1. Background
Sleep is one of the basic physiological needs of human life and is a regularly recurring and easily reversible state that is characterized by immobility and a significant increase in the response threshold to external stimuli compared to the awake state (1, 2). Sleep plays an essential role in restoring physical and mental strength (3).
Hospitalization causes disturbances in the sleep pattern and decreases the quality of sleep (4, 5). Sleep also plays a vital role in the growth and repair of damaged cells. Therefore, enough sleep and rest in hospitalized patients will play a very important role in the process of health and recovery from the disease (6). Recent surveys of patients and nurses have always shown a decrease in the quantity and quality of sleep of patients admitted to hospitals (7, 8). Researchers believe that patients admitted to intensive care units (ICUs) need more sleep for recovery and survival than healthy individuals (9), and they have implemented numerous drug and non-drug treatments to improve the quality of sleep in these patients (10-13).
Given the side effects of sleep medications, other techniques with fewer complications and side effects can be used to improve patients’ quality of sleep. One of the non-pharmacological procedures is to limit noise and ambient light using eye masks and earplugs as a nursing intervention (14, 15). Richardson conducted the first study to investigate the combined effect of two non-pharmacological interventions, eye masks, and earplugs and showed that a cheap and affordable intervention could be applied to improve the quality and length of sleep in hospitalized patients (16). Furthermore, several interventions, such as drug therapy (12, 17, 18), aroma therapy (19), earplugs and eye masks (20, 21), relaxation techniques (22), massage therapy (23), and music therapy (24), have been applied to reduce the negative impact of factors disturbing the sleep of ICU patients.
Massage is another effective technique for improving patients’ quality of sleep and has many advantages (25). Swedish massage is known as one of the best massage therapy techniques that mainly aims to relax the entire body (26). Swedish massage is very useful for increasing blood oxygen levels, reducing muscle toxins, and improving blood flow and flexibility. A study by the National Center for Complementary and Alternative Medicine showed that individuals who received 45 minutes of Swedish massage therapy had a significant decrease in stress hormone levels and cortisol and an increase in serotonin. One of the causes of insomnia is a lack of serotonin in the body (27). Serotonin produces the hormone melatonin, which is very effective in preparing the body to experience a comfortable and deep sleep (28). By increasing the serotonin hormone in the body, massage helps a person to experience comfortable and quality sleep (27). Kashani and Kashani showed that the use of massage techniques improves the health and sleep quality of patients, and massage therapy can be applied as a non-pharmacological procedure to improve sleep quality in patients (23).
The available evidence shows that fewer studies have addressed the effects of non-pharmacological interventions in patients admitted to the ICU. For instance, Wang et al. and Hu et al. reported that the main non-pharmacological interventions in ICU patients include the use of eye masks and earplugs (29, 30). Moreover, in their review study, Jagan and Park examined the effect of massage on the quality of sleep in ICU patients and showed that the intervention was effective (25). Nevertheless, Kawabata et al. examined the effect of massage on patients and showed that the quality of sleep was not improved by massage therapy (31). However, very few studies have addressed the effects of massage on the quality of sleep. Therefore, given that massage is likely to be effective in improving the quality of sleep of patients and the use of eye masks and earplugs as common noise reduction and light control techniques, the present study aimed to compare the effectiveness of Swedish massage and earplugs and eye masks in the quality of sleep of patients admitted to ICUs of hospitals in Zahedan, Iran, in 2022.
2. Methods
This quasi-experimental study was conducted on two groups of ICU patients using a pre-test-post-test design. The research protocol was approved by the Ethics Committee of Zahedan University of Medical Sciences (IR.ZAUMS.REC.1401.093). The participants were 40 patients admitted to the ICUs of hospitals affiliated with Zahedan University of Medical Sciences in 2022. The participants were selected from all adult patients admitted to the ICUs of Khatam Al-Anbia and Ali Ibne Abi-Talib hospitals in Zahedan in 2022.
Following a similar study (Ebrahimi Tabas et al.) (32) and using the following formula, the sample size was estimated as 18 subjects per group with a 95% confidence interval and 95% test power. However, given the possibility of the participants’ dropout, the sample size was considered 20 subjects per group (40 participants in total) as follows:
The criteria for enrolment in the study were being alert and aware of time and place (the Glasgow Coma Scale [GCS] ≤ 12), absence of hearing and vision disorders, absence of history and habit of using eye masks and earplugs, absence of drug use at night, and non-prohibition of massage for the patient. The exclusion criteria were the occurrence of acute problems during the study and the transfer of the patient to other wards. Participants’ personal and clinical data were collected using a questionnaire that assessed information about age, gender, marital status, education, occupation, patient's marital status, underlying disease(s), APACHE II score, pain intensity, medication use, and history of sleep disorders. These data were collected through interviews with the patients and were recorded in their medical files.
Richards-Campbell Sleep Questionnaire (RCSQ) is a 5-item visual analog scale (33). The questionnaire scores vary from 0 to 100 (0 = worst possible sleep and 100 = best possible sleep), and the total scores range from 0 to 500 (34). The questionnaire was translated into Persian by Amirifar et al., and its validity and reliability were confirmed. The inter-rater reliability coefficient and Cronbach’s alpha were 0.714 and 0.906, respectively (35). In this study, the reliability of the tool was assessed again and confirmed with an inter-rater reliability coefficient of 0.89.
After making the necessary arrangements, the researcher went to the neonatal intensive care units (NICUs) and checked the patients’ level of consciousness. She invited the patients who met the inclusion criteria to participate in the study. The researcher also provided some instructions to the patients about voluntary participation in the study and the confidentiality of their information. Then, the patients eligible to enter the study were selected through convenience sampling. In the next step, the selected patients were randomly placed in two intervention groups (Swedish massage and earplugs/eye masks) using colored cards. First, the demographic information questionnaire and RCSQ were completed for the participants through interviews with them. After enrollment in the study, the patients in both groups did not receive any intervention during the first night, and their sleep quality was checked using the RCSQ on the first night as a pre-test. The participants in both groups received the intended interventions on the second night after entering the study, and their sleep quality on the second night was measured as a post-test.
The patients in the Swedish massage group were placed in the supine position one night for 20 minutes before bedtime, and the massage was given by a trained researcher for 20 minutes from 10:00 p.m. using special ointment on the back (the lumbar cavity to the shoulder). The depth and pressure exerted on the patient’s body were different according to the patient’s body tissue and muscle tone. The researcher had received the required training for 150 hours (from the Iran Technical and Vocational Training Organization). Moreover, the patients in the earplug/eye mask group were asked to wear earplugs and eye masks for one night from 10:00 p.m. to 6:00 a.m. They were also told to remove the earplugs/eye masks for a while in case of any difficulty or inconvenience and wear them again. The questionnaires were completed through interviews with the patients in both groups for two consecutive days after 6 a.m. The sleep quality of the patients on the first night after entering the study was considered the baseline scale.
Data analysis was performed using SPSS software (version 26). The data were summarized using descriptive statistics, including mean and standard deviation. The Shapiro-Wilk test was run to check the normality of the data. The paired samples t-test was used to compare the mean of quantitative variables in each group before and after the intervention and the independent t-test was used to compare the mean of quantitative variables between the two groups. The chi-square test was also run to compare qualitative variables between the two groups. All statistical procedures were conducted at a significance level of less than 0.05 (P < 0.05).
3. Results
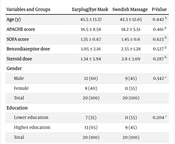
The results of the study indicated that the participants in the earplug/eye mask and Swedish massage groups had no significant differences in terms of age, gender, education, marital status, occupation, underlying diseases, sleep disorder, pain intensity, APACHE score, sequential organ failure assessment (SOFA) score, and benzodiazepine and steroid dosage, as shown in Table 1.
| Variables and Groups | Earplug/Eye Mask | Swedish Massage | P-Value |
|---|---|---|---|
| Age (y) | 45.5 ± 13.37 | 42.3 ± 12.65 | 0.442 b |
| APACHE score | 16.5 ± 8.58 | 18.2 ± 5.51 | 0.461 b |
| SOFA score | 1.35 ± 0.67 | 1.45 ± 0.6 | 0.623 b |
| Benzodiazepine dose | 1.05 ± 2.16 | 2.55 ± 1.28 | 0.527 b |
| Steroid dose | 1.34 ± 3.94 | 2.8 ± 3.69 | 0.287 b |
| Gender | 0.342 c | ||
| Male | 12 (60) | 9 (45) | |
| Female | 8 (40) | 11 (55) | |
| Total | 20 (100) | 20 (100) | |
| Education | 0.204 c | ||
| Lower education | 7 (35) | 11 (55) | |
| Higher education | 13 (65) | 9 (45) | |
| Total | 20 (100) | 20 (100) | |
| Marital status | 1 c | ||
| Single | 8 (40) | 8 (40) | |
| Married | 12 (60) | 12 (60) | |
| Total | 20 (100) | 20 (100) | |
| Occupation | 0.185 d | ||
| Employed | 15 (75) | 11 (55) | |
| Unemployed | 5 (25) | 9 (45) | |
| Total | 20 (100) | 20 (100) | |
| Underlying diseases | 0.429 c | ||
| Yes | 15 (75) | 14 (70) | |
| No | 5 (25) | 6 (30) | |
| Total | 20 (100) | 20 (100) | |
| Sleep disorders | 0.465 d | ||
| Yes | 15 (75) | 13 (65) | |
| No | 5 (25) | 7 (35) | |
| Total | 20 (100) | 20 (100) | |
| Pain intensity | 0.341c | ||
| No or mild pain | 10 (50) | 13 (65) | |
| Moderate and severe pain | 10 (50) | 7 (35) | |
| Total | 20 (100) | 20 (100) |
Comparison of the Demographic and Clinical Characteristics of Patients in 2 Groups a
The results showed that mean sleep quality scores for the participants in the Swedish massage and earplug/eye mask groups were 130.25 ± 41.91 and 135 ± 44.36 before the intervention, respectively. Furthermore, the mean sleep quality scores for the participants in the Swedish massage and earplug/eye mask groups were 202 ± 46.03 and 184.79 ± 39.5 after the intervention, respectively, showing a significant increase in the mean sleep quality score in each group after the intervention as confirmed by the paired samples t-test (P = 0.001). In addition, the mean sleep quality score for the participants in the Swedish massage group was significantly higher than that of the participants in the earplug/eye mask group after the intervention (P = 0.037). The mean differences in the sleep quality scores for the participants in the Swedish massage and earplug/eye mask groups were 71.79 and 49.79, respectively. Therefore, there was a significant difference in the sleep quality scores between the Swedish massage and earplug/eye mask groups after the intervention, as confirmed by the independent samples t-test (P = 0.002) (Table 2).
| Stages and Groups | Pre-intervention | Post-intervention | Mean Difference | Paired Samples t-Test | ||
|---|---|---|---|---|---|---|
| t | df | P | ||||
| Earplug/eye mask | 135 ± 44.36 | 184.79 ± 39.5 | 49.79 ± 24.5 | 9.195 | 19 | 0.001 |
| Swedish massage | 130.25 ± 41.91 | 202 ± 46.03 | 71.79 ± 33.5 | 0.718 | 19 | 0.001 |
| Independent samples t-test | t = 0.348; df = 38; P = 0.73 | t = 2.15; df = 38; P = 0.037 | t = 3.34; df = 38; P = 0.002 | |||
Comparison of Mean Sleep Quality Scores in Two Groups Before and After the Intervention a
4. Discussion
The findings of the present study showed that both earplug/eye mask and Swedish massage interventions improved the sleep quality of patients admitted to the ICU; nevertheless, the patients in the Swedish massage group reported a significantly greater improvement in their sleep quality than the patients in the earplug/eye mask group. This finding implies that the Swedish massage technique was more effective than wearing earplugs and eye masks in improving the sleep quality of ICU patients.
Similarly, some studies have reported an improvement in sleep quality in individuals wearing earplugs and eye masks. For instance, Arab et al. compared the effect of using eye masks and earplugs on the sleep quality of patients in the coronary care unit (CCU) and showed that the average scores of sleep quality were significantly different in the three groups after the intervention and concluded that eye masks and earplugs improve sleep; nevertheless, earplugs have the strongest effect (36), as confirmed in the present study. However, the present study did not address the effects of eye masks and earplugs separately, and they were compared with the Swedish massage technique. In line with the present study, Dehghani et al. examined the effect of wearing eye masks and earplugs on the quality of sleep of patients admitted to the ICU and showed that the intervention improved the quality of sleep of the patients (37). This study examined the effect of these two interventions separately and in two intervention groups; however, the present study assessed the effectiveness of earplugs and eye masks as a single intervention.
Consistent with the findings of the present study, Sharafi et al. investigated the effect of the simultaneous use of earplugs and eye masks at night on the quality of sleep of patients admitted to the ICU. The results showed a statistically significant difference in the sleep quality scores reported by the patients in both groups before and after the intervention (38). Furthermore, Le Guen et al. investigated the sleep quality of patients one night after surgery with and without sound (earplugs) and light (eye masks) protection in the post-anesthesia care unit. In the aforementioned study, 46 patients without any neurological or respiratory failure underwent minimally invasive heart surgery. The patients randomly slept in the recovery room on the first night after surgery with or without earplugs and eye masks. The findings showed that earplugs and eye masks during the first night after surgery prevented a decrease in sleep quality, compared to standard care (20), as evident in the present study. Although the aforementioned study is different from the present study in terms of the research sample, it still demonstrated the effect of interventions to reduce environmental stimuli to improve sleep quality.
Hu et al. investigated the effects of earplugs and eye masks combined with relaxing music on sleep, melatonin, and cortisol levels in ICU patients. In this study, 45 patients admitted to the ICU were selected and randomly divided into the intervention group (n = 20) and the control group (n = 25). The findings showed a significant difference between the groups in the depth of sleep, falling asleep, waking up, sleeping again after waking up, and the overall quality of sleep. Perceived sleep quality was also better in the intervention group (21). In a clinical trial study, Chaudhary et al. evaluated and compared the effect of earplugs and eye masks against ocean sound on the sleep quality of ICU patients. The findings confirmed a significant change in the sleep quality score, indicating that the sleep quality score improved after using earplugs and eye masks and listening to ocean sounds. The least significant difference (LSD) post hoc test also showed a significant difference in the intervention groups. Earplugs and eye masks were more effective in improving the quality of sleep than the ocean sound (39).
Babaii et al. examined the effect of aromatherapy with damask rose and blindfold on the sleep quality of patients admitted to cardiac critical care units. The findings indicated that the overall sleep quality of the patients was significantly improved after the intervention in both the damask rose and blindfold groups. Furthermore, the patients in the blindfold group reported a greater improvement in their sleep quality than the patients in the damask rose group (40). Overall, previous studies (e.g., Hu et al.; Chaudhary et al.; Babaii et al. (21, 30, 39, 40) confirmed that earplugs/eye mask intervention is more effective in improving sleep quality than aromatherapy and music intervention, and it seems that reducing light and noise can increase the quality of sleep in patients by using eye masks and earplugs. Therefore, patients in the ICU who are exposed to unfavorable environmental stimuli, such as light and noise, need higher-quality sleep as it helps reduce irritability, aggression, and pain in these patients.
Massage is another non-pharmacological intervention effective in improving patients’ sleep quality and has various advantages (25). Similarly, the present study showed that Swedish massage is more effective and useful than earplugs/eye mask intervention in improving patients’ sleep quality. Moreover, a study by the National Center of Medicine demonstrated that individuals who receive 45 minutes of Swedish massage therapy experience a significant reduction in stress hormone (i.e., cortisol) and the production of arginine, which can lead to an increase in cortisol and serotonin. One of the causes of insomnia is the lack of serotonin in the body (27). Serotonin produces melatonin, which is very effective in preparing the body to experience a comfortable and deep sleep (28). By increasing serotonin in the body, massage helps a person experience comfortable and quality sleep (27).
Accordingly, Kashani and Kashani reported that learning and applying massage techniques as a non-pharmacological method improves the health and sleep quality of patients (23). Alinia-Najjar et al. examined the effect of foot reflexology massage on burn-specific pain anxiety and sleep quality and quantity of patients admitted to the burn ICU. The trend of different days in each group was compared with Friedman’s test, and the results showed a significant difference in sleep delay, sleep duration on the last day, and satisfaction with the last night’s sleep in burn patients in the two intervention and control groups. Moreover, the quality of sleep increased significantly in the intervention group (41).
In their clinical trial study, Raiesifar et al. investigated the effect of superficial backstroke massage on the quality of sleep and anxiety of stroke patients. The results showed a statistically significant difference in the total score of sleep quality and other dimensions of sleep quality, except for the two dimensions of subjective quality of sleep and sleep disorders (8). In a quasi-experimental study on 105 burn patients, Rafii et al. showed that the anxiety and sleep quality were significantly different in patients in three groups (control, massage, and massage combined with aromatic oil) after the intervention, and the sleep quality in the massage group was higher than the two other groups, as evident in the present study. Although the participants were different in the two studies, they confirmed the effectiveness of massage therapy (42).
In their systematic review study based on a focused literature search (PubMed, CINAHL, Scopus, EMBASE-Ovid, and Google Scholar), Jagan and Park investigated the effect of massage on the outcomes of adult ICU patients. The findings indicated that 8 of 12 studies used randomized control designs with high internal validity, and there was strong evidence of the effectiveness of massage in pain and anxiety reduction. The results showed that the massage intervention can have a positive effect on the outcomes of critically ill patients (25).
A systematic review and meta‐analysis by Fang et al. confirmed the effect of massage therapy on the sleep quality of critically ill patients. The findings indicated that massage therapy, especially foot reflexology, for two nights improves sleep quality in critically ill patients (43). This finding is consistent with the data in the present study. However, a study by Ghanbari et al. on 90 hemodialysis patients showed that immediately after the intervention, restless leg syndrome and sleep quality in the foot reflexology group were significantly better than in the Swedish massage group (44). Contrary to the findings of the present study, Kawabata et al. compared the effect of massage and aromatherapy on the quality of sleep in the palliative care ward and observed that massage and aromatherapy do not affect the quality of sleep and fatigue of patients in the palliative care ward (31). As one of the shortcomings in the present study, some environmental conditions and factors in the ICU that were beyond the researcher’s control could affect the results.
4.1. Conclusions
According to the findings of the present study, it can be argued that earplugs, eye masks, and Swedish massage as non-pharmacological interventions can have a significant effect on improving the sleep quality of patients admitted to the ICU. Furthermore, Swedish massage can be more effective than earplugs and eye masks and have a greater effect on increasing the sleep quality and quantity in ICU patients. Therefore, patients admitted to the ICU who suffer from sleep disorders can benefit from Swedish massage therapy. Moreover, healthcare managers can hold massage training courses for healthcare and medical staff to empower them to apply massage interventions in ICUs.