1. Background
The new coronavirus pandemic spread rapidly worldwide, and based on the WHO's official figures on March 8, 2021, more than 113 million people were infected with the disease worldwide, and the death toll exceeded 2.5 million. Iran's share of these statistics is more than 1.8 million infections and more than 62,000 deaths (1). However, new waves of the disease started with a higher prevalence and severity of pathogenesis in many countries, including Iran. COVID-19 is an infectious disease with high transmissibility (2). Hence, measures should be taken to prevent the transmission of infection (3). Even though most people with COVID-19 experience mild to moderate respiratory illness and recover without any special treatment, the elderly and people with background diseases are more likely to have severe types of the disease (4) and require special care at hospitals. Therefore, hospitals face an influx of critical patients and a lack of specialized staff in inpatient and ICU departments. Thus, they must enlist personnel from other departments to provide the least care to patients infected by COVID-19 (5-7). Due to the elimination of elective surgeries and the reduced workload of operating room departments, their staff are sent to inpatients wards for care of patients with COVID-19 (8). However, many do not have enough self-protecting knowledge and experience to deliver extensive care to patients under mechanical ventilation (9). Undoubtedly, observing personal protection without necessary facilities and equipment is impossible. At the beginning of the crisis, hospital managers were involved with insufficient personal protective equipment (PPE). Hence, a large number of nurses and physicians died of this infection in different countries (5, 10). Therefore, hospital managers need to re-design a specific strategy for managing financial, human, and equipment resources to provide optimal care to patients and staff during crises (3, 11). It is a fact that human resources in operating room departments are essential at the time of crisis, as they are frequently sent to other departments to help physicians and nurses with performing procedures such as intravenous therapy. Nevertheless, retaining human resources is crucial in health care, and hospital managers are responsible for protecting the operating room team members and other staff by developing detailed instructions in each field and education for facing crises (12-14). Undoubtedly, the resilience of hospitals to pandemics or epidemics is not the same and depends on the readiness of medical centers in crisis management. Health care providers, such as physicians, nurses, and health care team members, are less susceptible to burnout if hospitals are better prepared to deal with crises through proper planning and policy-making (15, 16).
2. Objectives
Accessing the first-hand information and real experience of staff at hospitals about the COVID-19 crisis through interviews yield valuable findings that can be used to determine management strategies and formulate executive guidelines for managing COVID-19 and similar crises. Therefore, the present study was conducted to qualitatively investigate surgical technologists' work experiences during the COVID-19 disaster.
3. Methods
3.1. Study Design
The present qualitative study was carried out after receiving the code of ethics from Alborz University of Medical Sciences (IR.ABZUMS.REC.1399.058).
3.2. Participants and Setting
This study was conducted from September 2020 to February 2021 at Alborz University of Sciences. We selected 42 surgical technologists using the purposive sampling method. The inclusion criteria were at least six months of work experience in providing care to COVID-19 patients in the operating room and other inpatients wards and willingness to share experiences with the researcher. The candidates were invited to participate in the study through WhatsApp. Consent forms were obtained from those who voluntarily participated in the study.
3.3. Data Collection
The semi-structured interviews were conducted online through WhatsApp due to restrictions on face-to-face communication. The interviews lasted between 35 - 60 min.
The semi-structured interview form included the following questions:
• How do you evaluate working in the operating room during the COVID-19 crisis?
• How was working in a crisis different from the previous routine situation?
• What problems did you have in the hospital?
• What did you consider as a relief in other departments?
• Did you encounter a shortage of equipment, and if so, how did you manage it?
• In your opinion, how can one efficiently manage a crisis in similar cases?
Motivational or probing questions were asked via WhatsApp depending on the cases after reading the participants' answers to deepen the interviews. The responses were then added to the text of their previous interviews. The questions were as follows:
• Can you tell me a little more about what you wrote?
• Can you give an objective example for the text you have written?
• Can you tell me how you felt about the experience you wrote about here?
Data collection continued until data saturation was achieved and no new data was obtained (Interview 42). Three interviews were repeated to confirm data accuracy.
3.4. Data Analysis
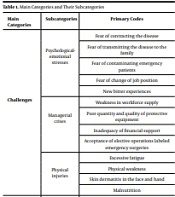
The data was analyzed using the steps proposed by Zhang and Wildemuth via content analysis (17). First, the researcher read each interview transcript several times to gain familiarity with the data and develop a preliminary understanding of the related concepts. The codes were compiled to form categories and subcategories using continuous comparison, evaluation, feedback, and interpretation. MAXQ-DA10 software was used to manage the data. After analyzing the last interview, no new code was extracted, no new category was created, and the data was saturated. Finally, 135 primary codes, six subcategories, and two main categories were extracted. Main categories, subcategories and examples of primary codes are shown in Table 1.
| Main Categories | Subcategories | Primary Codes |
|---|---|---|
| Challenges | Psychological-emotional stresses | Fear of contracting the disease |
| Fear of transmitting the disease to the family | ||
| Fear of contaminating emergency patients | ||
| Fear of change of job position | ||
| New bitter experiences | ||
| Managerial crises | Weakness in workforce supply | |
| Poor quantity and quality of protective equipment | ||
| Inadequacy of financial support | ||
| Acceptance of elective operations labeled emergency surgeries | ||
| Physical injuries | Excessive fatigue | |
| Physical weakness | ||
| Skin dermatitis in the face and hand | ||
| Malnutrition | ||
| Coping strategies | Emotion-based strategies | Adaptation with trust in God |
| Acceptance of the situation | ||
| Development of the spirituality | ||
| Cognition-based strategies | Changes of beliefs and attitudes | |
| Adapting to a new situation | ||
| Problem-based strategies | Following the guidelines | |
| Innovation and creativity | ||
| Change of lifestyle | ||
| Creating new communication channels |
3.5. Rigor
To strengthen the data, the researchers used Guba and Lincoln's criteria of credibility, transferability, dependability, and conformability (18). The credibility was promoted by prolonged engagement with participants and contact with them for a long time. During the study, the interview transcripts and the extracted codes were sent to the participants to ensure they were consistent with the participants’ experiences. Furthermore, maximum diversity was considered (age, sex, workplace, city, work experience, and history of infection with COVID-19) to enrich the information. Also, dependability and conformability were determined through a review of the data and peer code review in the data gathering process. Regarding transferability, the characteristics of the participants and the study process were described clearly and accurately so that other researchers could use them.
4. Results
Among the 42 participants in the study, 19 were male, and 23 were female. Other findings related to the individual and professional characteristics of the participants are presented in Table 2.
| Parameters | Average/No. (%) |
|---|---|
| Age | 32.88 |
| Work experience | 10.13 |
| History of infection with COVID-19 | 17 (40.5) |
| Sex | |
| Female | 23 (54.8) |
| Male | 19 (45.2) |
The technologists’ work experiences during the COVID-19 pandemic were investigated using qualitative content analysis, and the results were classified into two main categories, "challenges" and "coping strategies." The following section describes the main categories and their subcategories (Table 1).
4.1. Challenges
This category consists of three subcategories, "psychological-emotional stresses," "managerial crises," and "physical injuries," as described below.
4.1.1. Psychological-Emotional Stresses
Due to the cancellation of the acceptance of elective surgeries, the reduction of surgeries, and the crisis of shortage of specialized human resources in the COVID-19 wards, the surgical technologists were sent to other wards as relief workers. As the result of communication with staff in the wards, unfamiliarity with the physical location of the care equipment, and ignorance of the nursing care of patients, the majority of the participants described their transfer to new posts as a bitter experience.
"I felt lonely in the new department." (Participant 4)
"I did not know what to do in the ward where I was sent. I did not know where the equipment was. The staff was too busy, and I felt very bad. I was also stressed that I would get sick there, and thought that I was not useful and I could not help them." (Participant 15)
Due to the fear of contaminating emergency patients in the operating room, fear of transmitting the disease to the family, fear of contracting the disease, and feeling of rejection by family members, the surgical technologists constantly experienced emotional and psychological feelings that could affect their mental health.
"My spouse is no longer sleeping in the same room with me for fear of getting infected, and has completely separated oneself from my room." (Participant 13)
"I deeply want to hug and kiss my child." (Participant 7)
4.1.2. Managerial Crises
The data analysis indicated that "weakness in workforce supply," "poor quantity and quality of protective equipment," "inadequacy of financial support," and "acceptance of elective operations labeled emergency surgeries" were common codes from which the subcategory was derived.
Weakness in workforce supply was the main problem for the surgical technologists during this period. The absence of the employees and asking for sick leave, going for home quarantine, or hospitalization led to a shortage of specialized staff in the operating room. Thus, the remaining staff had to cover the shifts of those failing to attend work due to sickness.
"In such crises, I think it is very important to manage the work schedule among colleagues, for instance, some employees went off for rest and the others endured their workload. I think we should plan in such a way to get more manpower, pay higher, and thus motivate staff to work in this period." (Participant 23)
The lack of high-quality PPE was another crisis for the surgical technologists during the admission of COVID-19 patients. Due to the lack of such equipment in hospitals and medical centers, all the equipment was given to those working in emergency departments, intensive units, and inpatient wards for COVID-19 patients. In the operating room, only anesthesia staff received special protection kits in case of suspected COVID-19 patients; however, many admitted patients undergoing surgery were diagnosed with the infection after the operation.
"We did not have any protective equipment. We had to work with a mask during morning and evening shifts. We knew it was not fair, but we had no choice. Everything was poor and low quality." (Participant 19)
Working in such a situation is very difficult and requires strengthening managerial motivation. Psychological and financial support can play a valuable role in maintaining and strengthening staff wellbeing and resilience. However, due to the low presence of officials in inpatient wards and very low payments to employees compared to the workload imposed on them in some centers, they are dissatisfied with the management of units.
"The managers must first separate the wards and mostly handle the personnel in the COVID-19 wards, either in terms of salaries or nutrition; it is useless to say what a pity after making the personnel sick." (Participant 17)
Another issue reported by some of the participants was the admission of elective patients as emergency patients that increasingly exposed the surgical technologists to suspected cases of COVID-19 and worried them. Unfortunately, the management of hospitals was either unaware of this issue or ignored it to gain financial profits.
"After a few years, we can recognize that this operation by Dr. X is not an emergency, but what we can do when the management is also behind the surgeons. It's not fair that a lot of people are at risk of death." (Participant 2)
4.1.3. Physical Injuries
Physical injury was the last subcategory of the challenges category, dealt with by the surgical technologists. Excessive fatigue due to long shifts, physical weakness due to contracting the disease, lack of proper nutrition due to the nature of the protective cover of the body in the COVID-19 wards, fear of food contamination, skin damage on the face, sweating, skin dermatitis in various parts of the body, and dermatitis caused by frequent hand washing with disinfectants were frequently mentioned by the participants.
"Our clothes were terribly hot, the shields were bothering our faces and noses, and we did not dare to pick them up or throw them away for fear. We washed our hands too much, and got urticarial." (Participant 6)
"You cannot either eat anything or drink a little water for long hours, we have no power and are so tired." (Participant 14)
4.2. Coping Strategies
This category includes three subcategories, namely "emotion-based strategy," "cognition-based strategy," and "problem-based strategy."
4.2.1. Emotion-based Strategy
In the present study, the participants had to deal with the situation in different ways during the COVID-19 period. Some relied more on God and understood the greatness of the power of the Lord in creating a small creature that challenged human life; thus, they adapted to the existing conditions and surrendered. Some of the young surgical technologists covered for their colleagues who were at risk to keep them safe with a spirit of self-sacrifice.
"I realized that humans are not so powerful and a virus can make humans helplessness, and it allowed all creatures to live freely without the disturbance of humans." (Participant 19)
"Well, when you are young, you can go forward, be less worried about diseases, so I was nominated several times for working instead of my colleagues as they were older and someone was sick. It is not fair to be infected." (Participant 27)
4.2.2. Cognition-based Strategy
Some of the participants mentally lost their fear and accepted the situation over time. Changing their personal beliefs and attitudes, a group of participants forced themselves to adhere to hygiene principles, which sometimes turned into an obsession.
"In the early days, most employees were impatient and skeptical, but the situation gradually got better." (Participant 9)
"Some employees were so obsessed with hygiene and became obsessed. They were constantly linking everything to the coronavirus." (Participant 12)
"I gradually realized that these conditions persist, and I must try to get back to everyday life." (Participant 40)
"It was difficult, but as our awareness increased, we tried to obey personal protection rules as much as we could and reconcile with life." (Participant 42)
4.2.3. Problem-based Strategy
During this period, some personnel made innovations and initiatives to maintain their physical and mental health. For instance, they used accessible items such as garbage bags as covers for clothes and shoes, made shields, and sewed masks with whatever was available. They also tried to improve their communication with other staff in inpatient departments and provide a condition to live in a separate place to avoid any contact with other family members,
"We used alternative equipment to work with COVID-19 patients. For example, in the early days, when we did not have any special clothing, we used cloth scrubs, which we sterilized, or two ordinary masks instead of COVID-19 clothing, and we also prepared some shields ourselves, but with difficulty." (Participant 18)
These personnel pioneered solving the communication problem with the personnel of other departments and patients by trying to communicate with them and establishing an effective empathic relationship with patients as a new experience. Their emotions grew, and their sense of fulfilling the patient's needs led to greater endurance and motivation to cooperate.
"In the coronavirus ward, I tried to be very welcoming to the patients, and be kind to them, and it was my morals that influenced other colleagues who were on shifts with me, and the patient's prayers were with us." (Participant 10)
They included the issuance of instructions and guidelines about changes in care programs and direct admission of patients and recovery by the anesthesia team in the operating room, restriction of staff movement, and the prohibition of gathering in the restroom.
"After a long, they insisted that patients should go directly to the ward from the operating room, and the surgical technologist should not go to the operating room until the patient was anesthetized, so we could partially control the situation." (Participant 7)
They learned to return home with some lifestyle changes and live with family members.
"I try to prepare an isolated room to separate myself from
my family." (Participant 38)
5. Discussion
The results of this qualitative content analysis about investigating surgical technologists' work experience during the coronavirus were categorized into two main categories, "challenges" and "coping strategies."
"Psycho-emotional stress" was the first challenge for the employees in this period and was created due to new conditions and situations, fear of contracting and transmitting the disease, and feeling of rejection. Zhu et al. also found that health providers at the forefront of battling against the COVID-19 pandemic had high symptoms of anxiety and depression (19). In another study, medical staff in direct contact with COVID-19 patients were more anxious than other staff (20). In a similar qualitative study examining nurses' experiences of caring for MERS-COV patients in South Korea, a challenge expressed by nurses under severe stress during this period was the bitter experience of being forced to go to infectious wards due to the lack of labor and fear of becoming sick (21), which is consistent with the present study’s results. Managerial inefficiency was another challenge for operating room nurses during the COVID-19 crisis, and it was related to poor management in the provision of professional workforce, poor quantity and quality of PPE, lack of psychological and financial support of staff involved in caring for patients with COVID-19, and not monitoring the admission of elective patients regarded as emergency patients. Koh et al. conducted a systematic study and emphasized the importance of providing PPE, adequate training, and personal support to protect health care workers during an epidemic (22). Catton also believes that nursing managers must provide supportive policies and a safe workplace for the mental and emotional health of nurses working in different departments in dealing with the fear of the COVID-19 pandemic (23). Based on Zamanzadeh and colleagues' study, the non-standard design and lack of PPE lead to difficulty in delivering optimal nursing care in the COVID-19 crisis (24). The above results are consistent with the present study’s findings. Therefore, examining management crises from the perspective of hospital staff in different wards may help reduce problems and increase their motivation. Physical injury was the last subcategory of the challenges category. In a similar study, nurses reported that their physical power decreased due to the use of poor PPE, caring for patients with special conditions, stress, and continuous disinfection and cleaning of rooms since working during the MERS-COV epidemic (21). In a study by Kang et al., participants experienced high burnout due to the high workload during the outbreak of Middle East Respiratory Syndrome (MERS) (25). Therefore, it is necessary to adopt appropriate strategies to reduce this fatigue.
The "coping strategies" category was the second category in the present study. The "emotion-based strategy" was a coping strategy chosen by the surgical technologists. Some of the technologists adapted to the existing conditions to some extent by relying on God, and others by self-sacrifice and conscientiousness. In a study by Kim, higher friendship and cooperation, encouragement from the public, and higher experience and pride in the nursing profession were some of the coping strategies for South Korean nurses during the MERS-COV epidemic (21). The cognition-based strategy was another coping strategy undertaken by a group of surgical technologists. Some of them accepted the situation over time, but others developed obsessive-compulsive disorder and severe anxiety. Similarly, Lee et al. reported the effects of positive or negative adjustment due to anxiety and fear of COVID-19 (26). This result is consistent with the results of a study by Niuniu Sun, who investigated the theme of growth under pressure and reported cases of maturity in individuals who grew personally and professionally by solving the problem of environmental pressure (27).
The problem-based strategy was the last subcategory extracted from the "coping strategies" category. Nurses sought to solve problems by taking measures such as reducing face-to-face visits and family parties, transferring family members, residing in separate places, using alternative available protective equipment, and direct discharge of patients from the operating table to wards. Ahmadidarrehsima and colleagues reported that nurses in COVID-19 wards in Iran used problem-solving strategies, similar to this study's result (28).
5.1. Conclusions
The surgical technologists' experience indicated that the COVID-19 crisis, especially on the first days, posed serious challenges, most of which were related to the shortage of protective facilities and the lack of adequate training about self-care and patient-care in wards where they had no work experience. Therefore, managers of medical centers need to offer appropriate purposive training courses to sufficiently develop their staff's knowledge and competence to manage the crisis in pandemics or epidemics. Also, health system policymakers need to establish a secure health care system by predicting possible crises and providing adequate human resources, funding, and equipment.
5.2. Limitations
Travel restrictions and Quarantine condition at the height of the Covid-19 crisis and the dispersion of the study population in the country level, leaded to impossibility for face to face interviews. So, the interviews was only administered via WhatsApp.