1. Background
Traumatic brain injury (TBI) is an important health problem and one of the main causes of death and disability worldwide (1). Traumatic brain injury refers to the change in the normal function of the brain due to cerebral pathological lesions secondary to the application of external mechanical forces (2). Predictions show that TBI will continue to be a leading cause of disability due to neurological disorders until 2030 (3). In fact, TBI is known as the most common type of brain damage that causes multiple disabilities in young and middle-aged people (4). In the United States, about 2.8 million cases of TBI occur annually (5). The incidence rate of TBI varies widely in different countries, and its average is 47.3 - 84.9 per 100,000 people per year (6). In Iran, brain injuries rank second in terms of the causes of mortality (7).
Patients with moderate to severe TBI initially need to be admitted to intensive care units (ICUs) (8), where they are exposed to complications such as bed falls, bedsores, deep vein thrombosis, and urinary infections, which persist even after discharge. One of the most common complications, making the patient seek help from family members, is urinary tract infection (UTI) (9-11), as the most common type of infection, accounting for about 40% of hospital-acquired infections in the United States. Odgaard et al. showed that UTIs are among the most common complications in TBI patients (10), which are most commonly associated with the use of urinary catheters and lead to the death of approximately 13,000 patients per year, causing substantial costs for countries (12). Urinary tract infections in TBI patients may also be related to bladder dysfunction (neurogenic bladder), causing urinary retention and urinary incontinence (13). About 65 - 70 % of TUIs caused by catheters can be prevented (14).
Urinary tract infections increase the risk of death and the need for extensive rehabilitation in TBI patients. Rehabilitation in these patients is a long-term process and requires coordination among medical staff. The family is one of the most important pillars of the rehabilitation team and is responsible for the continuation of post-discharge care (9, 15). Urinary tract infections in patients recovering from TBI can be a result of the improper use of urinary catheters by family caregivers. Thus, a nurse-family collaborative program can reduce the incidence of catheter-related UTIs (12, 16). Furthermore, the implementation of home-based educational programs may be effective in reducing the incidence of UTIs (17).
Home-based training is one of the promising educational approaches that can improve family members’ awareness and attitudes regarding the nature and management of TBI by increasing their communication and problem-solving skills (18). Other goals of home-based healthcare include promoting and maintaining patients’ well-being and independence and reducing their disabilities caused by chronic diseases. Face-to-face interactions with the patient and family members and directly training them will further improve the independent functioning of the client. Nowadays, community-oriented rehabilitation models have received considerable attention. Thus, the engagement of the client and family members in home-based healthcare services and training them in this regard will improve the self-care and quality of life of patients. Moreover, among the valuable advantages of home-based healthcare services are their cheapness and effectiveness in comforting patients and reducing the rate of hospitalization (19-22).
Since TBI is a chronic condition, the primary responsibility for long-term care relies on family members; however, most families lack enough knowledge and skills to care for TBI patients. Therefore, it is of crucial importance to improve family caregivers’ awareness and performance in caring for these patients to avoid complications such as UTIs (23-25). Family-oriented care models have received considerable attention due to their cost-effectiveness in comforting patients and increasing their quality of life (19). In addition, traditional educational methods routinely performed in healthcare centers and clinics are not able to respond to all educational needs at home and lead to ineffective self-care behaviors. Thus, training programs to be more effective should be delivered through efficient educational methods. Home-based education for patients with TBI may be effective in reducing complications such as UTIs. As mentioned, home-based education has many benefits for the patient and family members. A review of the literature showed that there was no study on the effects of home-based education on the incidence of UTIs in patients with TBI.
2. Objectives
The present study aimed to investigate the effects of a home-based educational program on the incidence of UTIs in patients with TBI discharged from the hospital.
3. Methods
The protocol for this quasi-experimental study was approved by the Ethics Committee of Zahedan University of Medical Sciences (IR.ZAUMS.REC.1401.032). The participants included 50 patients discharged from the neurosurgery ward of the Khatam Al-Anbia Hospital of Zahedan City in 2022. After obtaining the required permits, the researcher visited the office of the hospital’s manager and received permission to conduct the research. Then arrangements were made with the head of the ward, and TBI patients and their caregivers who met the criteria for enrollment in the study were selected using convenience sampling. The participants were randomly divided into the intervention and control groups.
Inclusion criteria for patients were the diagnosis of TBI confirmed by a neurologist, consciousness level of 8 - 13 (according to the Glasgow coma scale), no urinary infection at discharge, no diabetes, age between 18 - 60 years, being a male, living in Zahedan, and having a Foley catheter or a condom sheet for emptying the bladder. Inclusion criteria for caregivers were being the main caregiver of the patient, being over 18 years old, having literacy, and living in Zahedan. Exclusion criteria for patients were readmission to the hospital during the study, unwillingness to cooperate, and withdrawal during the study. Finally, caregivers in the intervention group who missed more than one training session were also excluded from the study.
The participants were randomly assigned to either of the two study groups using color cards. Fifty cards, 25 red (intervention) and 25 yellow (control) cards, were prepared and arranged randomly. The patients and caregivers who consecutively entered into the study were randomly assigned a card to determine their group membership. According to Rintala et al., taking a 95% confidence interval and 95% test power, the sample size was estimated as n = 13 per group using the following formula (26). Taking into account any probable dropout and in order to improve the study’s rigor, the sample size in each group was estimated to be n = 25 (50 subjects in total).
The researcher provided some instructions about the objectives of the study and research procedures to caregivers in the hospital and invited them to participate in the study. The caregivers were also ensured that participation in the study was voluntary and their information would be kept confidential. Moreover, informed written consent was obtained from the participants, who were also told that they could leave the study at any time they wished, and their withdrawal would have no effect on the treatment process of their patients.
The data were collected using a demographic information questionnaire, and urine culture test results were recorded. The caregivers in the intervention group attended two 45-minute face-to-face training sessions. The first session was held on the second day after discharge and the second session on the fifth day after discharge at the patient’s home (Table 1). In addition, an educational pamphlet was delivered to the caregivers, and an educational video was played for them to show the correct catheterization and catheter care methods. After the last training session, the researcher communicated with the caregivers every two weeks by phone and provided the necessary instructions. Moreover, a phone number was provided to the main caregiver to contact the researcher if they needed any additional information. A urine sample was taken from each patient in the intervention group by a sterile method at the patient’s home and sent to the laboratory to check for UTIs. The patients and caregivers in the control group only received routine training. Similar to the patients in the intervention group, their counterparts in the control group were examined for UTIs after four weeks of hospital discharge.
| Session | Place | Time | Duration | Content |
|---|---|---|---|---|
| 1 | At the patient’s home | Day 2nd after discharge | 45 min | Acquaintance with the patient and caregiver, explaining traumatic brain injury, its complications, and long-term risks for patients |
| 2 | At the patient’s home | Day 5th after discharge | 45 min | Explaining urinary infections and their underlying mechanisms, educating the correct catheterization methods and urinary infection preventive measures |
The Content of the Home-Based Educational Intervention
To collect urine samples, the researcher first wore gloves; the patient’s urinary catheter was clamped for about 30 minutes before connection to the urinary bag, and then the place where the needle entered the catheter was disinfected with 70% alcohol. Twenty mL of urine sample was drawn into a syringe and transferred into a sterile container, which was labeled with the patient’s information and sent to the laboratory in less than half an hour (27). The urine sample was cultured in the laboratory using the calibrated loop method in blood agar and EMB media. The plates were placed in an incubator at 37°C for 48 hours. If no colony grew, the test result was reported as negative, but in the plates in which colonies grew, the number of colonies was determined and multiplied by the volume of the lobe. If the number of colonies was 105 per mL or more, the test result was considered positive, confirming the diagnosis of UTI.
To comply with ethical protocols, all the educational content provided to the participants in the intervention group was also offered to the participants in the control group in the form of a booklet. Moreover, the necessary arrangements were made for all patients to receive a doctor’s visit at the end of the study.
The data collected were analyzed by SPSS 21 software. The independent samples t-test was used to compare quantitative variables between the two groups. Moreover, the Chi-square test was used to compare qualitative variables between the two groups. A significance level of less than 0.05 was considered for data analysis.
4. Results
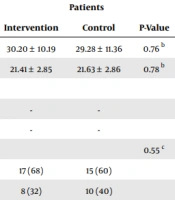
The mean ages of the participants in the intervention and control groups were 30.20 ± 10.19 and 29.28 ± 11.36, respectively. The chi-square test showed no statistically significant difference between the two groups in terms of marital status (P = 0.55). Also, no statistically significant difference was found between the two groups in terms of age, gender distribution, occupational or educational status of the caregiver, and the familial relationship of the main caregiver with the patient (P > 0.05, Table 2).
| Variables | Patients | Caregivers | ||||
|---|---|---|---|---|---|---|
| Intervention | Control | P-Value | Intervention | Control | P-Value | |
| Age (y) | 30.20 ± 10.19 | 29.28 ± 11.36 | 0.76 b | 32.64 ± 11.81 | 31.12 ± 11.18 | 0.64 b |
| BMI (mg/m2) | 21.41 ± 2.85 | 21.63 ± 2.86 | 0.78 b | - | - | - |
| Gender | 0.57 c | |||||
| Male | - | - | 12 (48) | 14 (56) | ||
| Female | - | - | 13 (52) | 11 (44) | ||
| Marital status | 0.55 c | 0.99 d | ||||
| Married | 17 (68) | 15 (60) | 22 (88) | 23 (92) | ||
| Single | 8 (32) | 10 (40) | 3 (12) | 2 (8) | ||
| Occupation | 0.49 d | 0.57 c | ||||
| Employed | 21 (84) | 18 (72) | 13 (52) | 11 (44) | ||
| Unemployed | 4 (16) | 7 (28) | 12 (48) | 14 (56) | ||
| Education | 0.99 c | 0.77 c | ||||
| Lower education | 17 (68) | 17 (68) | 14 (56) | 15 (60) | ||
| Higher education | 8 (32) | 8 (32) | 11 (44) | 10 (40) | ||
| Relationship with the patient | 0.58 c | |||||
| Spouse | 9 (36) | 10 (40) | ||||
| Parent | 7 (28) | 4 (16) | ||||
| Other | 9 (36) | 11 (44) | ||||
Comparing the Demographic Characteristics of Patients and Caregivers Between the Two Groups a
Overall, 28% of patients in the intervention group were positive for UTIs compared to 64% of patients in the control group. The chi-square test showed a statistically significant difference between the two groups in terms of the incidence of UTIs (P = 0.01, Table 3).
| Group Unitary Infection | Intervention | Control | Chi-square |
|---|---|---|---|
| Positive | 7 (28) | 16 (64) | χ2 = 6.52; df = 1; P = 0.01 |
| Negative | 18 (72) | 9 (36) | |
| Total | 25 (100) | 25 (100) |
Comparing Urinary Tract Infections in Patients Between the Two Groups After the Intervention a
5. Discussion
The findings of the present study showed that the frequency of UTIs was lower in the patients whose caregivers received the educational intervention than in the control subjects, revealing a significant difference between the two groups in terms of the incidence of UTIs. Thus, home-based education was effective in reducing the incidence of UTIs in patients with TBI. Similarly, Cardenas et al. investigated the effects of a training program on the incidence of UTIs in patients with spinal cord injuries and confirmed the effectiveness of the educational program in reducing urinary infections in these patients (17). Moreover, Mosavi et al. investigated the effectiveness of home care education for parents according to the health belief model in reducing the recurrence of urinary infections in children and reported that home care education reduced the incidence of UTIs in children (28). The empowerment of family members and patients is of particular importance in nursing practice as a requirement for boosting patients’ health. In fact, involving the family caregiver in caring for the patient can play an important role in improving the patient’s condition.
In line with the findings of the present study, Ahmed and Shehata showed that the implementation of a catheter care training program reduced the incidence of urinary infections in patients carrying urinary catheters (29). Likewise, we here observed that training TBI patients regarding correct catheterization and urinary catheter care methods could be effective in preventing UTIs. In addition, face-to-face interactions between patients and their family members, as those primarily responsible for providing patient care at home, and direct and unmediated training them further improve the patient’s independent functioning.
Nevertheless, some studies have reported contradictory results compared to our observations in the present study. Lee et al., who investigated the effects of implementing a collaborative training program for nurses and families on the self-efficacy of family caregivers in preventing UTIs in patients with urinary catheters, declared that the incidence of urinary infections was lower in the patients of the intervention group than those in the control group; however, this difference was statistically insignificant (16). Most likely, this contradicting finding can be attributed to differences in the number and duration of the training sessions, as well as the fact that Lee et al. evaluated the patients five days after implementing the intervention (16). Another important difference was that the training intervention in the current study was carried out at home (i.e., in the patient’s real-life environment), which could increase the effectiveness of the training program and the compliance of the patients and their caregivers, boosting the effectiveness of the intervention in reducing the incidence of UTIs.
Since patients with TBI have multiple and often long-term disabilities, raising family caregivers’ and patients’ awareness seems to be an effective strategy for preventing and controlling the complications of the disease. Given that TBI is a chronic condition, the main responsibility for long-term care rests with family members, who, in most cases, are devoid of adequate knowledge and skills to care for patients. Thus, home-based education is an effective method to prevent catheter-related complications in these patients.
Overall, studies have indicated that the implementation of educational programs can be effective in preventing and reducing the occurrence of urinary infections in patients carrying catheters. The findings of the present study also showed that home-based education played an important role in preventing UTIs in patients with TBI discharged from the hospital.
Addressing the limitations of this study, the main caregiver sometimes changed during the study, which could have affected the results. In addition, some of the caregivers could have obtained information from other sources, which could also have downplayed our interpretation regarding the effectiveness of the home-based educational intervention.
5.1. Conclusions
Regarding the findings of the present study, training family caregivers at home can be one of the effective, simple, low-cost, and uncomplicated ways to reduce UTIs in patients with TBI. Thus, home-based education should be incorporated into nursing care to reduce urinary infections in patients with TBI. Future studies are recommended to investigate the effectiveness of this intervention on larger samples.