1. Background
Psoriasis, as one of the most common inflammatory skin diseases, is affected by various predisposing factors, such as race, geographical location, genetic factors, and environmental conditions (1, 2). Previous studies have reported the prevalence of psoriasis to vary from 0.6% to 4.85% in different communities (2). In addition, 2 - 2.6% of individuals in the United States are affected by this disease, and 150,000 to 260,000 new cases are annually reported (3). The prevalence of psoriasis has been reported to be less than 1% in Iran (4).
Psoriasis is characterized by skin inflammation with symptoms in the form of scaly red plaques noticed in different parts of the body (5, 6). Therefore, living for a long time with skin and appearance symptoms can threaten the identity and lead to changes in the patient’s roles, mental image, or lifestyle (7).
Psoriasis patients often suffer from complications, such as adjustment disorders, low self-confidence, body dysmorphic disorder, and feelings of embarrassment and shame (6), because the individuals around them and others avoid having contact with the patients, and this behavior leads to fear and lower self-image in the patients. If such behaviors are repeated, they might cause anger, shame, and despair in the patients. Finally, this makes patients worry about dealing with others and avoid social activities (2, 8). Consequently, patients experience the feeling of being defamed, ashamed, and embarrassed due to their appearance (9). Therefore, such feelings in patients with psoriasis force them to hide their disease from others (10).
Another factor that affects the lives of psoriasis patients is multiple visits to skin clinics to receive different and long-term treatments, which leads to a waste of time and high costs (11). These patients, similar to other patients suffering from chronic and debilitating diseases, need permanent and lifelong treatment and care and are struggling with many psychological, economic, and social problems, each somehow disturbing treatment adherence and follow-up. Given the small number of studies in this field, the nature of psoriasis, and the unique experiences of each patient, the patient’s lived experiences gained through their social interactions cannot be adequately explored using a few questionnaires or a set of closed questions (12).
If the available information in a specific field is limited, it will be difficult to determine what the unknowns are. Therefore, a naturalistic approach and qualitative methods should be used to detect unknown factors (13). This approach advocates qualitative methods in research. Qualitative research is a systematic and subjective method that provides significant and rich information about events, human behaviors, and activities and allows us to define, interpret, and better understand the meaning of activities, problems, and processes in the social context. Qualitative research is based on the assumption that individuals themselves in certain situations have the best position to analyze and describe their experiences and feelings in their language (14). The epistemology of the qualitative perspective relies on understanding, and understanding is the outcome of interpreting human social situations (13). Qualitative research is defined as a systematic method of investigation to understand human beings and their interactions with themselves and their surroundings. Qualitative research is a holistic method that considers humans in the environment with all their complexities (15).
Qualitative research is conducted to provide a deep and comprehensive understanding of the whyness and howness of existing phenomena and processes, and choosing a suitable research method depends on the explored phenomenon and the research questions (16). Qualitative research is conducted using different approaches, and the main goal of all approaches is to investigate meanings (17).
All qualitative studies, regardless of their type, have many common features, including attaching weight to participants’ views, belief in multiple facts, exploring the research problem in a natural setting, commitment to follow methods that lead to a deeper understanding of the phenomenon in question, giving importance to the engagement of the researcher in the research process, and conveying what the researcher has understood in the form of a literary report rich in the participants’ statements (18).
Since the nursing profession pursues a very strong humanistic approach to its daily functions, a positivist method cannot effectively respond to its problems and questions. Holistic paradigms and quantitative approaches have been expanded and endorsed by nursing experts. Additionally, naturalistic research has received much attention from academia and researchers. Accordingly, qualitative research methods can answer many deep and complex questions about humans and their behaviors, such as the patients’ experiences of psoriasis.
2. Objectives
This qualitative study aimed to provide a deep understanding of the experiences of patients with psoriasis.
3. Methods
This study was conducted using a phenomenological approach. Phenomenology is one of the best research methods to deeply understand experiences and conceptualize a key meaning. Interpretive phenomenology is used for exploring relationships and meanings. This approach is a special type of phenomenology whose purpose is to reveal the hidden meanings of phenomena (19).
3.1. Participants and Sampling
The participants in this study were patients diagnosed with psoriasis who were admitted to the skin clinics of hospitals affiliated with Zahedan University of Medical Sciences, Zahedan, Iran. The participants were selected via purposive sampling. The researcher tried to select the participants purposefully to collect the specific information needed. During the sampling process, the participants were selected with maximum variations in terms of characteristics, such as age, gender, education, and duration of disease diagnosis, to obtain different views and collect rich data. The data collection process continued until data saturation. The participants in this study were 10 patients with psoriasis.
Before starting the study, each participant was informed about the objectives of the study, the research procedure, and how the interview would be conducted. The data were saturated with 10 interviews conducted with the participants. From the eighth interview onward, no new information or theme was obtained, and the collected data were saturated.
3.2. Data Collection
Interviewing is the main data collection method in phenomenological studies. An interview provides an opportunity for participants to describe their view of the world as they experienced it using their own language and words. The purpose of the interview in phenomenological studies is to extract the participants’ responses from the depth of the subject, and participants discuss their experiences about the subject in question (13). The data in phenomenological studies are collected through semi-structured, in-depth, and multiple interviews with participants. The data in this study were collected through semi-structured interviews with the patients using an interview guide.
This research project started on September 30, 2018, and finished on July 17, 2019. The interviews with the patients were conducted by the researcher using open-ended questions in one of the hospitals in Zahedan. Additionally, the interviews with three participants were conducted at their homes. The time of each interview varied from 60 to 90 minutes based on the participants’ agreement. Moreover, the interviews with two participants were conducted on two occasions. The participants’ statements during the interviews were recorded upon their permission and were then transcribed word by word. The questions focused on the patients’ life experiences from the time of developing the disease until the time of the interview (e.g., how did you find out about your disease? Could you please describe it? What things have happened to you since you got psoriasis?). All the interviews were conducted by the researcher.
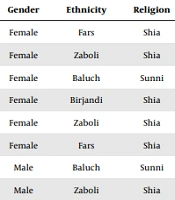
The participants were selected using purposive sampling based on the inclusion criteria. The researcher provided some instructions for the participants about the objectives of the study and the research procedure and clarified his/her position in this research project. Each interview lasted 60 - 90 minutes, depending on the participant’s willingness. The place and time of the interviews were determined with the participants’ agreement. Therefore, seven participants were interviewed at the hospital, and three participants were interviewed at their homes (Table 1). The interviews were recorded with the permission of the participants while maintaining the confidentiality of their identities.
| Code | Age (y) | Disease Duration (y) | Education | Place of Residence | Gender | Ethnicity | Religion | Income Level | Medication |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 29 | 10 | Master’s student | Zahedan | Female | Fars | Shia | Average | Corticosteroid, light therapy, homemade ointments |
| 2 | 21 | 2 | High school diploma | Zabol | Female | Zaboli | Shia | Low | Corticosteroid, homemade ointments |
| 3 | 18 | 5 | High school diploma | Khash | Female | Baluch | Sunni | High | Corticosteroid, homemade ointments |
| 4 | 15 | 1 | High school student | Zahedan | Female | Birjandi | Shia | High | Corticosteroid, homemade ointments |
| 5 | 20 | 4 | Bachelor’s student | Zahedan | Female | Zaboli | Shia | Average | Corticosteroid, homemade ointments |
| 6 | 34 | 10 | Bachelor’s degree | Zahedan | Female | Fars | Shia | High | Corticosteroid, light therapy, homemade ointments |
| 7 | 31 | 2 | High school diploma | Zahedan | Male | Baluch | Sunni | Average | Corticosteroid |
| 8 | 39 | 1 | Bachelor’s degree | Zabol | Male | Zaboli | Shia | Average | Corticosteroid |
| 9 | 44 | 3 | High school diploma | Iranshahr | Male | Baluch | Sunni | Low | Corticosteroid |
| 10 | 46 | 1 | Associate degree | Zahedan | Male | Fars | Shia | Average | Corticosteroid |
3.3. Data Analysis
Data analysis was performed using Colaizzi’s seven-step method with MAXQDA software (version 10) by the members of the research team. In the first step, the interviews were recorded and listened to. Then, the content of the interviews was transcribed word by word on paper, and the transcripts were read several times to gain a deep understanding of their meanings. In the second step, the sentences or statements related to the phenomenon in question were underlined. In the third step, primary codes were extracted. In the fourth step, the collected codes were converted into subthemes. In the fifth step, the extracted subthemes were merged into a set of themes based on their similarities and differences. In the sixth step, a thorough description of the phenomenon was presented. In the last step, the findings were validated by referring to the participants and discussing the findings. In qualitative studies, the data can be validated by referring to each participant to follow up on their opinions about the validity of the data.
3.4. Study Rigor
The criteria proposed by Lincoln and Guba (as cited by Anney), including credibility, dependability, confirmability, and transferability, were used to establish the rigor of the study (20). The credibility of the findings was enhanced using member checking. To this end, the text of the interviews was returned to the participants after coding to ensure a consistent understanding of the content by the researcher and the participants. The researcher’s prolonged engagement in data collection, codification, and analysis led to the researcher’s immersion in the data. In addition, the data codification and analysis procedure were reviewed and approved by subject-matter experts in the research team who had adequate experience in qualitative research and were familiar with psoriasis. The participants were selected from psoriasis patients with maximum variations in terms of demographic characteristics to ensure the transferability of the findings. To increase the confirmability of the data, the researcher tried to record and describe all procedures adopted in data collection, codification, and analysis so that they could be further examined by readers and other researchers.
3.5. Ethical Considerations
The permission to conduct this study was obtained from the Ethics Committee of Zahedan University of Medical Sciences, Zahedan, Iran (ethics code: IR.ZAUMS.REC.1401.262). This study was conducted in compliance with the ethical principles of the participants’ freedom, autonomy, and confidentiality. Written and oral informed consent was obtained from all the participants, and their participation in the study was voluntary. They were also assured of the confidentiality of their information. Before conducting the interviews, the necessary information was given to the participants regarding the objectives of the study and the research procedure. Written consent was obtained from the participants for audio and video recording of the interviews, and they were allowed to leave the study at any stage if they wished.
The participants’ age ranged from 15 to 46 years. Table 1 shows the participants’ demographic characteristics.
4. Results
Data analysis revealed 180 primary codes divided into three main themes, namely the progression of the disease in the shadow of the ignorance of the medical staff, physical and mental suffering, and the ominous shadow of fear of the disease recurrence. Table 2 shows the themes and subthemes extracted in this study.
| Subthemes | Themes |
|---|---|
| Doctors’ initial unawareness of the early symptoms of psoriasis; difficulties faced by the patient due to the distance to specialized medical centers in Tehran; wrong diagnoses and deterioration of the disease; disappointment with modern medical treatments and turning to traditional medicine | The progression of the disease in the shadow of the ignorance of the medical staff |
| The limitations and side effects of drug therapy; patient isolation; psychological complications | Physical and mental suffering |
| The patient’s constant worry and fear of disease recurrence; discontinuation of treatment causing the return of psoriasis symptoms | The ominous shadow of fear of the disease recurrence |
4.1. Progression of the Disease in the Shadow of the Ignorance of the Medical Staff
This theme was divided into four subthemes detailed as (1) doctors’ initial unawareness of the early symptoms of psoriasis; (2) difficulties faced by the patient due to the distance to specialized medical centers in Tehran; (3) wrong diagnoses and deterioration of the disease; and (4) disappointment with the modern medical treatment and turning to traditional medicine.
The participants’ statements indicated that they suddenly discovered a series of initial symptoms and did not know anything about these skin lesions. Due to extreme fear and concern, they went to general practitioners; however, they failed to diagnose the disease. Therefore, the patients suffered from high stress. Furthermore, the distance from medical centers in Tehran and the lack of facilities to help diagnose the disease increased the financial burden on the patients’ families. Even this rare disease was not correctly diagnosed in the patients who had access to facilities and reputable doctors. Moreover, the use of ineffective medications and the accumulation of chemicals resulted in more damage to other vital organs of the body. On the other hand, given the cultural norms prevalent in the province, individuals generally advised the patients to seek traditional medicine, and since the patients were disappointed with modern medical treatments, they often turned to traditional medicine.
The patients in this study also complained about doctors’ initial unawareness of the early symptoms of psoriasis. One of the patients stated: “My body was filled with flaky patches, and they took samples several times; however, they did not diagnose the disease or diagnosed it wrongly. I referred to many other doctors and, finally, a doctor took a skin sample and stated that I was suffering from a skin disease but could not specify the type of the disease” (participant #1).
The patients also pointed to the wrong diagnoses by doctors and the deterioration of the disease. One of the patients stated: “The doctor said I should take a blood test or go to a hematologist; maybe these symptoms are caused by an infectious disease. He gave me a handful of antibiotics and told me to take them for 2 weeks to see what happens to my symptoms” (participant #9). The same participant added: “Once, even one of the doctors prescribed an ointment for me. These ointments were handmade and very expensive. I applied that ointment, and I did not get better at all. Three days later, when I returned from Tehran, I went to my doctor, who was doing phototherapy. I showed him the ointment, and he said that this ointment is for vitiligo patients, and I stopped using the ointment”.
The patients in this study also stated that they got disappointed with modern medical treatments and resorted to traditional medicine. One of the patients stated: “The doctors did not tell me that if I did not treat it, this disease would progress and the symptoms get worse. So, I did not complete my treatment and did not pay much attention until my disease progressed a lot, and no doctor could do anything for me; I am angry with the doctors who did not tell me to do so. Later on, I made inquiries and found out that the side effects of phototherapy with old devices are black spots on the skin with severe skin wrinkles, cataracts, and glaucoma. Well, when you are told that treatment is useless, you suddenly turn to traditional treatments because my grandfather had an herbal shop. Traditional treatments were always used for any diseases, and interestingly, they were also good, for example, for colds. I convinced myself that this treatment is of no use to me” (participant #5).
4.2. Physical and Mental Suffering
This theme was further divided into three subthemes, namely (1) the limitations and side effects of drug therapy; (2) patient isolation; and (3) psychological complications.
The psoriasis patients in this study reported that when the disease was diagnosed, a secondary fear developed in them, making them refer to different doctors and follow different treatments with many complications. Moreover, when the symptoms did not disappear with treatment, they slowly began to change their behavior and retreat to isolation, and this was the beginning of psychological complications for the patient. These complications were sometimes mild and sometimes very severe, as reported by the participants.
The limitations and side effects of drug therapy were among the common problems faced by the patients in this study. One of the patients reported: “First, a small spot appeared on my head. I went to the doctor in Khash , and then they told me that it was a fungus grown on my head. The doctor prescribed shampoo, pills, and a solution. However, when I used these medicines, the symptoms got worse, and after a few months, I went to a dermatologist in Zahedan. He said I got psoriasis and was prescribed homemade soluble drugs. When I started taking these medicines, I had severe nausea, and I was lethargic; then, I went to another doctor, and he said that I should not have taken the medicines prescribed by the previous doctor because these medicines were not suitable for young people and would ruin the liver” (participant #3).
The isolation of patients was another problem reported by the participants in this study. One of the patients stated: “I did not feel comfortable. Even though I spent time with my friends on different occasions, I tried to avoid them as much as possible due to my symptoms; if they saw them, it would be very bad for my family members and me. Baluch people usually have their daughters get married at a young age, and this is a concern for families. When I realized that I could not treat these spots better with therapies, medicines, and ointments, I tried to avoid people lest they notice these spots. Since then, I have not attended any party or ceremony for many years, and every time anyone wants to see me, I make an excuse” (participant #8).
The same participant added: “I was diagnosed with a disease about a year ago. The doctor said that it was psoriasis and there was no cure, and we should just stop the progress of this disease. I cried a lot. There was no cure. It was like the world collapsed on my head. Mentally, the disease had negative effects on me. I was the only girl in the family, and at school, they asked me what these things were. They came close and looked at me. I had no way to do anything. Even one day, my health teacher asked me a lot of questions, and she did not accept any of my responses. She asked me to come with my mother the other day. When we went to school the next day, she asked my mother what the name of my illness was. She wanted to make sure that the disease was not contagious and that other students would not get it. I did not like going to school at all. I had just a friend, but I did not have a relationship with her anymore. I cannot control my behavior. It is like I have become psychotic. I feel anxious and depressed. I am exhausted due to this disease”.
4.3. Ominous Shadow of Fear of the Disease Recurrence
This theme was divided into two subthemes, namely (1) the patient’s constant worry and fear of the disease recurrence; and (2) discontinuation of treatment causing the return of psoriasis symptoms.
The patients in this study stated that doctors and researchers have pointed out that after the partial treatment of the disease and the improvement of the symptoms, one-third of the patients will have a recurrence of the skin lesions, and in case of insufficient treatment, the symptoms will develop progressively. Therefore, patients who have been treated or are being treated pointed out that this disease might be with them for the rest of their lives.
The patients in this study had constant worry and fear of the disease recurrence. One of the patients stated: “Corticosteroid drugs that we used in Yazd were very good. They stopped the disease. I felt uncomfortable because the dandruff that was on my head due to psoriasis plaques could be seen through my hair, and it was very annoying cosmetically. It would have spilled over my clothes, especially when I was wearing dark clothes. I got a lot better with medication, and this helped me to get along with this disease. The disease got much better. It seemed to be silent for several years. Last year when I had the university entrance exam, the disease started getting worse suddenly. I did not know what to do anymore” (participant #7).
The participants also stated that stopping the treatment would contribute to the return of the psoriasis symptoms. One of the patients stated: “I was taking the drugs for 3 years, and then I stopped using them for a year. Afterward, the disease started getting worse, and my whole body started to have awful muscle pains. Then, the symptoms spread all over my body, covering my chest. Only below my neck to my chest remained unaffected. Even my legs, knees, and hands were also affected. At first, there were small round spots. Then, they grew in circles, dried up, and began to scab and itch” (participant #1)
5. Discussion
This study explored the experiences of patients with psoriasis. The results revealed three main themes, including the progression of the disease due to the inadequate knowledge of the medical staff, physical and mental suffering, and the ominous shadow of fear of the disease recurrence.
The second theme, physical and mental suffering, was further divided into three subthemes, namely (1) the limitations and side effects of drug therapy; (2) patient isolation; and (3) psychological complications. When a person is diagnosed with psoriasis, they experience fear and anxiety and try to reduce the symptoms and psychological complications by visiting different doctors and receiving multiple treatments that are associated with more complications. Psoriasis patients are afraid of being labeled and rejected by others (21). Psoriasis forces patients to live a life of secrecy. Patients might avoid activities, such as sunbathing, for fear that others will find out about their illness (22); as a result, the patients gradually begin to change their behavior and retreat to isolation due to the feeling of stigma, and this is the beginning of mental complications for patients.
Takata et al. showed that depression, anxiety, and social stigma are common among patients with psoriasis (23). Joachim and Acorn also showed that patients with chronic diseases with visible or invisible symptoms hide their disease from others for various reasons, such as increasing the support of sympathetic individuals or stigma and isolation (24). This is also the case with patients with psoriasis, and they try to hide their disease. Furthermore, they avoid social activities and prefer isolation, leading to mental and physical complications.
Another theme revealed in this study was the ominous shadow of fear of disease relapse, which was divided into two subthemes, namely (1) the patient’s constant worry and fear of the disease recurrence; and (2) discontinuation of treatment causing the return of psoriasis symptoms. The patients in this study stated that doctors and researchers have pointed out that after the partial treatment of the disease and the improvement of the patient’s symptoms, one-third of the patients will be still at risk of a recurrence of the skin lesions, and in case of insufficient treatment, the symptoms will develop progressively. Therefore, patients were likely to stop treating the disease or did not comply with the treatment protocols.
Following the findings of the present study, Richards et al. showed that psoriasis is a condition that confronts patients with frequent and debilitating physical, psychological, and social complications. Consequently, patients do not often use their medications according to the instructions (25).
The patients in this study complained about the progression of the disease due to inadequate knowledge of the medical staff. They also reported problems, such as doctors’ initial unawareness of the early symptoms of psoriasis, difficulties faced by the patient due to the distance to specialized medical centers in Tehran, wrong diagnoses and deterioration of the disease, and disappointment with the treatment and turning to traditional medicine. A person suffering from psoriasis suddenly faces the disease and its symptoms. The patient is not aware of the disease and has many visits to doctors for treatment. The chronic nature of the disease, the absence of any definitive treatment, and the distance from specialized medical clinics make patients disappointed and lead them to use traditional medicine.
Similar to the findings of the current study, Pariser et al., in a qualitative study, reported financial problems, lack of knowledge and lack of attention to psoriasis by doctors and individuals, failure to find effective treatments, and unpleasant treatments as the main reasons for patients’ failure to adapt to the symptoms (26).
The present study explored psoriasis patients’ experiences and perceptions using a qualitative approach. Given the methodological limitations in this study, its findings might have less generalizability for other groups and populations.
5.1. Conclusions
Research with a quantitative approach has been effective in increasing knowledge about psoriasis. However, following the naturalistic perspective, there is no specific truth, and the truth can be different in each person’s context and life. Therefore, considering the contextual conditions and the lived experiences of psoriasis patients, qualitative studies can help the scientific community and psoriasis patients by proposing new ideas.
The results of the present study showed that the progression of the disease due to inadequate knowledge of the medical staff is an important challenge for patients with psoriasis. Furthermore, the recurrence of the disease can be a serious threat to trust in the current treatments of this disease. Physical and mental suffering can lead to the isolation of patients and makes it very difficult for them to bear the burden of the disease. As a result, psychiatrists, doctors, and nurses should try to raise the patients’ morale and improve body image, self-confidence, and physical care by increasing their awareness of patients’ experiences and understanding their conditions. Considering the new developments in the treatment of skin diseases, the financial and family support of patients will enable them to continue these treatments and obtain desirable outcomes.
5.2. Limitations of the Study
The present study was conducted using a qualitative approach, and the findings revealed the perceptions of patients with psoriasis. These findings have implications for the studied populations but are not perfectly generalizable to other groups. Contrary to these limitations, the patients in this study were selected with maximum variations in terms of age, gender, duration of disease, and disease complications, which could enhance the transferability and generalizability of the findings to similar populations to some extent. In addition, the data were accurately analyzed, and the findings were confirmed by experts in the field.