients, healthcare workers, families, children, students, mentally ill patients, and even staff in various occupations (10-12).
Anxiety and depression are 2 of the most serious psychological crises that can have a detrimental effect on the mental health of patients diagnosed with COVID-19 (13). Previous studies on patients with SARS reported a variety of psychosocial problems, including anxiety and depression (14, 15). In addition, the results of recent studies conducted on COVID-19 showed that patients with COVID-19 might exhibit persistent mental diseases, including anxiety and depression, even after discharge (16-18). Psychological distress and depression can exacerbate the prognosis of COVID-19, impairing the patient’s immunological response, which is associated with loss of smell and taste, and patients with COVID-19 might develop persistent depression even after the beginning of the infectious disease (19, 20).
Pulmonary rehabilitation (PR) is a critical component of managing pulmonary disorders, such as chronic obstructive pulmonary disease (COPD), since it can enhance exercise capacity and physical activity, decrease dyspnea, build muscle strength, improve quality of life, and boost self-efficacy (21). One of the primary goals of rehabilitation is to assist the patient in doing everyday life activities so that the person can meet their basic needs and achieve the maximum possible level of independence to do daily activities (22).
According to the international protocol, PR programs, such as upper and lower limb stretching, improve lung function, arterial blood gases, respiratory muscle strength, dyspnea, and fatigue in patients, while also lowering treatment costs and improving quality of life. Additionally, one of the most critical methods of PR is carrying out respiratory maneuvers, such as pursed-lip breathing and diaphragmatic breathing, which strengthens and improves the function of respiratory muscles, increases arterial oxygen saturation, establishes an effective breathing pattern, and ultimately improves lung function. Respiratory muscles are critical to each individual’s activity process; as an individual’s respiratory capacity increases, the quality and efficiency of his/her activity increase (23). Numerous studies have also demonstrated that various phases of rehabilitation can improve a patient’s quality of life, mental health, depression, and anxiety (24-26).
Nurses play a critical role in achieving this goal because not all patients have access to a formal rehabilitation program. According to Taylor, nursing is a science that focuses on the unique care and needs of each individual via the use of specialized knowledge and skills, education, and research (27). Nurses can play a critical role in teaching the patient and family and supporting special services for patients, such as training breathing exercises, physical therapy for exercise and breathing exercises, and occupational therapy for energy storage strategies during everyday life activities (27).
2. Objectives
Given that health policies place a premium on accelerating client discharge from hospitals, minimizing patient stay in health facilities, and providing care in the community, home-based health services have been viewed as a care solution with characteristics, such as ease of access, low-cost, client acceptance, and family participation (28). Additionally, due to the limited congestion in PR centers due to the prevalence of COVID-19 and the fact that no study has been conducted to date on the effect of home-based pulmonary rehabilitation (HBPR) on anxiety and depression in COVID-19 patients, this study aimed to determine the effect of an HBPR program on anxiety and depression in COVID-19 patients following discharge from hospital.
3. Methods
This randomized clinical trial (IRCT code: IRCT20190702044074N1) was conducted as interventional using simple random sampling. Patients with COVID-19 admitted to Afzalipour Hospital in Kerman, Iran, within August 14 to September 14, 2021, were included in the study. The sample size estimated based mean and standard deviation of anxiety score before and after Respiratory rehabilitation, with α = 0.05, and power = 0.80. Accordingly, 32 participants were required for each group (29). Finally, 38 cases for each group were included to improve study power.
Patients who entered to study had the following inclusion criteria:
The age range of 30 - 65 years, a history of non-invasive mechanical ventilation, no known mental illness or taking drugs that affect the psyche, no drug or smoking addiction, no motor or orthopedic diseases (e.g., trauma and kyphoscoliosis), no chronic diseases (e.g., chronic respiratory disease, kidney disease, thyroid diseases, and cancer), no history of severe physical illness (e.g., pacemaker, right and left heart failure, uncontrolled hypertension, deep venous thrombosis, pulmonary embolism), no history of heart or chest surgery, minimum literacy, and having a caregiver at home.
Additionally, patients should have no history of stressful events, such as the death of first-degree relatives in the past 6 months and during the study, not being a professional athlete, and not be related to the treatment staff members. If the patient had a peripheral oxygen saturation of less than 90% at the time of discharge, hypoxia with little activity, and pulse rate of more than 120 beats per minute, a need to be re-hospitalized, non-compliance with more than 50% of the home training program, and difficulty to make telephone calls after discharge, he/she was excluded from the study.
The information related to demographic data and collected from 5 questions related to patients’ characteristics and the Hospital Anxiety and Depression Scale (HADS), including 14 items, were used. To date, HADS reliability and validity have been confirmed in numerous studies in different countries (29-33). For example, Kaviani et al. reported the validity of the questionnaire with an alpha of 70% and 85% in the depression and anxiety subscales, respectively (29). Additionally, the reliability of this questionnaire has been investigated using the test-retest method in the depression subscale (r = 0.77, P < 0.001) and the anxiety subscale (r = 0.81, P < 0.001) (29).
The HADS was created by Zigmond and Snaith in 1983 and includes 2 scales: Anxiety and depression (34). Of the total questions, 7 are related to anxiety levels and 7 others are related to depression levels. Each question is graded based on the severity of the symptoms from 0 (none) to 3 (severe); on this basis, anxiety and depression are reported in 3 levels: Low (0 - 7); medium (8 - 14); and high (14 - 21) (34). In the present study, the reliability of the tool was calculated at equal to 0.75 using Cronbach’s alpha coefficient.
After selecting the eligible patients and determining the patient group by the researcher, the research questionnaires were given to the patients with providing necessary explanations on how to fill in the research questionnaires in such a way that the HBPR procedures assessed anxiety and depression, once on the first day of discharge and then 4 weeks after discharge from the hospital.
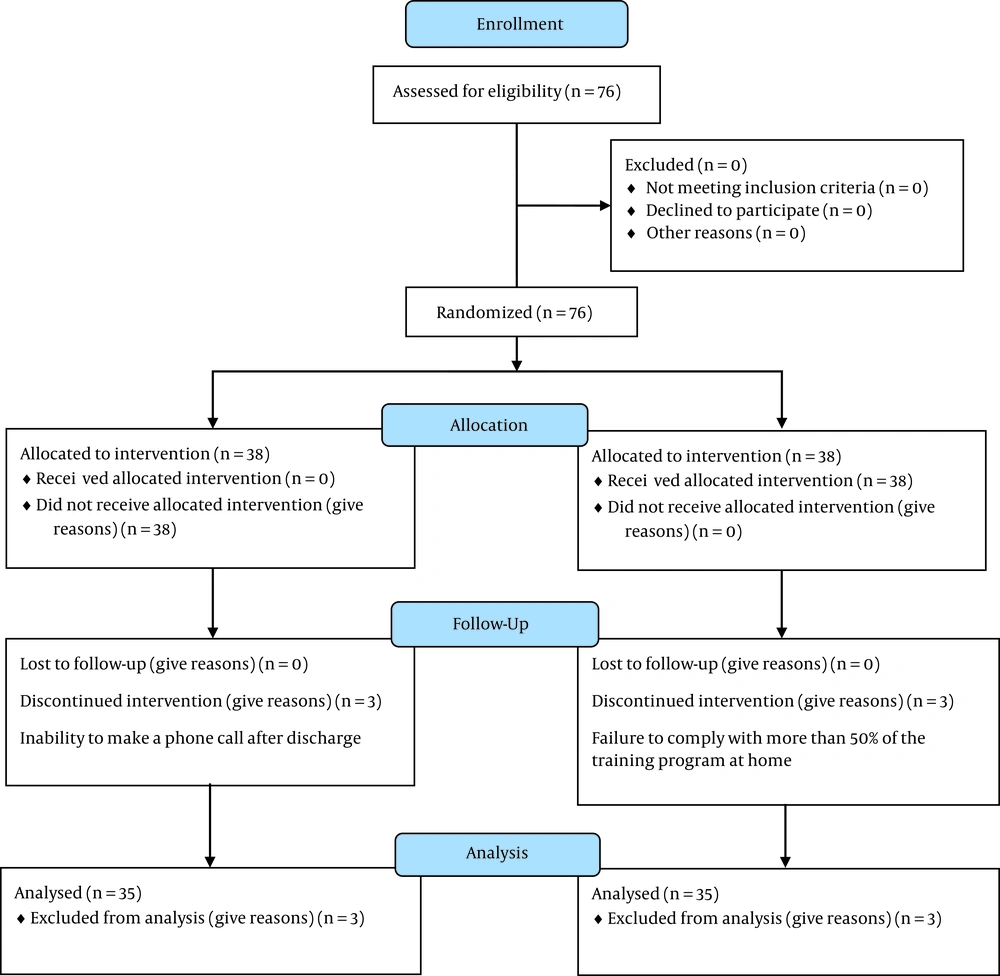
Finally, 70 patients based on inclusion and exclusion criteria were included in the study. These patients were randomly assigned to the intervention and control groups both of which consisted of 38 patients by lottery (color carts). Firstly, the patients in the intervention and control groups received the allocated and routine treatments. Note that, during the study, 3 patients in the intervention group and 3 patients in the control group were excluded due to failure to comply with more than 50% of the training program at home and loss to follow-up, respectively. Finally, 35 patients in each group participated in the analysis (Figure 1).
After discharge from the hospital, the control group patients received only routine post-discharge care that was received in the past; nevertheless, in the intervention group, the patients received PR after discharge. In the intervention group, the HBPR procedure program was provided for the patients as an educational pamphlet designed by the researchers, based on a protocol by John Hopkins University, the United States, with 5 layers (i.e., breathe deep, turn on the vestibular system, cross your body, build strength, and gain endurance) of human movement that repair and optimize the whole individual’s health in the body and mind (35). Moreover, the program was fully explained to the patients after discharge by the researcher. The HBPR program included the first 2 weeks (1 day in between; 1 week on even days, 1 week on odd days, 2 sessions every day, and each session for 10 minutes) and the second 2 weeks (1 day in between; 1 week on even days, 1 week on odd days, 2 sessions every day, and each session for 15 minutes), which lasts 4 weeks in total; however, the patients in the control group received routine care.
All of the ethical codes of research in medical sciences throughout the study were considered. The median and interquartile range for continuous data (i.e., age, duration of hospitalization, and anxiety and depression scores) and numbers and percentages for nominal and categorical data (i.e., gender, marital status, educational level, and anxiety and depression status) are reported. The chi-square and Fisher’s exact tests were used to compare gender, marital status, educational level, and anxiety and depression status between the intervention and control groups. The Shapiro-Wilk test was used to test the normality of continuous variables. As the distributions of these variables were not normal, the Mann-Whitney U test was used to compare age, duration of hospitalization, and anxiety and depression scores between the 2 groups. At the end of the study, P < 0.05 was considered statistically significant.
4. Results
There was no statistically significant difference between the intervention and control groups regarding gender, age, marital status, educational status, duration of hospitalization, and the severity of hospital anxiety and depression (instantly after discharge) (Table 1).
| Variables | Intervention (n = 35) | Control (n = 35) | P-Value |
|---|---|---|---|
| Gender | |||
| Male | 19 (54.3) | 19 (54.3) | 1 b |
| Female | 16 (45.7) | 16 (45.7) | |
| Marital status | |||
| Single | 6 (17.1) | 4 (11.4) | 0.46 c |
| Married | 28 (80.0) | 31 (88.6) | |
| Divorced | 1 (2.9) | 0 | |
| Age (y) | 44 (39 - 51) | 43 (39 - 53) | 0.98 d |
| Educational level | |||
| Primary school or lower | 3 (8.6) | 4 (11.4) | 0.92 c |
| Middle school | 3 (8.6) | 3 (8.6) | |
| High school and above | 29 (82.8) | 28 (80.0) | |
| Duration of hospitalization | 10 (8 - 10) | 10 (8 - 12) | 0.30 d |
| Anxiety | |||
| Low | 0 | 0 | 0.14 b |
| Moderate | 18 (51.4) | 12 (34.3) | |
| High | 17 (48.6) | 23 (65.7) | |
| Depression | |||
| Low | 0 | 1 (2.9) | 0.33 c |
| Moderate | 22 (62.9) | 17 (48.6) | |
| High | 13 (37.1) | 17 (48.6) | |
| Anxiety | 14 (11 - 16) | 15 (13 - 17) | 0.44 d |
| Depression | 14 (11 - 15) | 14 (13 - 16) | 0.35 d |
Baseline Demographic and Clinical Characteristics by the Group at the Time of Discharge a
The outcome of this clinical trial was the severity of anxiety and depression 4 weeks after discharge. After this timeline and following the HBPR program, the anxiety severity levels in patients in the intervention group (82.9%, 17.1%, and 0% with low, moderate, and severe anxiety, respectively) were significantly lower than in the control group (20%, 71.4%, and 8.6% with low, moderate, and severe anxiety, respectively). Four weeks after discharge, the depression score in patients in the intervention group (80%, 20%, and 0% with low, moderate, and severe depression, respectively) were significantly lower than in the control group (11.4%, 74.3%, and 14.3% with low, moderate, and severe depression, respectively) (Table 2).
| Variables | Intervention (n = 35) | Control (n = 35) | Test Statistic | P-Value |
|---|---|---|---|---|
| Anxiety | χ2 = 28.1 | |||
| Low | 29 (82.9) | 7 (20.0) | < 0.001 b | |
| Moderate | 6 (17.1) | 25 (71.4) | ||
| High | 0 | 3 (8.6) | ||
| Depression | χ2 = 33.9 | |||
| Low | 28 (80.0) | 4 (11.4) | < 0.001 b | |
| Moderate | 7 (20.0) | 26 (74.3) | ||
| High | 0 | 5 (14.3) | ||
| Anxiety | 5 (4 - 7) | 14 (13 - 16) | Z = 5.7 | < 0.001 c |
| Depression | 6 (5 - 7) | 10 (9 - 13) | Z = 6.1 | < 0.001 c |
Comparison of Severity and Median Scores of Hospital Anxiety and Depression Between Intervention and Control Groups After 4-Week Pulmonary Rehabilitation a
In addition, after 4 weeks of discharge, the median anxiety score in the intervention group was significantly lower than in the control group (5 vs. 14, P < 0.001), and the median depression score in the intervention group was significantly lower than in the control group (6 vs. 10, P < 0.001).
5. Discussion
The anxiety and depression score after 4 weeks of PR in the intervention group was significantly lower than in the control group. Liu et al. in 2022 studied a group psychological protocol that was combined with PR programs in the trial group for patients with mild COVID-19 patients (36). The results showed that both anxiety and Pittsburgh sleep quality scores of the intervention group were significantly lower than the control group (36). The results of the current study also demonstrated that anxiety scores improved after patient discharge from the hospital with an HBPR program; however, no psychological protocol was followed in the present study. The study by Liu et al. in 2020 on PR in elderly patients with COVID-19 showed that after 6 weeks of PR in these patients, the anxiety and depression scores were improved (37). Therefore, it can be concluded from this study that PR improves COVID-19 side effects in elderly patients (37). The results of the present study also indicated that the severity of hospital anxiety and depression improved after 4 weeks of rehabilitation, which is in line with the results of the aforementioned study, except that the rehabilitation program in the present study is home-based and easy to access.
In a study by Kerling et al., 42 depressed inpatients were randomly divided into a 6-week structured and supervised exercise intervention and treatment as usual or treatment as usual lonely (38). Their results demonstrated that through appropriate physical activity, the release of neurotransmitters and the functions of the reticular formation are regulated to keep patients happy and promote their mental health (38). The results of the aforementioned study are in line with the results of the present study; accordingly, HBPR was beneficial to the nervous system of patients with COVID-19 and reduced the severity of hospital anxiety and depression. According to Kerling et al.’s investigation, which mentions the release of neurotransmitters and the effect on the nervous system due to exercise as the causes of improvement, it can be concluded that the rehabilitation program of the present study can also improve anxiety; however, the findings of the current study confirm the above-mentioned statement (38). The present study used an HBPR program after the discharge of COVID-19 patients from the hospital, and to the best of our knowledge, the current study is the first one of its kind.
Previous studies demonstrated the benefits of home-based programs, including HBPR, to patients’ recoveries similar to those in hospitals (39-41). Considering the COVID-19 pandemic situation, these out-of-hospital programs seem helpful and are advised (42). The HBPR studies’ benefits especially on HADS are proven previously in COPD patients (43-45). For example, a study by Vilarinho et al. demonstrated that some pulmonary parameters plus HADS scores were improved after HBPR in 30 patients with severe COPD (46). Additionally, Wallaert et al. studied HBPR in 112 patients with idiopathic pulmonary fibrosis and fibrotic nonspecific interstitial pneumonitis (47). Their results showed that the 2-month PR improves HADS score and quality of life (47). Although in terms of the duration of the intervention, their intervention was longer than the present study, it confirms the results of the present study and is consistent with the results of the present study.
The strength of the current study is that this HBPR program occurs at home, which is applicable to everyone in almost any condition. It can be said that the use of this strategic method is effective in developing the principle of justice-oriented to provide health services to all individuals. Furthermore, the presence of individuals in public is reduced and can help reduce the pandemic spread.
5.1. Conclusions
The current study showed that HBPR is effective in reducing the severity of anxiety and depression after discharge. However, these results show that an HBPR program can be used as a safe and efficient recovery plan for patients with COVID-19 at home, which reduces patient resort to health centers.
5.2. Study Limitations
In this study, there was a possibility that the treatment plan could not be fully controlled before and during the operation and it might affect the results, which can lead to problems and bias in the study. Therefore, the present study produced an educational pamphlet for patients, and the program was fully explained to the patients after discharge by the researcher to avoid misunderstanding. Additionally, the mobile number of the researcher was given to the patients for better communication.