1. Background
More than 80 - 90 percent of hospitalized patients are treated intravenously, and more than 500 million peripheral vein catheters are placed annually (1). Despite the importance and benefits of intravenous injections, they may lead to several complications, such as phlebitis, thrombophlebitis, thrombosis, and local pain. Intravenous fluid therapy in children is sensitive and important due to their metabolism rate, the ratio of body surface to weight, premature renal excretion, and the sensitivity of blood circulation, and one of its most common complications is phlebitis (2).
Phlebitis, as a serious complication of intravenous injection, is an inflammation of the inner layer of blood vessels, which is accompanied by pain, and if it occurs, the vein should not be used again (3). The symptoms of phlebitis include visible red streaking along with a rope- or cord-like and painful vein that may remain for several days to several weeks. One of the most important risk factors for phlebitis is antibiotics, accounting for 63 percent of the total phlebitis (4). Roszell and Jones showed that antibiotic treatment was the most predictive factor of phlebitis in 1054 peripheral vein catheter samples, and out of every 5 patients with a peripheral vein catheter, 1 with antibiotic prescription developed phlebitis (5).
The prevalence of phlebitis varies depending on the factors influencing the occurrence of this complication, which include the choice of vein, the choice of catheter, the procedure, the venous site, and the care process during intravenous fluid therapy. The child's age is also influential; the younger the child, the higher the incidence of complications, which are more common and dangerous in infants. The American Nursing Association defines an acceptable prevalence of phlebitis as 5 percent or less (6). However, its actual prevalence in some communities is higher than the acceptable rate reported by the American Nursing Association, and the overall prevalence of this complication is reported as 25% to 35% (7). According to a study by Macklin in 2003, the occurrence of phlebitis ranges from 27% to 70% (8).
Pain is one of the complications of phlebitis due to catheterization. Pain is an unpleasant sensory and emotional experience associated with active or potential tissue damage and is present whenever a person expresses it (9). Paying attention to pain relief in children is very important, and failure to address pain relief leads to negative consequences in eating, sleeping habits, self-confidence, fear, depression, and despair, and disrupts the child's development (10). Pain leads to the release of chemical hormones, which subsequently cause complications in body systems and death (11).
Previous studies have shown that children who have been repeatedly hospitalized and underwent painful procedures in the first six months of life and whose pain has not been adequately relieved suffer from physical, behavioral, and social disorders in their childhood (12). Pharmacological treatments are an important part of pain relief treatments (13). Although drug therapy is the most powerful tool available to nurses for pain relief, it is not the only available intervention. Non-pharmacological nursing measures cause fewer complications and can effectively relieve the patient’s pain (14). Nurses should consider the control of phlebitis and the pain caused by it, and the failure to address it has consequences such as septicemia, increased length of stay and treatment costs, and even the death of the patient. Thus, treating phlebitis and pain caused by venous catheters in children using non-pharmacological methods should be one of the nursing priorities. Applying Aloe vera gel and warm compresses is one of the non-pharmacological nursing procedures.
Aloe vera is a plant from the Liliaceae family that grows in tropical regions and has anti-inflammatory, immunomodulating, moisturizing, anti-aging, and antiseptic effects (15). Anggraeni et al. compared the effect of Aloe vera compress and 70% alcohol on 42 Indonesian children from 1 month to 7 years old with phlebitis. They showed that Aloe vera significantly reduced the degree of phlebitis compared to 70% alcohol (16). The pain relief effect of Aloe vera is likely due to its anti-inflammatory chemical compounds called anthraquinones, which reduce swelling and promote healing and pain relief when applied to the skin (17).
In addition to the immediate removal of the catheter for the treatment of phlebitis, warm and moist compresses can be used to increase blood flow, cause faster recovery of phlebitis, and reduce the pain caused by it. Annisa et al. examined the effect of warm water compresses on the degree of phlebitis in Indonesia and showed that warm water compresses effectively reduce the degree of phlebitis (18). In addition, Hariati showed the positive effect of warm compresses on the pain of older adults with rheumatoid arthritis (19).
Phlebitis in hospitalized children has a high prevalence, and phlebitis caused by venous catheters can cause stress, fear, and pain. It does not receive adequate attention, and the recovery process of phlebitis usually takes a relatively long time. Thus, there is a need for an alternative treatment method to facilitate its recovery. Furthermore, few studies have addressed phlebitis in children in Iran. In addition, no study has compared the effect of Aloe vera and warm compresses on the pain caused by phlebitis in children in Iran.
2. Objectives
The present study aims to compare the effectiveness of Aloe vera and warm compresses applied to the pain caused by phlebitis in children admitted to the pediatric wards in Ali Ibn Abi Talib Hospital in Zahedan in 2022.
3. Methods
This three-group, single-blind clinical trial study was conducted on a sample of children admitted to the Ali Ibn Abi Talib Hospital pediatric ward in Zahedan. The inclusion criteria were the absence of underlying diseases such as diabetes, asthma, and skin diseases and not receiving vancomycin. The exclusion criteria were discharged from the hospital three days before the start of the intervention, unwillingness to continue cooperating in the study, failure to use Aloe vera compress or warm compress during the study, and the patient’s critical condition for any reason.
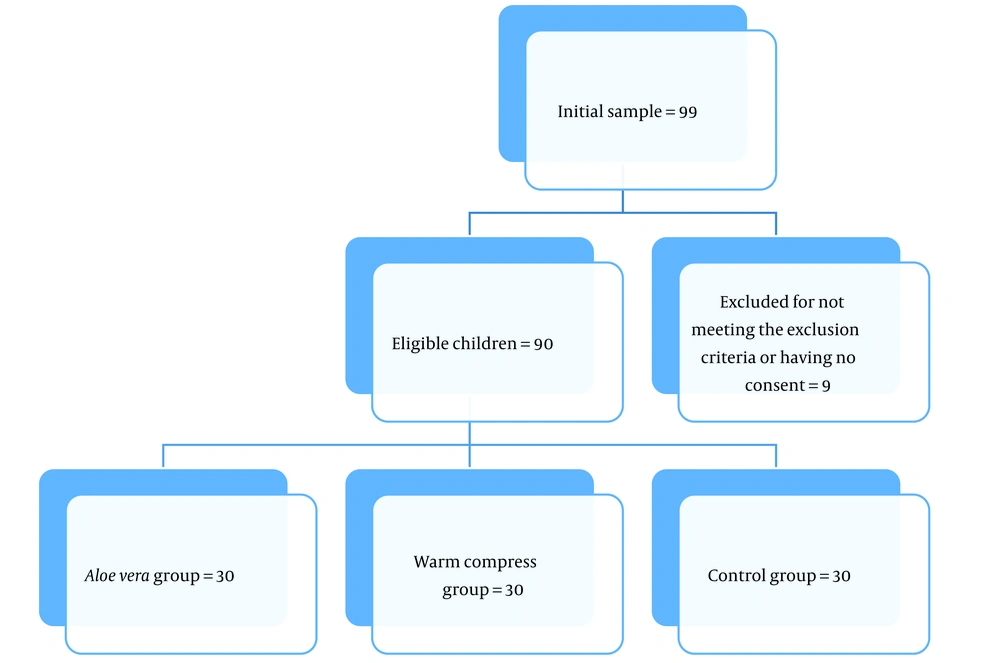
The sample size was estimated as 19 patients per group based on the mean and standard deviation of the degree of phlebitis (Haji Hosseini et al., (20)), considering a 95% confidence interval, and 85% test power, using the following formula. Following similar studies and given the probable dropout, a total of 90 patients were selected as the participants in the study (30 patients in each group) (Figure 1).
Z1-α/2 = 1.96, S1= 0.45, μ = 1.20, Z1-β = 1.03, S2 = 0.9, μ = 0.7.
Before conducting the study, 90 children aged 3 - 8 years who had phlebitis caused by a peripheral vein catheter and met other criteria were selected through convenience sampling. Then, in the second stage, the selected children were randomly divided into three groups: Control, Aloe vera compress intervention, and warm compress intervention groups. For this purpose, 90 colored cards (30 blue colored cards for the Aloe vera intervention group, 30 red colored cards for the warm compress intervention group, and 30 yellow cards for the control group) were placed in a box. Then, each child's mother picked out a colored card from the box with her eyes closed, and the child was assigned to a group based on the color of the card. The pain intensity was first measured for the children in the control group. The parents of all children in the three groups received the necessary instructions about the study's objectives and the research procedure.
The data in this study were collected using a patient demographic information questionnaire and Wong-Baker Faces Pain Rating Scale. The demographic information questionnaire contained 5 items that measured the child's gender, age, current diseases, and any underlying illnesses and skin diseases. The Wong-Baker Faces Pain Rating Scale was developed in 1988 and consists of a card with 6 emoticons marked with a numerical scale (from laughing to crying). The patient, who is usually 3 - 8 years old, chooses one based on the pain's intensity. Then, the intensity of pain is calculated by the researcher. The score range on the scale varies from 0 (no pain) to 10 (severe pain).
The validity and reliability of the Wong-Baker Faces Pain Rating Scale has been confirmed in several studies (21-23). The Persian version of this scale has been used in several studies (24, 25). Nikfarid et al. estimated the correlation coefficient for the scale as equal to 0.82, confirming its validity (24). The scale's reliability was assessed in the present study using inter-rater reliability and was confirmed with a coefficient of 0.79. The demographic information questionnaire was completed by interviewing the parents and using the data in patients’ medical records. Moreover, the pain intensity was measured using the Wong-Baker Faces Pain Rating Scale, and the related values were recorded in a form. The equipment used in this study consisted of a heat gel pack, Aloe vera gel (Kaman Brand, Seilaneh Sabz Company), cotton bandage, sterile gauze, and a digital thermometer.
Before starting the intervention, the pain intensity in the children was measured and recorded using the Wong-Baker Faces Pain Rating Scale. Then, after disinfecting the phlebitis site, a sterile gauze was soaked in 5 cc of Aloe vera gel, drawn with a syringe, and placed on the child’s phlebitis site in the Aloe vera group, and the place was covered with a bandage for 20 minutes.
In the warm compress group, first, the heat gel pack (model 810 or Sina Hakim) was placed in the microwave for 30 - 60 seconds at a temperature of 800 W (according to the manufacturer’s instructions). Then, the pack was gently taken out with gauze, and its temperature was checked with a digital thermometer to be 37 - 38 degrees Celsius. The pack was covered with sterile gauze and placed on the phlebitis site for 20 minutes. No intervention was performed for the children in the control group, and no special routine procedure was performed to reduce pain caused by phlebitis. Simultaneously with the other two groups, the pain scores for the patients in the control group were measured and recorded.
Pain intensity was measured for the children in the three groups before and after the interventions. The interventions were repeated by the researcher every 12 hours for 3 days. The researcher recorded the pain score every 12 hours before the intervention and on the first, second, and third days. Six interventions were performed for the children in the Aloe vera and warm compress groups. The researcher repeated all intervention times. Pain intensity was recorded and assessed in the pre-intervention stage for the children in all three groups. It was also measured for the warm compress group half an hour after the intervention and for the Aloe vera group at the beginning of the intervention. Data analysis was performed using a blind procedure by a person who knew nothing about the interventions and the groups.
Data analysis was performed using SPSS-22 software. First, the normality of the data was checked using the Shapiro-Wilk test, and since the data followed a normal distribution pattern, parametric tests, including the chi-square test, independent samples t-test, one-way analysis of variance (ANOVA), and Fisher’s exact test were run at a significance level of less than 0.05 (P < 0.05). The present study was conducted based on a research proposal approved with code IR.ZAUMS.REC.1401.059 by the Zahedan University of Medical Sciences and Medical Services Ethics Committee. This research project was registered with the IRCT code (IRCT20220427054677N1) in the Iranian Registry of Clinical Trials.
4. Results
The average age of the children in the warm and Aloe vera compress groups was 5.93 ± 1.70 and 5.57 ± 1.83 years, and that of the participants in the control group was 6.10 ± 1.72 years. The ANOVA results showed no significant difference between the three groups regarding age (P = 0.48). Table 1 shows the descriptive statistics for the participants’ gender and diseases in the three groups:
| Categories | Frequency (%) | Fisher’s Exact | ||
|---|---|---|---|---|
| Warm Compress | Aloe vera Compress | Control | ||
| Gender | P = 0.957 | |||
| Male | 15 (50) | 15 (50) | 14 (47) | |
| Female | 15 (50) | 15 (50) | 16 (53) | |
| Disease | P = 0.656 | |||
| Gastrointestinal problems | 5 (16.66) | 14 (46.66) | 5 (16.66) | |
| Fracture and infection | 14 (46.66) | 10 (33.34) | 16 (53.34) | |
| Internal diseases | 11 (36.68) | 6 (20.00) | 9 (30.00) | |
| Total | 30 (100) | 30 (100) | 30 (100) | |
The Descriptive Statistics for the Participants’ Gender and Diseases
The results of Fisher’s exact test showed no statistically significant difference between the three groups in terms of the patient’s gender and diseases (P > 0.05) (Table 2).
| Groups | Mean ± SD | P-Value (ANOVA) | ||
|---|---|---|---|---|
| Warm Compress | Aloe vera Compress | Control | ||
| Pain intensity | ||||
| Pre-intervention | 6.67 ± 1.67 | 6.73 ± 1.73 | 6.33 ± 1.58 | 0.59 |
| First day | 6.0 ± 1.81 | 5.67 ± 1.66 | 6.0 ± 1.57 | 0.67 |
| Second day | 4.53 ± 1.73 | 3.87 ± 1.73 | 4.93 ± 1.46 | 0.04 |
| Third day | 3.93 ± 1.70 | 2.73 ± 2.31 | 6.47 ± 1.45 | 0.002 |
The Descriptive Statistics for Pain Intensity in the Patients
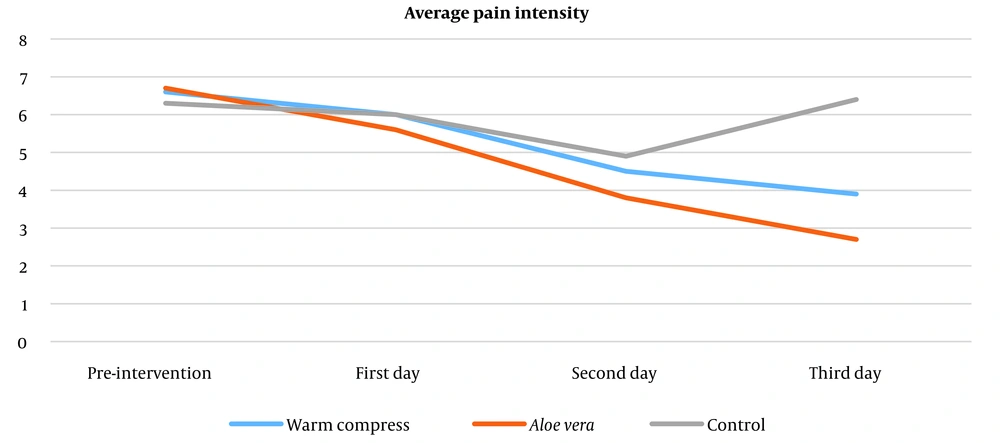
The results of the one-way ANOVA indicated that the average pain intensity scores before the intervention (P = 0.59) and on the first day (P = 0.67) did not have a statistically significant difference between the three groups. However, the average pain scores between the three groups on the second (P = 0.04) and third (P = 0.002) days after the intervention showed a significant statistical difference. Moreover, the data from Tukey’s post hoc test confirmed a statistically significant difference on the second day between the Aloe vera group and the control group (P = 0.001) and on the third day between the Aloe vera group with the warm compress group (P = 0.03) and the control group (P = 0.001). Indeed, the pain intensity in the Aloe vera group decreased more significantly than in the warm compress group and the control group (P = 0.001) after the intervention, as shown in Figure 2.
5. Discussion
This clinical trial study compared the effectiveness of Aloe vera and warm compresses in pain caused by phlebitis in children admitted to the pediatric wards of Ali Ibn Abi Talib Hospital in Zahedan in 2022. The results indicated that both warm and Aloe vera compresses reduced the intensity of pain caused by phlebitis. However, the average pain intensity score in the Aloe vera group decreased more than the warm compress group, which was significant in the Aloe vera compression group compared to the warm compress group on the third day of the intervention. A review of the literature revealed no study comparing these two interventions. Nevertheless, related studies are discussed in this section.
Zheng et al. examined the effectiveness of Aloe vera in the prevention and treatment of phlebitis caused by injection and showed that Aloe vera, either alone or in combination with conventional treatment, is more effective than conventional treatment in improving phlebitis symptoms, including less time for eliminating swelling and redness and less time to relieve pain at the site of intravenous injection. The difference between this study and the present study was in the research sample. The present study was conducted on children, while Zheng et al.’s study was conducted on patients of different ages. The authors also compared the effect of Aloe vera with other treatments, such as alcohol and magnesium sulfate (MgSO4). In contrast, the present study compared the effects of Aloe vera and warm compresses. However, despite these differences, the two studies reported similar findings (26).
A meta-analysis study by Ali and Wahbi on the effectiveness of Aloe vera in the management of oral lichen planus indicates that although corticosteroids are still the gold standard, Aloe vera shows promising results, especially since Aloe vera has no specific side effect compared to various adverse effects of corticosteroids (27). Anggraeni et al. compared the effect of Aloe vera compress and 70% alcohol on 42 children from 1 month to 7 years old with phlebitis admitted to a West Java, Indonesia, healthcare center. The results showed that Aloe vera significantly reduced the pain caused by phlebitis by 70% compared to alcohol. This study was similar to the preset study in terms of the research sample and the type of intervention. It demonstrated the effectiveness of Aloe vera in reducing the pain caused by phlebitis. However, this study compared the effect of Aloe vera and 70% alcohol (16).
The effectiveness of Aloe vera is likely due to its internal ingredients. Aloe vera contains anti-inflammatory substances such as lignin, saponin, anthraquinone complex, asmenan, bradykinase enzyme, tannin, alectin A, amino acids, vitamins, and salicylate. Lignin can be used as a topical treatment because it can be absorbed into the skin. In addition, Aloe vera is analgesic because it prevents the migration of neutrophil cells into inflamed vein tissues, thus inhibiting the inflammation process. Amino acids, glycoprotein, and aloemodin in Aloe vera accelerate the growth of new cells in the process of regeneration of the epithelium of blood vessels (28).
The findings from the present study showed that warm compresses are also effective in reducing phlebitis pain. Hence, the reduction of pain intensity in the warm compress group compared to the control group was significant on the second day of the intervention. This finding was also in line with the results reported in previous studies. Warm moist compress is a low-risk and uncomplicated method that reduce pain and inflammation by dilating blood vessels and increasing blood supply to the target area (29). Jourabloo et al. (29) compared the effect of warm compress and calendula ointment on pain caused by phlebitis on 96 patients hospitalized at the surgical departments in a hospital in Tehran and found that both interventions reduced pain, but calendula ointment was more effective than work compress. This study was different from the present study in terms of the research sample and the type of intervention compared with warm compresses. However, in line with the present study, the findings confirmed the effectiveness of warm compresses in reducing pain caused by phlebitis (30). Furthermore, the present study found that the reduction in pain intensity on the third day of the intervention was less in the warm compress group than in the Aloe vera group, indicating that the warm compress is less effective than Aloe vera.
In a study conducted at the University of Sumatra in Indonesia, Hariati confirmed the effect of warm compresses on pain intensity in older adults with rheumatoid arthritis. This study differed from the present study regarding the research sample and the type of pain in the patients. However, in line with the results of the present study, it confirmed the effectiveness of warm compresses in reducing pain intensity (19). Heat deactivates the nerve fibers that cause muscle spasms and can cause the release of endorphins, which block the transmission of pain, such as very strong opioids. In general, blood flow increases in body parts that are heated because heat relaxes the blood vessel walls, and heat is effective in increasing flexibility (30).
Overall, the present study showed that although both warm and Aloe vera compresses reduced the pain caused by phlebitis, Aloe vera compress was more effective than warm compress in reducing pain intensity. Aloe vera contains 75 potentially active compounds, including vitamins, enzymes, minerals, sugars, and amino acids, some of which have multiple medicinal properties (31).
5.1. Conclusions
The findings of the present study showed that the application of warm and Aloe vera compresses reduced the pain intensity caused by phlebitis in children, but the application of Aloe vera compresses resulted in a greater reduction in pain intensity compared to warm compresses. Thus, Aloe vera compresses can be applied as an easy and uncomplicated method to reduce the pain caused by phlebitis.