1. Background
Birth injuries are those occurred during the birth process, which includes labor and delivery. They may be avoidable or unavoidable. Birth injuries are still among the major causes of neonatal morbidity in neonates hospitalized in neonatal intensive care units (NICUs). There are some concerns about the severe intracranial injuries following assisted vaginal deliveries and unsuccessful attempts made in these deliveries (1). Different types of birth injuries include; injuries to soft tissue, injuries to head and face, to the neck, shoulder girdle and chest, injuries to spine and spinal cord, injuries to abdominal organs, injuries to extremities and genitalia. The overall prevalence of birth injuries has decreased due to the advances in the field of birth care and prenatal diagnosis. Reports suggest that the prevalence of birth injuries is approximately 2% per vaginal delivery in the cephalic fetal position and approximately 1.1% in cesarean section (C-section) births (2, 3). In 1981, birth injuries were the sixth cause of neonatal mortality, and yet they have become the eleventh cause of neonatal mortality due to the improvements in obstetric methods and the increase in C-section cases (4). The most prevalent type of birth injury is soft tissue injuries, including bruises, petechiae, subcutaneous fat necrosis, and lacerations (5). The predisposing factors of birth injuries are as follows: neonates that are large for the gestational age (especially infants with weights exceeding 4,500 grams) (6), assisted deliveries (especially deliveries assisted by forceps or vacuums), vaginal deliveries with a breech presentation, and excessive or abnormal stretching at the time of labor (1).
In this regard, Mondal et al. carried out a study at Hindu Rao Hospital in New Delhi for 8 months (March to October 2014) to analyze all neonates for birth injuries. Of the 4,741 live births, 73 cases of birth injuries were recorded, with a prevalence of 15.4 per 1,000. The most common injuries were soft tissue injuries, as well as skull and scalp injuries. The related risk factors included older maternal age, shorter maternal height, higher birth weight, assisted delivery, non-cephalic presentation, and prolonged labor (7).
In a study in the northeast of Nigeria, Pius et al. explored the prevalence of birth injuries in this region. In this study, the prevalence of birth injuries was 5.7 per 1,000 live births, and soft tissue injuries were the most common types of injuries. Subconjunctival hemorrhage, birth asphyxia, central nervous system (CNS) injuries, and brachial plexus paralysis also had the next ranks prevalence-wise (8).
Abedzadeh-Kalahroudi et al. examined the prevalence and factors of birth injuries in Kashan. In their study, the prevalence of birth injuries was 2.2%: 3.6% in vaginal deliveries and 1.2% in C-section cases. The most common injury was cephalohematoma, followed by asphyxia. In a logistic analysis, fetal heart rate drop, fundal pressure, shoulder dystocia, vaginal delivery, male sex, infant weight, delivery by a resident, induction of labor, and labor in a teaching hospital were considered predictors of birth injuries (9).
Rezaie et al. conducted a study on 2,005 infants born at Imam Sajad Hospital in Yasuj City and stated that the prevalence of birth injuries was 10.8% in vaginal births and 3.7% in C-section cases. The most prevalent injuries were caput succedaneum, subconjunctival hemorrhage, cephalohematoma, erythema, and facial scratches, while the risk factors were difficult vaginal delivery, high fetal age, low 1-minute Apgar score, night shift of maternity ward personnel, use of vacuum, and shoulder dystocia (10).
The other injuries included clavicle fracture, brachial plexus paralysis, crushed face, brain hemorrhage, and skin hematoma. In their study, the prevalence of birth injuries was 41.16 per 1,000 live births. The risk factors of birth injuries in this study were the induction of labor, premature rupture of membranes, academic degree of the doctor conducting the delivery, higher weight, and delivery age (11).
2. Objectives
Due to a lack of research on the prevalence of birth injuries and their related risk factors in Fatemieh Hospital and considering it as the only third-level referral center providing perinatal and neonatal care in Hamadan Province (wherein up to 5,000 to 6,000 births take place annually) and based on mentioned studies, thus identifying these complications, long-term planning of caregiver skills training can be done. This study was carried out to identify the prevalence of birth injuries and its determining factors at Hamadan Fatemieh Hospital (2020 - 2021).
3. Methods
In this case- control study, included all live births at Hamadan Fatemieh Hospital from October 2020 to October 2021 were examined on the first day of birth by pediatricians and neonatologists working in this center. In the case of detecting any birth injury, the cases were categorized by injury type and recorded on a checklist form included demographic data of mother, data of pregnancy and child birth along with the risk factors. An equal number of neonates with no birth injuries were also examined for the same risk factors. The census method was used, and from total of 5,592 births, all 66 cases with birth injuries were included as case group. Moreover, 65 neonates without birth injuries were enrolled and matched (age, birth weight, sex, Apgar score, fetal age) in the control group. The inclusion criterion included all live births during the study course, while no exclusion criterion was set.
To describe and report quantitative variables with normal distribution Shapiro-Wilk test showed that the distribution of quantitative variables are normal), the mean and SD were used, while the median and interquartile range were used for non-normal variables. As for the qualitative variables, number and percentages were used. To compare two groups of quantitative data (with birth injury and without birth injury), an independent t-test was used with normal data distribution, and the Mann-Whitney test was used with non-normal data distribution. To compare two groups of qualitative data, a chi-square test was used, and data frequency distribution was used to determine the birth injury frequency. The statistically significant level was 5%, and data analysis was performed using SPSS version 16 (SPSS Inc., Chicago, Ill, USA).
4. Results
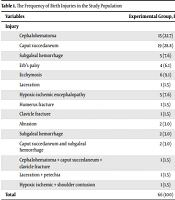
During the study, a total of 66 birth injuries were recorded among 5,592 birth (prevalence rate 11.8 per 1,000 live births). Besides, 131 participants were studied: 66 with birth injuries (case group) and 65 without birth injuries (control group). The most prevalent birth injuries were caput succedaneum (28.8%) and cephalohematoma (22.7%; Table 1).
| Variables | Experimental Group, Frequency (%) | Accumulative Percentage |
|---|---|---|
| Injury | ||
| Cephalohematoma | 15 (22.7) | 22.7 |
| Caput succedaneum | 19 (28.8) | 51.5 |
| Subgaleal hemorrhage | 5 (7.6) | 59.1 |
| Erb’s palsy | 4 (6.1) | 65.2 |
| Ecchymosis | 6 (9.1) | 74.2 |
| Laceration | 1 (1.5) | 75.8 |
| Hypoxic-ischemic encephalopathy | 5 (7.6) | 83.3 |
| Humerus fracture | 1 (1.5) | 84.8 |
| Clavicle fracture | 1 (1.5) | 86.3 |
| Abrasion | 2 (3.0) | 89.3 |
| Subgaleal hemorrhage | 2 (3.0) | 92.4 |
| Caput succedaneum and subgaleal hemorrhage | 2 (3.0) | 95.5 |
| Cephalohematoma + caput succedaneum + clavicle fracture | 1 (1.5) | 97 |
| Laceration + petechia | 1 (1.5) | 98.5 |
| Hypoxic ischemic + shoulder contusion | 1 (1.5) | 100 |
| Total | 66 (100) |
The findings revealed that the relationship of birth injuries with gestational age, birth rank, and Apgar score was statistically significant (P-value < 0.05), whereas its relationship with maternal age was insignificant with independent t-test (P-value > 0.05) (Table 2).
| Variables | Mean ± SD | P-Value, t-Test | |
|---|---|---|---|
| Experimental | Control | ||
| Gestational age | 37.106 ± 5.90033 | 38.813 ± 1.5560 | 0.034 |
| 1-minute Apgar | 7.919 ± 1.83141 | 8.703 ± 1.00285 | 0.001 |
| 5-minute Apgar | 2.229 ± 1.24356 | 9.781 ± 0.62915 | 0.002 |
| Maternal age | 27.322 ± 6.78599 | 29.468 ± 7.00560 | 0.087 |
| Birth rank | 1.907 ± 1.01440 | 2.854 ± 1.32192 | 0.004 |
There was a statistically significant relationship between birth injuries and delivery type, as well as birth injuries and the cause of delivery (P-value < 0.05) (Table 3).
| Variable | Group, No. (%) | Total | P-Value | |
|---|---|---|---|---|
| Experimental | Control | |||
| Type of delivery | 0.006 | |||
| C-section | 17 (25.8) | 31 (49.2) | 48 (37.2) | |
| Vaginal | 49 (74.2) | 32 (50.8) | 81 (62.8) | |
| Responsible person for delivery | 0.001 | |||
| Midwife | 20 (28.2) | 51 (71.8) | 71 (100) | |
| Assistant gynecologist | 38 (73.1) | 14 (26.9) | 52 (100) | |
| Gynecologist | 4 (100) | 0 (0) | 4 (100) | |
| Midwife + gynecologist | 1 (100) | 0 (0) | 1 (100) | |
a Chi-square test.
There was no significant relationship between birth injuries and neonate gender, birth weight, non-cephalic presentation, abnormalities, underlying maternal diseases (diabetes, hypertension, preeclampsia, and other factors); (P-value > 0.05).
5. Discussion
This study aimed to determine the prevalence of birth injury and its determinants at Hamadan Fatemieh Hospital within a year. During the study, a total of 5,592 births took place, and 66 cases of birth injury were recorded, while the prevalence of birth injuries was 11.8 per 1,000 live births. Different statistics have been reported in studies worldwide. However, the overall prevalence of birth injuries has definitely decreased over time, and thus lower statistics have been reported in studies conducted in recent years. In India, Mondal et al. showed that the prevalence of birth injuries at a hospital was 15.4 per 1,000 (7), and in the USA, Sauber-Schatz et al. showed that it was 29 per 1,000 (12). Also, in Pakistan, Shabbir and Zahid, in a study from 2010 to 2012, indicated that the prevalence was 41.16 per 1,000 vaginal births (13). In Nigeria, Pius et al. reported that the prevalence was 5.7 per 1,000 (8). Some causes of difference in prevalence may be included: Different sample sizes, different strategies for C/S, educational medical center (experience of the person who is responsible of labor).
Among the similar studies conducted in Iran, Rezaie et al. performed a cross-sectional study within a year and showed that the prevalence of birth injuries in Yasuj was 10.8% in vaginal births (10), while Borna et al. carried out a 3-year study at Imam Khomeini Hospital in Tehran and reported a rate of 41.16 per 1,000 live vaginal births (11). In Finland, Kekki et al. conducted a study in which the prevalence of birth injuries in all births from 1997 to 2017 was investigated through the registry system, and the prevalence of birth injuries decreased from 34 to 16.6 per 1,000 live births (14). In a study conducted over a period of 2 years in the NICU of a third-level center at Bijapur Hospital in India, 100 of 850 hospitalized neonates (11.76%) suffered birth injuries (15). In a study in Ghana, 5,590 neonates hospitalized in the NICU of a third-level teaching hospital from January 2018 to December 2019 were included in the study, and the prevalence of birth injuries was 37 per 1,000 live births (16).
In the present study, the most prevalent birth injuries were caput succedaneum, cephalohematoma, ecchymosis, subgaleal hemorrhage, hypoxic-ischemic encephalopathy, and Erb’s palsy, and 5 neonates were diagnosed with more than one birth injury. In most studies, the most prevalent birth injury was scalp soft tissue injuries (caput succedaneum and cephalohematoma), which is consistent with the present study (1-6, 17-20). Hypoxic-ischemic encephalopathy was the most prevalent birth injury only in a study conducted at Bijapur Hospital in India (15). It is not consistent with our study.
In the study by Mondal et al., the risk factors associated with birth injuries differed from the present study and included older maternal age, shorter maternal height, higher birth weight, assisted delivery with the non-cephalic presentation, and prolonged delivery (7). In Sauber-Schatz et al.’s study, the relationship between birth injuries and non-cephalic presentation was significant, unlike our study (12). In Shabbir and Zahid’s study, there was a significant relationship between birth injuries, gestational age, and delivery cause, similar to the present study. However, in the mentioned study, other risk factors were premature water breaking, assisted delivery, and birth weight, which is not in line with the present study (13). Among the risk factors revealed in Abedzadeh-Kalahroudi et al.’s study (9), Borna et al.’s study (11), and the present study, there were common factors such as the delivery cause and the type of delivery which is along with this study. In Rezaie et al.’s study, birth injuries had a significant relationship with the Apgar score and delivery age, similar to the present study (10).
5.1. Conclusions
The most prevalent birth injuries are soft tissue injuries. Also, training gynecological assistants and midwifery students is suggested to be a proper solution to reduce the prevalence of birth injuries.