1. Context
The main goal of nursing education is to train an efficient and high-quality workforce to provide healthcare and treatment services. Therefore, nursing education plays a vital role in human health. Accordingly, nursing education should move towards improving and ensuring quality (1). Focusing on quality assessment through guidance and control solutions or promotion measures is an important issue and one of the main challenges of higher education in Iran in recent years. Monitoring and evaluation can be regarded as a way to ensure the quality of curricula in universities and higher education institutions, and it is used in many countries worldwide (2, 3).
Since nursing education is mainly provided in clinical settings and clinical education is known as the heart of the nursing profession (4), more attention should be paid to supervision in clinical education for nursing students (5). Nursing education planners consider clinical education the essential part of nursing education and believe that nursing students can develop their theoretical knowledge by working in an internship setting (6). The clinical setting helps students learn by experimenting and transforming their theoretical knowledge into various mental and psychomotor skills necessary for patient care (7, 8). Clinical education is very complex and involves many aspects that should be considered in improving clinical education (9, 10).
Nursing students must have the minimum necessary competencies to enter the nursing profession, and supervision in clinical education is one of the critical strategies to improve their clinical skills (9, 10). The clinical setting improves students' attitudes, knowledge, and performance in clinics and causes the distance between theory and practice to disappear. However, the basis of a successful clinical education setting is the clinical supervision of nursing students. Numerous nursing sources have highlighted clinical supervision as the only way to demonstrate functional competencies and skills in educational settings. Clinical supervision causes the globalization of the nursing field and contributes to training students with adequate professional skills worldwide (11, 12).
The complexity and unpredictability of the clinical setting have made this setting full of challenges. Thus, clinical supervision can be used to support students in these complex situations. On the other hand, the development of nursing education and academic promotion has led to the complexity of nursing education. Indeed, what the students learn in the classroom has little resemblance to their experience in the clinical setting. However, the supervisor's ability and experience in supporting the students' learning process help them apply their theoretical knowledge in practice. This ultimately reduces the gap between theory and clinical practice. Clinical settings expose students to the real environment and create an opportunity to develop their knowledge, attitudes, and performance. Nevertheless, the most critical point for the success of a clinical setting is the high-quality clinical supervision of nursing students (13, 14).
Although numerous studies have highlighted the benefits of clinical supervision (15) and reported many positive outcomes for supervision in clinical education, before turning such benefits into reality, the educational system needs to acquire the necessary competencies in providing supervision of clinical education. Thus, the effective and safe provision of nursing education requires competence to perform a supervisory role (16, 17).
Although many seminal studies have addressed supervision in clinical education, there are many obstacles to implementing and regulating the education system in clinical supervision. Some of these obstacles include the absence of an effective model, lack of educational resources, managers' and instructors' inadequate knowledge about supervision, managers' insufficient support, instructors' misconceptions of supervision, and the lack of support in the clinical setting for applying educational supervision models. These problems show the need for identifying the exact process and performance of the supervision of clinical education. The benefits of supervision in clinical education imply that such supervision is not part of the nursing profession but the key to solving problems such as the gap between theory and clinical practice, supporting students to become professionals, and generally advancing the nursing profession (18-21).
Supervision plays a crucial role in clinical education. It can also lead to many problems and challenges in nursing education. Furthermore, it contributes to inducing the personal and professional growth of students. Clinical supervision also has positive goals and functions for managers, instructors, students, patients, care organizations, and the nursing profession. Thus, it is essential to provide adequate supervision in clinical education (21-23). Since supervision in clinical education cannot be understood separately from its context, and people in different fields and even in various universities tend to have different perceptions of supervision, there are many differences in factors affecting clinical supervision, the ways to improve supervision in clinical education, and its outcomes in various contexts (24-26).
According to previous studies, there has been significant growth in awareness of the value of clinical supervision. However, there is still not enough knowledge about how clinical supervision contributes to clinical education and practice and what factors are involved (4, 6, 27). In recent years, a growing body of studies has addressed clinical supervision. Nevertheless, these studies have not adequately addressed factors affecting nursing education (21, 22, 28). Qualitative research is a means to accurately understand and deeply discover the complexities of a phenomenon and reveal various aspects and factors affecting that phenomenon (29, 30). Thus, this type of research helps understand the unknown elements of phenomena. Besides, there is no comprehensive study on clinical supervision in Iran, so there is an information gap in this field. To fill this gap, the present study used a qualitative conventional content analysis approach to explain the factors affecting nursing instructors' clinical supervision. The findings of this study can contribute to bridging the knowledge gap in the clinical supervision of nursing instructors in Iran.
2. Procedure
This qualitative study was conducted using a conventional content analysis approach. The participants were 18 persons, including 11 instructors, three students, and four experienced nurses who attended individual interviews. The participants were selected using purposive sampling among applicants who were willing to participate in the study and could express their experiences of supervision in clinical education. Following the qualitative design of this study, the data were collected through in-depth, open, and semi-structured interviews. The approximate duration of the interviews was informed in advance to the participant, and the interviews were recorded with the prior arrangement with the participants upon their permission. The interviews were transcribed verbatim within 24 hours after recording, and the resulting data were used in statistical analysis.
The interviews lasted 20 to 130 minutes. The interviews continued until the data were saturated. Some of the questions that were used only as a guide for the interview were: How do you control the students' performance? What things affect your performance? Could you talk about conditions or experiences that you felt affected your performance and work? Who played a role in this situation, and how? Since qualitative research is conducted in a real setting, i.e., the place where the process and its experiences take place, the participants were selected from the staff in the inpatient departments of teaching hospitals, and the interviews were conducted in the same departments.
The collected data were analyzed using the conventional content analysis approach. To this end, the themes directed from the data were extracted and codified. For qualitative analysis, the content of all the interviews was collected and coded using an inductive coding procedure. The content analysis was performed through four main steps with some adjustments to find the dominant codes (31). After reading the texts several times, the primary codes were extracted, identifying and highlighting significant statements and paragraphs as the units of analysis. It was decided to pay attention to both explicit and implicit content. A core code and sub-codes were extracted from each analysis unit. The core codes with similar meanings were classified in the second coding step. After classification, the codes were put together to form a conceptual model, the relationship between the categories was identified, and the themes were extracted. To validate the extracted themes, we reviewed the data recurrently to provide evidence supporting the extracted themes (30-32). To comply with ethical principles in research, we obtained informed consent from the participants. Besides, the participants' data were kept confidential. The participants were also permitted to leave the study whenever they wished. The interview text was made available to each participant upon their request.
3. Results
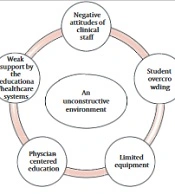
The participants in this study were 18 persons, including 11 instructors, three nursing students, and four nurses that were interviewed individually (Table 1). The instructor's interaction with the clinical setting affects the concept of clinical supervision in nursing education. An exploration of the lived experiences of clinical instructors showed that they face some challenges in clinical settings. A total of 190 codes were extracted from the participants' statements. After reviewing and summarizing the codes several times, they were divided into five main categories: (1) Student overcrowding, (2) clinical education with limited equipment, (3) negative attitudes of clinical staff, (4) physician-oriented education, and (5) the inefficiency of the education-treatment system to support students. In addition, 13 subcategories were identified (Table 2).
| Participant Code | Position | Academic Degree | Age | Gender |
|---|---|---|---|---|
| 1 | Instructor | Ph.D. | 46 | Female |
| 2 | Instructor | Ph.D. | 43 | Male |
| 3 | Instructor | Master's degree | 50 | Female |
| 4 | Instructor | Master's degree | 38 | Female |
| 5 | Instructor | Master's degree | 35 | Male |
| 6 | Instructor | Master's degree | 29 | Male |
| 7 | Instructor | Master's degree | 41 | Female |
| 8 | Instructor | Master's degree | 33 | Female |
| 9 | Instructor | Bachelor's degree | 30 | Male |
| 10 | Instructor | Bachelor's degree | 44 | Female |
| 11 | Instructor | Bachelor's degree | 42 | Female |
| 12 | Nurse | Bachelor's degree | 35 | Female |
| 13 | Nurse | Bachelor's degree | 40 | Female |
| 14 | Nurse | Bachelor's degree | 43 | Male |
| 15 | Nurse | Bachelor's degree | 26 | Female |
| 16 | Student | Bachelor's student | 21 | Female |
| 17 | Student | Bachelor's student | 22 | Female |
| 18 | Student | Bachelor's student | 22 | Male |
| Core Category | Categories | Subcategories |
|---|---|---|
| Non-constructive setting | Student overcrowding and poor control | Student overcrowding in inpatient departments |
| Poor control of students due to overcrowding | ||
| Controlling students is time-consuming | ||
| Physician-oriented education | Official assignment of nursing procedures to medical students | |
| Nurses' emphasis on the performance of nursing procedures by medical students | ||
| Negative attitudes of clinical staff | The negative attitudes of nurses and head nurses toward students' education | |
| Nurses and head nurses as an obstacle to the provision of care by students | ||
| Negative attitudes of clinicians toward education | ||
| Separation of education and the clinical setting | ||
| Clinical education with limited equipment | Limitations in the use of equipment in clinical education | |
| The requirement of the hospital for compensation of damages by the instructor and student and the lack of support from the faculty | ||
| The inefficiency of the education-treatment system | Lack of support facilities for students in the hospital | |
| Disorganization of students caused by weak faculty support |
4. Student Overcrowding and Poor Control
The participants stated that there was a large number of nursing and non-nursing students in the department, and this disrupted adequate supervision and clinical education by the instructor: "There are so many students in the department that our students get lost among them, especially when doctors want to visit patients. There are many students including interns, residents, and even nutrition and laboratory science students. It is practically impossible to do anything with all these people in the department" (Instructor #1).
"Each instructor has to supervise 10 to 12 students who are sometimes working in two different wards. How can you supervise and teach them under these conditions? The only great job we can do is to ensure nothing bad happens" (Instructor #5).
"With this great number of students, I am only an observer, and I can only check if they are present in the ward and control their appearance. Given the students' heavy workload and a great number of students, it is impossible to monitor their performance" (Instructor #7).
Students also reported similar experiences: "There are too many of us. Actually, the instructor can only check if students are present or absent. When we want to do something and need the instructor's guidance, he/she is working with someone else" (Student #1).
Clinical education with limited equipment: The participants pointed out the restrictions in using equipment in clinical education, including the restricted use of expensive drugs due to the risk of their loss and limited insurance coverage for the patient's consumables. These restrictions cause the instructor to face a shortage of equipment and lead to fewer opportunities for supervision and learning.
One of the instructors stated, "Once, the vial of one of the patient's drugs was broken. The drug was very expensive because it was a chemotherapy drug. But the college and the hospital did not provide any support, and the student and I put money together and paid for it. So, we decided to stop using these medicines."
Another instructor said, "I swear to God, many nurses grumble about reporting an extra peripheral venous catheter so that I either have to do venipuncture myself or it should be done under my direct supervision so that the student doesn't waste it and the nurse doesn't have to report an additional catheter. Restrictions make training and supervision difficult."
One of the experienced nurses stated, "Everything was OK in the past. Students were allowed to use any equipment they needed. But now all medicines need to be registered individually, and if something is damaged or non-sterilized by the student, you have to give a logical explanation in the report; otherwise, you will have to pay for it. Insurance companies are getting stricter."
5. Negative Attitudes of Clinical Staff
The instructors reported that they faced some challenges due to the negative attitudes of nurses and supervisors as they entered a new clinical setting. These challenges reduce the efficiency of the learning and teaching process, ultimately leading to the exhaustion of the instructor and ineffective training and supervision: "When you enter a new department, it's as if everyone is your enemy. I often see the nurses and supervisors hide equipment so we would not use them. Now, do you think it's possible to work in this environment, let alone supervise the students" (Instructor #3).
"The clinical staff behaves in a way as if we are disturbing or interfering with their work. They always say that they should do their work themselves rather than get it done by the students" (Instructor #7). "They don't allow students to write reports at all, even though we write reports much better than them. They don't trust our work at all, and the supervisor constantly complains and asks us to leave the station. It is not really possible to work in these conditions. There is a poisonous atmosphere in the station. The internship lasts only four hours on the whole, but we get exhausted and feel disappointed" (Instructor #9).
One of the nurses stated, "Students hinder our work. It is much easier to do the work ourselves than to ask them because we have to check lest they have made a mistake. They sit in the station and make it crowded. The instructors don't do anything useful. They just let the students wander in the department" (Nurse #).
The students also reported the same experience, "The staff doesn't treat us well. They don't teach anything to us, and they are always complaining as if it is not a teaching hospital and we are here to learn something" (Student #2).
Physician-centered clinical education: The participants in this study highlighted the excessive attention of the healthcare system to medical education. Accordingly, with an increase in the number of students admitted to the field of medicine and the changes in the curriculum, most of the nursing procedures have been transferred to the clinical education of medical students, and this is the reason for the limited clinical procedures for nursing. Furthermore, some procedures need to be performed by interns upon physicians' orders. However, these procedures are entrusted by nurses to medical students, making clinical education and supervision more difficult for nursing students.
"They have admitted so many medical students that they don't know what to do with them. They assigned all nursing procedures to medical students, so we don't know what we should teach and supervise" (Instructor #10).
"In all their medical orders, they specify that interns should do some procedures (dressing, NG, Foley catheterization, etc.). So, we have to persuade the supervisor to let us do it, and it is not legal because the law is a doctor's order. Some supervisors and nurses also say interns should do them, and they don't allow us to do them" (Instructor #11).
One of the nurses also stated, "We are obliged to follow the doctor's order. If something wrong happens, no one will support us, and they ask why we let a nursing student do it. Once, the orthopedic surgeon fussed over the infection in a bandaged limb and asked why it had not been done by an intern" (Nurse #1).
A nursing student also stated, "Medical students do all procedures, so we have practically nothing to do, except when the instructor can get a procedure or if medical students are busy, they will allow us to do it" (Student #2).
The lack of support facilities for students and the disruptions caused by the ineffective organization of educational facilities reflect the inefficiency of the educational-healthcare system in providing support to students. This has a significant effect on reducing the instructors' quality of supervision and students' learning.
One of the instructors stated, "If the equipment in the department is damaged while the students are working, no one will support us. The students and instructor have to compensate for the loss of medicines or the damaged equipment, and the university doesn't seem to care as if it has no responsibility" (Instructor #4).
"When the bus brings the students late and leaves before the internship course is ended, how can we control the entry and exit of the students?" (Instructor 8).
A student said, "Our locker room is exactly 10 minutes away from the ward, and it is very far. That's why we are always late. But the instructor does not accept it and asks us to come earlier. The bus arrives late, and the locker room is also far away, how can we get there on time?" (Student #3).
Concerning the lack of educational equipment and the lack of support from the educational system, one of the instructors suggested, "They should provide some additional equipment for students, such as syringes, peripheral venous and Foley catheters, NG, etc. so that nurses don't have to report the breakdown of any equipment or pay for them" (Instructor #1).
Even one of the nurses in the hospital said, "If they don't blame us for consumables and medicines, or if they allocate an additional fund to the education of students, our work will be easier, and we can trust them to do the work better" (Nurse #1).
An exploration of the participants' experiences in this study indicated that the organizational environment affects the performance of clinical supervisors, which essentially facilitates or hinders clinical supervision. Clinical education with limited equipment, negative attitudes of clinical staff, weak support of the educational-healthcare system for students, and physician-centered clinical education were some obstacles to the supervisory and educational functions of nursing instructors. In other words, an instructor can have an adequate supervisory role when there is a proper context. The participants' experiences and statements reflected a "non-constructive clinical setting." As shown in Figure 1, the weak interaction between the two educational and clinical systems responsible for providing clinical education in practice leads to an unconstructive environment. Educational environments should be created for learning; this is not the sole responsibility of clinical instructors. Educational systems should consider clinical settings as educational environments, and to improve them, they should provide a proper context for offering educational services to students by drafting laws and regulations. The findings of this study indicated that drafting regulations for nursing procedures by other students, even regardless of their nature, can actually put nursing students on the sidelines. Thus, educational managers of nursing schools or educational administrators of hospitals are responsible for establishing an effective interaction to optimize and maintain educational justice in these environments.
6. Discussion
An overview of the lived experiences of nursing instructors showed that achieving the goals of nursing education requires qualified instructors who can supervise students in clinical education settings. However, if the instructors are primarily engaged in resolving the restrictions in the clinical setting, they will gain nothing other than marginalizing formal clinical education.
According to the participants, student overcrowding and poor control hinder clinical education and adequate supervision. In fact, the overcrowding of the department makes it difficult to monitor student performance, which managers should consider when planning internship courses. Kermansaravi et al. stated that one of the shortcomings in the educational environment is the failure to perform procedures due to many students. Delaram also considered decreasing the number of students in the clinical setting to improve clinical education. The results of both studies were in line with the present study's findings, confirming the effects of the overcrowding of the department on nursing students' education and supervision (26, 33).
The present study indicated that limited equipment in clinical education leads to a decline in the quality of education and monitoring of learning. Similarly, Aliafsari and Zamanzadeh stated that the lack of equipment and facilities is a factor in students' clinical education. Kermansaravi et al. also emphasized the negative impact of the lack of equipment on the quality of clinical education (33, 34).
The participants in this study pointed to the negative attitudes in the clinical setting, confirming the adverse effect of nurses' non-cooperation and their negative attitudes on clinical education. Shoja et al. found that the nurses' lack of support for students is one of the main challenges of clinical education. Moreover, Mamghani et al. reported the absence of communication between instructors and nurses as an inhibiting factor in clinical education (34-36).
Following the findings of this study, physician-centered clinical education could restrict clinical supervision and decrease the quality of teaching-learning. Paying too much attention to the education of medical students and assigning nursing procedures to them caused limitations in clinical education. On the other hand, the emphasis of nurses and supervisors on the performance of nursing procedures by medical students based on doctors' orders has made the situation more complicated. Rambod et al. considered physician-centered clinical education as an inhibiting factor in clinical education and attributed it to the negative impact of the extra-organization on the decline in the quality of clinical education (37).
The present study highlighted the negative effect of the lack of support from the educational-healthcare system on the quality of clinical education. In fact, the lack of support in equipment and facilities for students can disrupt the education process, and practically, the supervision of the student's performance is also disturbed. Mamghani considered the lack of equipment in the clinical setting and the lack of support from the educational system as the challenges of nursing education. Rassouli et al. also pointed to the weak support in equipment and welfare as inhibiting factors in clinical education (8, 34, 36).
7. Conclusions
The present study indicated that the most critical challenge for nursing instructors and the nursing education system, in general, is non-constructive learning environments. As mentioned, instructors are not the only ones responsible for improving clinical settings. However, to enhance clinical learning and teaching, they should perform the responsibility of clinical supervision effectively and gradually try to minimize the limitations in the educational system with the cooperation of colleges and hospitals. Furthermore, efforts should be made to improve the current situation so that educational supervision is not forgotten because it is the most important function that guarantees the quality of students' education and competencies.