1. Background
With an increase in life expectancy, chronic diseases have become a significant health problem. Chronic, long-term, debilitating diseases with incurable pathology account for 60% of deaths worldwide (1). Chronic kidney failure refers to a process of significant, continuous, and irreversible decline in the number of nephrons, in which the kidney's ability to eliminate metabolic wastes and retain fluids and electrolytes is lost. This failure leads to the syndrome of increased blood urea (2). According to the available data, chronic kidney failure affects more than 10% of the general population worldwide, accounting for more than 800 million people (3). About 320,000 people in Iran are suffering from a severe type of chronic kidney failure. Approximately 49% of these patients have had a kidney transplant, and the rest use hemodialysis (48%) and peritoneal dialysis (3%) (4). Undergoing hemodialysis causes changes in the patient's lifestyle, health status, and roles. Thus, they may face many physical, psychological, and social stressors, and one of the reported problems in dialysis patients is their compliance with treatment (5).
Treatment adherence in hemodialysis patients involves diet adherence, fluid intake restriction, and compliance with drug regimens used to improve kidney failure symptoms (6). However, the lack of treatment adherence is common in hemodialysis patients, and about 25% to 86% of these patients do not follow their treatment regimens. Noncompliance with treatment regimens leads to numerous complications, including shortening the duration of dialysis, not taking drugs correctly, and not observing the diet and fluid restrictions (7, 8). About 50% of patients have fluid restriction, and 44% do not observe some aspects of diet (9). There is evidence of the relationship between treatment adherence in dialysis patients and reduced hospitalization of these patients (7). Non-adherence to treatment in these patients often leads to additional tests, changes in the treatment plan, changes or adjustments in the doses of prescribed drugs, hospitalization, and increased costs of medical care. It also aggravates weight gain between two dialysis sessions and causes complications such as muscle cramps, shortness of breath, dizziness, anxiety, worry, lung edema, heart failure, and high blood pressure (10-12).
Hemodialysis patients need effective training to follow complex treatment regimens, care for themselves, and improve their quality of life. Several studies have confirmed the positive effects of education on these outcomes, including the quality of life (13-15). Accordingly, nurses can play a key and effective role in educating these patients. In other words, patient education is one of the important aspects of nursing care and one of the critical roles of nurses in providing healthcare services. Furthermore, the Charter of the Patient's Rights also declares that it is the patient's right to receive accurate information from the caregivers about the diagnosis, type of treatment, and prognosis of the disease (16). Several factors highlight the necessity of educating the patient, including prevention of diseases, recovery, and reduction of the patient's pain, adaptation to chronic diseases and disabilities, shortening of hospitalization, reduction of disease recurrence, improvement of quality of life, assurance of continuity of care, reduction of patient's anxiety, reduction of disease complications, increased engagement in care programs, and enhancing the patient's independence in performing daily activities (17). Despite the importance of patient education, there are many obstacles to patient education, such as anxiety, poor physical condition, lack of knowledge about the benefits of patient education, lack of time for healthcare workers, role conflict between specialists in different fields of medical sciences, poor management support, lack of material resources (financial, equipment, and facilities), and lack of educational skills of healthcare staff (18). A study in Iran showed that the nurses do not sufficiently provide the training needed by the patient because of the lack of time of the nursing staff, insufficient resources, unsuitable environment, nurses' unawareness, and their disregard for this issue (19); thus, patient education should be considered a continuous process. It is also possible to follow up on the treatment through the patient's regular visits to the treatment center. However, given the significance of long-term follow-up, there should be an easy and applicable follow-up method for many patients (20). Although mHealth technologies cannot physically transport drugs, doctors, and equipment between different locations, they have the potential for fundamental changes and improving the healthcare experience and outcomes. They can transport and process data in various forms, such as encrypted data, texts, audio files, and videos (21).
Mobile phone applications enable nurses to perform various actions such as monitoring the patient, providing training, collecting information, performing nursing interventions, controlling pain, and supporting the patient's family (20). With the help of mobile technology, nurses can enhance the quality of life, reduce medical costs and length of study, and empower patients. Mobile technology can be used to plan activities, make clinical decisions, and manage signs and symptoms (22). Research has shown that using mobile phones can help educate patients in managing chronic diseases such as migraine and provide early diagnosis and self-care for breast cancer (23-26).
Many mHealth applications and optimization programs focus on self-monitoring and self-care. These applications provide a tool to help measure health parameters that will contribute to determining and achieving the treatment goals of patients (21). In clinical settings, this technology is essential for providing access to documented information in the healthcare field (27). Hence, considering the importance of patient education, the chronic and debilitating nature of the final stage of kidney diseases, the need of patients for long-term use of hemodialysis, and the impact of the disease and treatment methods on patients' treatment adherence, there is a need for enhancing the effectiveness of patient education to improve the compliance of these patients to the treatment regimen (16, 19). Moreover, mobile phone applications are relatively new patient education techniques. Such applications have many advantages, such as saving time, remote training and follow-up, and no need for the physical presence of the patient and healthcare staff for training, among others. Thus, it is essential to measure the effectiveness of this method compared to routine training, which is an available method.
2. Objectives
The present study aimed to examine the effect of mHealth training on treatment adherence of hemodialysis patients in Zahedan in 2022.
3. Methods
This quasi-experimental study was conducted on two groups (with a pretest-posttest design). The research population consisted of all hemodialysis patients who visited two hemodialysis centers affiliated with Zahedan University of Medical Sciences in 2022. The inclusion criteria were age over 18 years, undergoing dialysis for at least three months, verbal communication, having no known cognitive and psychological disorders, having a mobile phone with an Android operating system, not using psychoactive drugs, literacy in the use of mobile smartphones (attaining a minimum score of 33 in the standard media literacy questionnaire representing the average level of media literacy), the ability to read and write, and not suffering from acute physical or mental illnesses (according to the patient's medical records). The exclusion criteria were the transfer of the patient to a hemodialysis center outside of Zahedan for any reason and the unwillingness to continue participating in the study.
The sample size was estimated as 13 persons in each group based on the mean treatment adherence score for hemodialysis patients reported in a similar study, with a 95% confidence interval and 95% test power based on the following formula (28):
To ensure sample adequacy, taking into account possible dropout and the possibility of performing statistical tests, the sample size was 40 persons in each group (80 persons in total). The selected patients were divided into two intervention and control groups using random permutation blocks. To this end, the blocks with even sizes (4 blocks) were written in eight modes such as (A, A, B, B) (A, B, A, B). Then, with the enrollment of the first patient, one mode was selected from among the eight modes. Thus, half of the persons in each block were placed in the intervention group and the other half in the control group. Afterward, the researcher collected data related to the patient's characteristics and treatment adherence through interviews with the patients.
The data were collected using two instruments completed through face-to-face interviews with the patients. A demographic information form was used to record the patients' demographic characteristics, including age, sex, education, marital status, occupation, ethnicity, and duration of end-stage kidney disease. Moreover, the Media Literacy Questionnaire was used to measure the participants' media literacy using 20 items scored on a five-point Likert scale (1 = strongly disagree to 5 = strongly agree). A respondent's score in this questionnaire ranges from 20 to 100. A score of 20 to 33 shows a low level of media literacy, a score of 33 to 66 indicates an average level of media literacy, and a score of higher than 66 shows a high level of media literacy. The validity of the questionnaire was confirmed, and its reliability was established with a Cronbach's alpha coefficient of about 79% (29). The End-Stage Renal Disease Adherence Questionnaire (ESRD-AQ) measured the patients' treatment adherence. The instrument was developed by Kim et al. (30). It contains 46 items and five primary subscales: General information (5 items), adherence to hemodialysis treatment (14 items), medications (9 items), fluid restrictions (10 items), and dietary restrictions recommendations (8 items). The overall treatment adherence score ranging from 0 to 1200 is obtained as the sum of the scores on the five subscales, with higher scores indicating better adherence to the treatment. The items are scored on a 5-point Likert scale (1 = non-adherence to treatment to 5 = total adherence to treatment). To assess treatment adherence, one standard deviation above and below the total score is considered the average treatment adherence, with scores higher than the average level indicating good treatment adherence and scores below the average level indicating poor treatment adherence. Rafiee Vardanjani et al. translated and validated this questionnaire in Iran. Its reliability was confirmed with Cronbach's alpha of 0.98 and the test-retest score of 0.85 (31). The Cronbach's alpha value for the questionnaire was estimated at 0.85 in the present study.
First, the researcher completed the Media Literacy Questionnaire through face-to-face interviews at the patient's bedside. The patients who scored less than 33 (the average media literacy level) were excluded from the study. Afterward, the demographic information form and the ESRD-AQ were completed for the participants in the two intervention and control groups through face-to-face interviews with them. In the next step, the participants in the intervention group attended the mHealth training program using a mobile app developed by the researcher. The app was given to the patients and their main caregivers. Three months after the first measurement occasion, the ESRD-AQ was again completed by the researcher through face-to-face interviews with the patients at the hemodialysis department. The patients in the control group received routine training provided by the nursing staff in the hemodialysis department. The ESRD-AQ was completed three months after its first administration through face-to-face interviews with the patients in the control group. The researcher was in contact with the patients and the caregivers during the intervention period through Goftino, an online communication platform, to answer any possible questions from the patients and caregivers. Goftino has some features such as a profile for each user, the ability to leave messages for and receive messages from the admin, the possibility of regular recording of health reports and data (dry weight, weight before the dialysis session, fluid intake, etc.) by the patients themselves, the curve showing the changes in the patient's health data, recording laboratory indicators, and containing educational clips.
As shown in Table 1, the content of the mHealth training program focused on the kidney and its chronic failure, fluid intake restrictions, compliance with medication regimen, exercise, and physical activity (32-36). All these sessions were held using video clips prepared by the researcher. The clips used simple and understandable language without any specific medical terms and highlighted the importance of treatment adherence for hemodialysis patients.
| Sessions | Content | Duration (min) |
|---|---|---|
| 1 | Introducing the functions of the kidney, chronic kidney failure, its symptoms and complications, dialysis and its complications and side effects | 4:31 |
| 2 & 3 | Dietary recommendations (restrictions in salt intake, foods that have hidden salt, more use of fresh fruits and vegetables, reading food labels, effects of sodium on blood pressure), fluid intake and balance, consuming coffee and tea per day and quitting smoking and alcohol | 3:13 & 8:18 |
| 4 | Compliance with medication regimen (instructions on use and side effects of medications, drug interactions, etc.) | 3:39 |
| 5 | The role of exercise in disease prevention and exercise strategies for dialysis patients | 4:32 |
The Content of the mHealth Training Program
The collected data were analyzed using SPSS-26 software. First, the normality of the data was checked using the Shapiro-Wilk test. Then, the frequency, percentage, average, standard deviation, minimum, and maximum were calculated through descriptive statistics. The paired samples t-test was used to compare the mean scores for each group before and after the intervention. In addition, the independent samples t-test was used to compare the mean scores between the two groups before and after the intervention. The frequency of the qualitative variables for the two groups was checked using the chi-square test. Analysis of covariance (ANCOVA) was also run to assess the effectiveness of the intervention by controlling the effect of the pretest and some possible confounding variables. The significance level in this study was considered less than 0.05 (P < 0.05).
4. Results
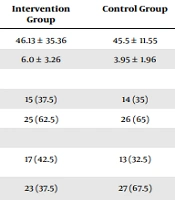
An analysis of the participants' demographic data showed that the patients in the two control and intervention groups were homogenous in terms of demographic and clinical characteristics. Thus, the patients of both groups had no significant differences in age, gender, marital status, occupation, and ethnicity (P > 0.05). However, there was a significant difference between the two groups regarding the average disease duration (P = 0.001). Other demographic findings are shown in Table 2.
| Variables and Categories | Intervention Group | Control Group | P-Value |
|---|---|---|---|
| Age | 46.13 ± 35.36 | 45.5 ± 11.55 | 0.76 b |
| Disease duration | 6.0 ± 3.26 | 3.95 ± 1.96 | 0.001 b |
| Gender | 0.82 c | ||
| Male | 15 (37.5) | 14 (35) | |
| Female | 25 (62.5) | 26 (65) | |
| Education | 0.36 c | ||
| Primary school | 17 (42.5) | 13 (32.5) | |
| Diploma or higher education | 23 (37.5) | 27 (67.5) | |
| Marital status | 0.74 c | ||
| Single | 6 (15) | 5 (12.5) | |
| Married | 34 (85) | 35 (87.5) | |
| Occupation | 0.22 c | ||
| Unemployed | 13 (32.5) | 7 (17.5) | |
| Housewife | 20 (50) | 19 (47.5) | |
| Employee | 8 (20) | 13 (32.5) | |
| Ethnicity | 0.40 c | ||
| Baluch | 26 (65) | 23 (57.5) | |
| Fars | 14 (35) | 17 (42.5) |
Comparing the Demographic Indicators in the Two Groups a
As shown in Table 3, the mean treatment adherence score of the patients in the control group increased significantly from 1011.87 ± 150.96 before the intervention to 1110.62 ± 86.95 after the intervention (P < 0.001). The corresponding value for the patients in the intervention group increased from 1067.50 ± 122.24 before the intervention to 1161.25 ± 49.98 after the intervention, showing a significant increase (P < 0.001). The independent samples t-test showed that the mean treatment adherence scores of the patients in the two study groups did not differ significantly before the intervention (P = 0.07), but it showed a significant difference after the intervention (P = 0.002). Moreover, the results of ANCOVA to control for the significant effect of the pretest scores and the duration of the disease indicated that the mean treatment adherence scores for the patients in the two groups showed a significant difference after the intervention (P < 0.05) (Table 4).
| Time Group | Pre-intervention | Post-intervention | P-Value |
|---|---|---|---|
| Control | 1011.87 ± 150.96 | 110.62 ± 86.95 | < 0.001 |
| Intervention | 1067.50 ± 122.24 | 1161.25 ± 49.98 | < 0.001 |
| P-value | 0.07 | 0.002 |
Comparing the Mean Treatment Adherence Scores in the Two Groups Before and After the Intervention a
| Source of Changes | Sum of Squares | df | Mean Squares | F | Sig. | Effect Size | Test Power |
|---|---|---|---|---|---|---|---|
| Pretest | 238220.4 | 1 | 238220.4 | 117.60 | 0.001 | 0.61 | 1.0 |
| Disease duration | 3121.22 | 1 | 3121.22 | 1.54 | 1.54 | 0.02 | 0.23 |
| Group | 8813.59 | 1 | 8813.59 | 4.35 | 4.35 | 0.05 | 0.45 |
| Error level | 153950.6 | 76 | 2025.67 | ||||
| Total | 1.04 E+8 |
ANCOVA Results for the Mean Treatment Adherence Scores of the Patients in the Two Groups After the Intervention
5. Discussion
The data in the present study indicated that the mean treatment adherence scores for the hemodialysis patients after the intervention significantly differed between the mHealth training group and the control group. However, the treatment adherence scores for the patients in the control group who received routine training by healthcare staff were higher than those in the mHealth training group, which was contrary to expectations.
The study results showed that the overall treatment adherence scores of the hemodialysis patients in the intervention and control groups were not significantly different before the intervention. This finding was consistent with the data reported by Davoudi et al. (37). However, the mean treatment adherence scores reported in other studies were lower than the mean score reported in the above study (38-40). The present study findings implied that a higher level of media literacy could increase treatment adherence (41). Following the requirements for enrollment in this study, such as using mobile phones, having moderate media literacy, and the ability to read and write, the patients in this study had a higher level of media literacy. Thus they obtained higher treatment adherence scores compared to other similar studies.
Moreover, since the patients in the present study were literate and had average media literacy, this intervention did not significantly affect their average treatment adherence score compared to the control group. Besides, the disease duration was longer in the patients in the intervention (mHealth) group than in the control group, which could slightly affect the training with the mHealth application. Hadian et al. showed that the effectiveness of two face-to-face and video self-care training programs on various aspects of treatment adherence of patients undergoing hemodialysis did not differ significantly (5). Therefore, despite the belief that mHealth training is more effective and has advantages such as saving time and not needing the instructor's presence, the findings of this study showed that routine training without a live and active instructor was almost as effective as mHealth training. This means that if a training program is executed based on scientific principles and models and a sound understanding of patients' needs and problems, it can be effective with different instruction methods.
Jayanti et al. reported that education increased the understanding of patients, ultimately enabling them to have more control over diet and fluids and thus reduce the frequency of hemodialysis (42), as confirmed in the present study. Contrary to the present study, another study by Wells in the United States showed that the educational intervention for chronic patients improved their knowledge, but these researchers pointed out that an increase in the patient's knowledge did not affect their treatment compliance (43).
Moreover, in line with the findings of the present study, Li et al. showed that the use of mHealth apps and social media not only improves self-efficacy and self-management in patients with chronic kidney failure but also facilitates increasing glomerular filtration rate (GFR) and drawing a healthy lifestyle for patients (44). Moreover, Connelly et al. showed that mobile phone applications not only improve the treatment process and effective dietary adherence in patients but also induce innovation and create insight into providing better healthcare services to patients suffering from chronic disorders (45). Feizalahzadeh et al. showed that multimedia-based education on "hemodialysis and necessary care" and the traditional methods (face-to-face education and pamphlets) improve the patient's knowledge and have positive effects on various aspects of treatment adherence in hemodialysis patients (33), as was confirmed in the present study.
Ong et al. showed that using mobile phone applications prevents the progression of symptoms of a person's disease and improves their awareness of taking medicines, precautions, and possible side effects. On the other hand, these applications significantly reduce medication errors and help patients to comply more effectively with the treatment (46). Following the findings of these studies, training interventions can improve patients' awareness of the disease, symptoms, and treatment adherence. Moreover, developing some applications for patients can reduce the time of instructions provided by nurses and provide information resources to patients so that they can get aware of their disease at any time and place and manage it well. One of the limitations of the present study was the short follow-up period of the patients. Thus, similar studies can examine patients over a longer period. Furthermore, one of the requirements for patients to enter this study was an average level of media literacy. Hence, the patients could search for their problems from different sources, such as the Internet, and find their solutions.
5.1. Conclusions
The present study showed that mHealth training and routine methods could help hemodialysis patients learn effective ways to adhere to the treatment. In other words, both mHealth training and routine training positively affected patients' treatment adherence. Thus, considering the effectiveness of routine training, mHealth training can be used with routine training in treatment programs for hemodialysis patients to improve treatment adherence in these patients.