1. Background
Traumatic brain injury (TBI) is an acquired brain tissue injury caused by an external force with different intensities from mild to severe, leading to a change in the patient’s level of consciousness (1). Traumatic brain injury is one of the major health problems worldwide (2). Men between the ages of 15 and 19 are 3 times more likely to develop TBI than women. Additionally, children, young adults, and older adults aged 75 and above are also at an increased risk for TBI. Approximately 155 000 cases of TBI are reported annually in individuals aged 65 years and above; this age group tends to have higher rates of hospitalization and mortality due to TBI (3-5).
One of the main complications of TBI is coma. Coma is a state of unconsciousness where a person is unresponsive without opening the eyes and cannot speak and obey orders (6). Recent medical advances and improvements in care services have increased the survival rate of TBI patients, but these advances have not guaranteed the return of patients to their pre-disease state. Thus, TBI patients are hospitalized for a long time in intensive care units (ICUs) (7). In addition, admission to ICUs, its associated challenges, and fear of the unknown ICU environment can cause instability of patients’ vital signs, deteriorating the patient’s level of consciousness (8). Furthermore, anxiety caused by admission to the ICU increases the heart rate and worsens the respiratory condition and body temperature changes of the patients (9). Deterioration of vital signs affects all body systems, including cardiovascular and respiratory systems (10).
Patients admitted to ICUs experience physiological stress, followed by changes in the heart rate, breathing rate, and blood pressure (11). Following these conditions and depending on the symptoms and complications caused by the loss of consciousness, the patient may receive other drugs for hemodynamic stabilization (blood pressure, heart rate, and breathing) and control the struggle with the ventilator. All these drugs affect organs such as the kidney, liver, and lungs and impair their function. Given the side effects of pharmaceutical methods used to impact the level of consciousness of trauma patients, non-pharmaceutical methods that have fewer side effects can be used for these patients. One of these methods is the use of complementary medicine, which involves aroma therapy, sound stimulation, touch therapy, foot reflexology massage, and familiar sensory stimulation.
Reflexology massage is one of the holistic health methods that involves applying pressure and massage on specific points. In many countries, reflexology massage plays an important role in the non-drug treatment of patients. Reflexology massage aims to remove the blockages, release the flow of energy, and ultimately cure the disease (12). On the other hand, sensory deprivation in the ICU is one of the threatening complications of comatose patients. Sensory stimulation is a treatment method that aims to reduce the risk of sensory deprivation and facilitate the recovery of various responses in trauma patients (13). Sensory stimulations can include hearing, sight, smell, taste, and touch stimulations. The start of sensory stimulations in the first 72 hours after a brain injury is very important in saving the patient, improving the quality of life, and reducing the length of hospitalization (14). Research has shown that sensory stimulation, especially if applied from the beginning of the patient’s admission, can shorten the average length of stay and reduce the patient’s anxiety (15). Creating sensory stimulations for the trauma patient is part of essential nursing care in the ICU. Moreover, the presence of the family members next to the patient admitted to the ICU can be a suitable source for creating these sensory stimulations (16, 17). For this purpose, encouraging the family members to engage in the sensory stimulation program enables them to participate in patient care and contributes to faster improvement of the patient’s cognitive status and a better prognosis due to the familiarity of these stimulations for the patient (13, 14, 18). Bahonar et al. showed that foot reflexology massage increased the level of consciousness of patients and reduced the duration of coma (19). Moreover, Hasanzadeh et al. showed that familiar and early sensory stimulations increased the level of consciousness of TBI patients (20). Azimian et al. also showed that foot massage increased the level of consciousness of comatose patients with TBI, and thus it can be used to increase the level of consciousness of comatose patients (21).
The use of safe and effective complementary medicine techniques (such as foot reflexology massage and familiar sensory stimulation by family members for TBI patients, in contrast to the extensive use of drugs that have many physical and psychological side effects) can stabilize hemodynamic indicators, increase the level of consciousness, reduce the intensity of pain, anxiety, and stress, increase the speed of recovery, and reduce the length of stay. Such techniques have been recommended in many studies.
2. Objectives
Given the shortage of nursing staff and time constraints to perform complementary medicine methods (such as reflexology massage) and also considering the possibility of familiar sensory stimulation interventions by the patient’s family members, it is necessary to compare these 2 methods to determine which method is more effective. Besides, since no study has addressed the effect of these 2 methods on the level of consciousness, the present study aimed to compare the effect of foot reflexology massage and familiar sensory stimulation on the level of consciousness of TBI patients admitted to the ICUs of Khatam Al-Anbia Hospital affiliated with Zahedan University of Medical Sciences in 2021.
3. Methods
This quasi-experimental study was approved by the Ethics Committee of Zahedan University of Medical Sciences (code: IR.ZAUMS.REC.1400.334). This study was conducted with a pretest-posttest design on 135 TBI patients with an altered level of consciousness and under ventilation admitted to the ICUs of Khatam Al-Anbia Hospital in Zahedan. The sample size was estimated as 29 persons per group based on the mean consciousness score in a similar study (20), with 95% CI and 90% statistical test power using the following formula:
Since there were 3 groups of patients in the study, the estimated sample size was multiplied by 1.4. Thus, 40 patients were considered in each group. To ensure the adequacy of the sample size and considering a 10% dropout rate, 45 persons were selected in each group (135 persons in total) (20).
Inclusion criteria were a Glasgow Coma Scale (GCS) score of 7 to 10, an age range of 15 to 75 years, pupillary light reflex, no hearing impairment, and absence of any lower limb amputation, wound, or fracture that would restrict the performance of foot reflexology massage, being at 24 to 48 first hours after stabilization of hemodynamic symptoms, the performance of the intervention when receiving the minimum dose of sedatives, narcotics, and benzodiazepines according to the order of the anesthesiologist, absence of underlying disease (diabetes, cardiovascular disease, history of coma in the past, sensory and neurological disorders, embolic symptoms, fat and skin disease), and non-addiction. In addition, the inclusion criteria for the main caregiver were a first-degree member of the patient’s family who had a greater share in the care of the patient (father, mother, spouse, child, and siblings), regular and constant presence of the main caregiver during the intervention hours, emotional stability of the family member, and having minimum literacy to read and write.
Exclusion criteria were a decrease in the consciousness level to less than 7 based on the GCS during the study, the unwillingness of the patient’s guardian or caregiver to continue participating in the study, the patient’s transfer to the operating room for surgery, discharge from the ICU before the completion of the intervention, or the patient’s death.
Data were collected using a personal information form (age, sex, marital status, and education), a disease information form (a history of hospitalization or underlying disease), and GCS. The validity and reliability of the GCS for patients admitted to ICUs have been confirmed in different studies (22, 23).
The eligible patients were randomly assigned to 3 groups (control, foot reflexology massage, and familiar sensory stimulation groups) through a lottery. To this end, the group membership for each patient was determined by randomly removing a color card from a container. Before starting the interventions, the researcher provided some instructions to the main caregivers about the objectives of the study and obtained informed consent from them. After obtaining written and informed consent from the legal guardians of the patients, the level of consciousness of the patients was measured and recorded using the GCS. During the intervention in the foot reflexology massage group, the patient lay on their back while the researcher sat in a chair in front of the patient's feet to perform the massage. Any metal objects, such as rings, were removed, and lubricant gel was used for smoothness and ease of massage. After warming the hands, a gentle massage was performed to warm the feet. Then, the heel of the foot was held with the left hand and was bent from the ankle area and then straightened; this movement was performed for about a minute. Next, direct pressure was applied with the thumb to the suitable points on the foot. The points related to the head and brain are located in the area of the arch of the foot. The massage was performed for 15 minutes for each foot (a total of 30 minutes). The massage was performed by the researcher using thumbs in the form of circular movements and applying pressure of about 10 - 12 kg. To ensure that the pressure was equivalent to 10 kg, the researcher applied pressure on the scale several times before doing the task.
The intervention in the familiar sensory stimulation group was performed by a member of the patient’s family who was trained. After receiving the necessary instructions (such as wearing gowns and slippers and washing hands for 3 to 5 minutes before entering and after leaving the ICU), the main caregiver attended the patient’s bedside with the researcher next to the patient after the prior arrangement with the patient’s nurse. On the first visit (24 - 48 hours after the patient’s admission), when the main caregiver’s mental and emotional conditions got stable, the researcher explained to him/her how to perform the sensory stimulation intervention as follows: Introducing the caregiver the patient, informing the patient of the time and place, narrating happy memories, reading/reciting the Quran, praying, reading the patient’s favorite book/poetry, playing music using headphones, touching the patient during the care, combing the patient’s hair, cutting their nails, moisturizing the patient’s lips, cleaning the patient’s nose and eyes with moist sterile gauze, and rubbing softening cream on the patient’s hands and feet. The intervention was carried out for 30 to 45 minutes. The level of consciousness was measured 5 minutes before and 30 minutes after the intervention that was performed twice a day (morning and evening) for 1 week. The control group received ICU routine care, and the frequency and intervals of measuring the level of consciousness of the patients were the same as those of the intervention groups.
Data analysis was performed using SPSS version 22 (SPSS Inc, Chicago, IL, USA). P values less than 0.05 were considered statistically significant. The data were summarized using descriptive statistics, including percentage, frequency, mean, and SD. The normality of the data was first checked and confirmed using the Shapiro-Wilk test. Thus, the data analysis was performed using the paired samples t-test, independent samples t-test, analysis of variance (ANOVA), analysis of covariance (ANCOVA), and chi-square test.
4. Results
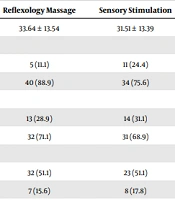
The results of ANOVA showed that there was no significant difference in average age between the 3 groups. Moreover, there was no statistically significant difference in the frequency of gender, marital status, education, and underlying diseases between the 3 groups (Table 1).
| Variables | Reflexology Massage | Sensory Stimulation | Control | P Value |
|---|---|---|---|---|
| Age | 33.64 ± 13.54 | 31.51 ± 13.39 | 33.51 ± 14.29 | 0.63 b |
| Gender | 0.14 c | |||
| Female | 5 (11.1) | 11 (24.4) | 12 (26.7) | |
| Male | 40 (88.9) | 34 (75.6) | 33 (73.3) | |
| Marital status | 0.96 c | |||
| Single | 13 (28.9) | 14 (31.1) | 14 (31.1) | |
| Married | 32 (71.1) | 31 (68.9) | 31 (68.9) | |
| Education | 0.26 d | |||
| Illiterate | 32 (51.1) | 23 (51.1) | 20 (44.4) | |
| Primary school | 7 (15.6) | 8 (17.8) | 17 (37.8) | |
| Middle school | 12 (26.7) | 12 (26.7) | 8 (17.8) | |
| Diploma and higher education | 3 (6.6) | 2 (4.4) | ||
| Underlying diseases | 0.43 d | |||
| Yes | 0 (0) | 0 (0) | 0 (0) | |
| No | 0 (0) | 0 (0) | 0 (0) |
a Values are expressed as No. (%) unless otherwise indicated.
b ANOVA.
c Chi-square.
d Monte Carlo.
As can be seen in Table 2, the ANOVA results showed a statistically significant difference in the level of consciousness between the 2 intervention groups and the control group both before (P = 0.001) and after the intervention (P = 0.001). Furthermore, the paired-samples t-test indicated that the average level of consciousness in the foot reflexology massage group was found to be significantly different after the intervention compared to before the intervention (P = 0.003). Similarly, the average level of consciousness in the sensory stimulation group was found to be significantly different after the intervention compared to before the intervention (P < 0.001). However, there was no significant difference in the control group in terms of the average level of consciousness, as there was no intervention (P = 0.185).
| Groups | Pre-intervention | Post-intervention | Paired t-Test |
|---|---|---|---|
| Reflexology massage | 9.55 ± 1.77 | 9.63 ± 1.75 | t = 3.14; P = 0.003 |
| Sensory stimulation | 8.75 ± 1.49 | 9.01 ± 1.53 | t = 6.75; P = 0.001 |
| Control | 7.73 ± 1.78 | 7.74 ± 1.78 | t = -1.35; P = 0.185 |
| ANOVA | F = 13.1; P = 0.001 | F = 14.5; P = 0.001 |
Abbreviation: ANOVA, analysis of variance.
The Tukey post hoc test showed a significant difference in the average level of consciousness between the control and reflexology massage groups and between the control and familiar sensory stimulation groups, but no statistically significant difference was observed between the 2 intervention groups. However, the average score of the level of consciousness after the intervention was higher in the foot reflexology massage than in the familiar sensory stimulation group, but there was no significant intergroup difference. After the intervention, the intensity of changes in the level of consciousness of the patients in both foot reflexology massage and familiar sensory stimulation groups showed a statistically significant difference compared to the level of consciousness of the patients in the control group.
Following the data from the Shapiro-Wilk test (statistic = 977; P = 0.09) and Levene test (F = 1.02; P = 0.21), the establishment of assumptions of approximate normality and homogeneity of variances, and the establishment of the assumption of regression homogeneity showing the non-significance of the interaction between the independent and dependent variables, the requirements for using ANCOVA were met. The result of ANCOVA to control the significant effect of the consciousness level scores in the pretest showed that the consciousness level of the patients in all 3 groups had statistically significant differences after the intervention (P = 0.001; Table 3).
| Source of Changes | Sum of Squares | df | Mean Squares | F | Sig. | Eta Square | Test Power |
|---|---|---|---|---|---|---|---|
| Pretest | 375.80 | 1 | 375.80 | 13298.75 | 0.001 | 0.99 | 1 |
| Group | 1.27 | 2 | 0.63 | 22.58 | 0.001 | 0.25 | 1 |
| Error level | 3.7 | 131 | 0.02 | ||||
| Total | 10889 | 135 |
5. Discussion
The findings of the present study showed that the level of consciousness of TBI patients increased after the foot reflexology massage and familiar sensory stimulation interventions, and both interventions were effective in improving the level of consciousness of intubated patients with altered levels of consciousness. Although the average score of the level of consciousness after the intervention was higher in the foot reflexology massage than in the familiar sensory stimulation group, there was no significant intergroup difference. The significant difference in the level of consciousness of the patients in the 3 groups before the intervention could be attributed to the fact that the patients were randomly selected from 3 different ICUs, and thus there were some differences in the medical diagnosis of the patients, quality of treatments, and care, which unfortunately were not under the control of the researcher.
The findings of the present study are in line with the results reported in several studies. For instance, Salmani et al. investigated the effects of family-centered affective stimulation on the level of consciousness of brain-injured comatose patients; they showed that family-centered affective stimulation significantly improved the level of consciousness of patients, leading the researchers to recommend the incorporation of familiar sensory stimulation into the nursing care program for these patients (22). In addition, Adinehvand et al. examined the impact of sensory excitation performed by family members and nurses on the level of consciousness in patients admitted to the ICU, showing that sensory excitation was more effective by family members than nurses in improving the level of consciousness of comatose patients (6). A clinical trial study by Hasanzadeh et al. showed that familiar sensory stimulation increased the level of consciousness of patients with brain injuries admitted to the ICU (20). All these studies confirmed that familiar sensory stimulation, especially if it is performed by family members or a person familiar with the patient, can improve the level of consciousness of patients. Moreover, the consistency of the results could be attributed to the similarity in the target population (patients with an altered level of consciousness) and the type of intervention (familiar sensory stimulation). An increase in the level of consciousness is suggested as an indicator of improvement in the course of the disease in critically ill patients, especially after brain lesions; thus, any type of care and intervention that leads to an increase in the level of consciousness of these patients can improve the patient’s prognosis (20).
A systematic review study showed that family-oriented primary sensory and emotional stimulation is more effective than routine care and sensory stimulation by nurses in improving the level of consciousness and awareness of comatose patients with brain injuries, and multisensory stimulation is more effective than single stimulation (23).
Some studies have confirmed the effect of foot reflexology massage on the level of consciousness of intubated patients. In a clinical trial study, Bahonar et al. examined the effect of foot sole reflexology massage on the level of consciousness and hemodynamic indicators of 60 patients with traumatic coma. The results showed that foot reflexology massage increased the level of consciousness of patients and reduced the duration of coma (19). Moreover, Azimian et al. also examined the effect of foot massage on the consciousness level in comatose patients with brain injury hospitalized in the ICU, showing that foot massage can significantly increase the level of consciousness of comatose patients with brain injury. Thus, foot massage can be used to increase the level of consciousness of comatose patients (21). The results of the above study are consistent with the findings of the current study. However, in the above study, both legs were massaged by the stroke method (each leg for 5 minutes) once a day for 14 days, showing some differences from the present study.
Moreover, as confirmed in the present study, Ahmadi et al. confirmed the effectiveness of foot tactile stimulation on the level of consciousness and physiological parameters in comatose patients admitted to the ICU (24). In their study, the intervention involved touching the ankle without applying any pressure. It was performed twice a day (in the morning and evening) for 10 minutes each time, over a period of 3 consecutive days. The intervention used in their study differed from the foot reflexology massage used in the present study. Cole believes that foot massage stimulates nerve fibers and skin layers containing touch and pressure receptors (which transmit nerve impulses to the brain). Thus, it can be concluded that foot massage can increase the level of consciousness in patients with an altered level of consciousness (25).
One of the limitations of the present study is the effect of sedative drugs on the level of consciousness of patients, which could affect the results of the study, but it was out of the researcher’s control.
5.1. Conclusions
The use of complementary medicine, including familiar sensory stimulation and foot reflexology massage, increases the level of consciousness of TBI patients, but none of them is superior to the other. The researchers suggest that nurses use these 2 complementary medicine methods, which do not have the side effects of pharmaceutical methods, to improve the level of consciousness of comatose patients under ventilators admitted to ICUs. Moreover, revising ICU visitation restrictions can contribute to the positive effects of family presence at the patient’s bedside.