1. Background
Cardiovascular diseases are the leading cause of death and the fifth cause of disability worldwide, accounting for 25 - 45% of all deaths. Heart failure, a type of cardiovascular disease, was responsible for 75% of the common causes of death globally in 2020 (1). Approximately 5.1 million Americans are affected by this disease, with 825 000 new cases reported annually (2). In Iran, the prevalence of heart failure is estimated at 3 500 cases per 100 000 individuals, three times higher than in the United States. Despite this, the number of patients with heart failure is expected to rise due to the aging population and advances in treatment that reduce mortality (3). Evidence indicates that patients with heart failure endure numerous physical, psychological, emotional, and spiritual challenges. Additionally, family members caring for these individuals encounter numerous difficulties (4). These challenges significantly impact patients' daily activities and their personal and social lives (5). Moreover, frequent hospitalizations and increased mortality rates among these patients are consequences of the myriad issues they face (6). Considering the high rate of hospital admissions and readmissions for heart failure (7), this condition places a considerable financial strain on both the patients and healthcare systems (8). Like other chronic illnesses, heart failure cannot be cured, and most treatments aim to manage the disease. A key component of managing heart failure is focusing on treatment adherence, which is often poor among these patients, exacerbating the condition's outcomes.
Treatment adherence encompasses a patient’s behavior in accordance with care instructions and advice. This includes attending scheduled programs on time, fully utilizing medications, monitoring the disease, and implementing necessary changes in health behaviors. Adhering to treatment recommendations can significantly reduce the acute and chronic complications of the disease, thereby preventing these complications. However, more than 50% of patients demonstrate inadequate treatment adherence (9). Patients with heart failure encounter numerous challenges in following treatment and self-care guidelines. While hospitalized, the direct oversight of doctors and nurses ensures full compliance with treatment and care instructions, with medical care being thoroughly administered under nurse supervision. Yet, post-discharge, adherence to medication and dietary regimens often changes, potentially leading to serious complications such as increased treatment costs, re-hospitalization, worsening clinical conditions, and even death. Therefore, patients with heart failure must understand the importance of lifelong treatment adherence to avoid severe consequences. Lack of treatment adherence represents a potentially modifiable behavior. Research in the USA has indicated that 20 to 64% of rehospitalizations among heart failure patients are due to non-adherence or poor adherence to medication (10).
Treatment adherence in heart failure patients can be influenced by several factors, including patient self-efficacy. Self-efficacy, a crucial predictor of a broad spectrum of health-promoting behaviors against diseases, was defined by Bandura in 1977.
According to Bandura, the sense of self-efficacy is a critical precursor to behavioral change. Self-efficacy is deemed an essential determinant of behavior because it operates as an independent component of an individual's basic capabilities. Therefore, patients who are confident in their ability to perform self-care are more likely to engage in self-care behaviors (11). To enhance heart failure patients' awareness and understanding of their medication regimen and, consequently, to maximize adherence, it is vital to employ effective training methods for these patients. While training programs for cardiovascular patients often emphasize behavioral change and encourage adherence to medication and medical directives, they sometimes overlook the importance of ensuring patients feel capable of maintaining lifestyle changes and medication adherence for life (12). Self-efficacy-based training represents one of the intervention strategies capable of yielding positive outcomes in patients. Indeed, self-efficacy-based training might enhance treatment adherence among heart failure patients, potentially leading to a reduction in patient rehospitalization rates. Thus, substituting traditional training approaches with interventions that boost self-efficacy appears to be a logical and effective strategy for modifying behaviors, lowering hospitalization rates among heart failure patients, and improving treatment compliance. In this context, nurses play a pivotal role in patient education. Self-efficacy-based training interventions primarily focus on medication adherence. However, the efficacy of such interventions has been less explored in heart patients.
2. Objectives
Considering the importance of investigating variables, such as treatment adherence and its deficiencies in heart failure patients, this study aimed to assess the impact of self-efficacy training on treatment adherence among patients with heart failure admitted to teaching hospitals affiliated with Zahedan University of Medical Sciences in 2021.
3. Methods
Upon receiving ethical approval (IR.ZAUMS.REC.1399.468) from the Ethics Committee of Zahedan University of Medical Sciences, this quasi-experimental study was undertaken with 70 heart failure patients admitted to the coronary care and cardiac intensive care units of Khatam Al-Anbiah (PBUH) and Ali Ibne Abi Talib (PBUH) hospitals in 2021. Drawing from a previous study [Kamrani et al., (12)], the sample size was determined to be 34 individuals per group, considering a 95% confidence interval and a 90% statistical power, according to the following formula. Ultimately, the sample size was set at 35 individuals per group, totaling 70 participants.
Following the project's approval and after obtaining an introduction letter from the Vice-Chancellor for Research and Technology, the researcher visited the designated hospital units to brief the hospital officials on the study's objectives and research procedures. Participants were then selected through convenience sampling based on the inclusion criteria from among those patients who were willing to participate and had signed an informed consent form. The selected patients were randomly allocated to the control and intervention groups using blue and red cards, which indicated each patient's group assignment.
The inclusion criteria for this study were a physician-diagnosed heart failure, at least 24 hours post-admission, an age range of 30 to 75 years, absence of speech, hearing, and visual impairments, basic literacy, an ejection fraction (EF) of 15 to 40% as determined by ECG results, no history of mental disorders, and neither the patient nor family members being employed in the medical profession. The exclusion criteria included failure to participate in more than one training session and failure to receive the training content. Data were gathered using a demographic information questionnaire (covering age, gender, frequency of hospital admissions, smoking status, and underlying diseases) and the Treatment Adherence Scale. This scale comprises three subscales: Adherence to the dietary regimen, adherence to the activity pattern, and adherence to the medication regimen. Developed by Heydari et al. at Mashhad Nursing and Midwifery College, the scale's content validity has been confirmed. Additionally, reliability correlation coefficients for the subscales on adherence to the dietary regimen, adherence to the activity pattern, and adherence to the medication regimen were 0.86, 0.91, and 0.95, respectively (13). In this study, the tool's reliability was verified using Cronbach’s alpha, resulting in a coefficient of 0.86. After dividing the patients into intervention and control groups, the demographic information questionnaire and the Treatment Adherence Scale were completed for all participants. Subsequently, the self-efficacy-based training intervention was implemented for the intervention group, while the control group received standard training. The training content was formulated based on authoritative sources and tailored to meet self-efficacy objectives.
The training intervention emphasized vascular risk factors, the repercussions of non-compliance, and the advantages of adhering to treatment, lifestyle modifications, medications, cessation of smoking, selection of low-fat foods, exercise, and stress management employing self-efficacy strategies. The program was delivered to heart failure patients through individual, face-to-face sessions, individual counseling, question-and-answer segments, and verbal encouragement. Starting 24 hours post-admission, the training content and self-efficacy enhancement strategies were introduced over four consecutive days in the coronary care unit. This was achieved using slides and an educational booklet prepared by the researcher in the presence of the patient and a family member. Each session lasted between 30 and 45 minutes. Prior to the intervention, an individual needs assessment was conducted for each patient to tailor the training content to their specific educational needs. The content addressed lifestyle changes (healthy nutrition, risk factor modification, symptom management, stress management) on the first day and medication administration on the second day. On the third day, participants viewed a video detailing medication types, mechanisms of action, and potential side effects like bleeding, diarrhea, rash, decreased heart rate, and blood pressure. In the final session, treatment adherence was encouraged by having patients in the intervention group maintain a diary to log their medication intake, diet, and physical activities.
The training content across all four sessions also emphasized self-efficacy enhancement strategies:
(1) Patients were provided with instructions on the essential skills and abilities needed to successfully change behavior and modify cardiovascular risk factors. Responsibilities were delegated to the patients to bolster treatment adherence, emphasizing that they are their own best caregivers through adherence to medication and dietary regimens and engagement in independent physical activity.
(2) A family member was encouraged to partake in the training, goal setting, and problem-solving to aid in achieving treatment objectives and lifestyle modifications. Patients were guided to develop an action plan for themselves with the assistance of a family member and the researcher and to share their newfound knowledge with their families. Learning skills were leveraged for behavioral change, drawing on the successful experiences of others who have managed vascular risk factors well. Patients successful in certain aspects of disease management were introduced to each other to facilitate mutual learning.
(3) The researcher fostered friendly relationships with the patients, allocating ample time to address their queries.
(4) Individual, achievable goals were established to stimulate the patients' enthusiasm and mitigate the impact of past failures in modifying risk factors.
(5) Efforts were made to ensure patients knew they could seek help when necessary and to maintain the momentum of the training provided. To this end, patients' phone numbers were collected, and they were given the researcher's contact information. The patients' daily activities and medication adherence were monitored through a diary and telephone follow-ups as part of the treatment adherence program.
(6) A family member was involved in every training session as a vital support resource. When patients successfully implemented the strategies discussed, they received encouragement, and in instances of failure, tailored training was provided as needed.
After completing the training intervention, a weekly telephone call was made to each patient in the intervention group for three months to remind them of the training instructions and to monitor their adherence to these instructions. The treatment adherence scale was administered three months post-intervention for patients in both groups. At the study's conclusion, the control group also received the training instructions, and each was given a training booklet. Data analysis was conducted using SPSS 26 software. Descriptive statistics (frequency, mean, and standard deviation) summarized the data. The chi-square test evaluated the qualitative variables' independence or dependence, and the independent samples t-test compared the contextual variables between the two groups. Additionally, the chi-square test assessed the quantitative variables. The Shapiro-Wilk test verified data normality. The significance level for this study was set at less than 0.05 (P < 0.05).
4. Results
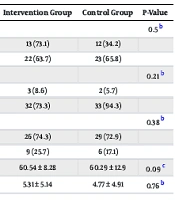
This study involved 70 patients with heart failure admitted to the coronary care and cardiac intensive care units of Khatam Al-Anbiah (PBUH) and Ali Ibne Abi Talib (PBUH) hospitals in Zahedan. The patients were divided into control (n = 35) and intervention (n = 35) groups. Parametric tests were utilized for data analysis. The average age of the patients was 60.54 years in the intervention group and 60.29 years in the control group. The independent samples t-test revealed no significant difference in the average age between the two groups (P = 0.09). The data indicated that the majority of patients in both groups were married, with the chi-square test showing no significant difference in marital status between the groups (P = 0.5). Moreover, no statistically significant differences were found between the groups regarding hospitalization history (P = 0.76), smoking habits (P = 0.21), and underlying diseases (P = 0.38) (Tables 1 and 2).
| Variables and Categories | Intervention Group | Control Group | P-Value |
|---|---|---|---|
| Gender | 0.5 b | ||
| Male | 13 (73.1) | 12 (34.2) | |
| Female | 22 (63.7) | 23 (65.8) | |
| Smoking | 0.21 b | ||
| Yes | 3 (8.6) | 2 (5.7) | |
| No | 32 (73.3) | 33 (94.3) | |
| Underlying diseases | 0.38 b | ||
| Yes | 26 (74.3) | 29 (72.9) | |
| No | 9 (25.7) | 6 (17.1) | |
| Age | 60.54 ± 8.28 | 60.29 ± 12.9 | 0.09 c |
| Number of admissions | 5.31 ± 5.14 | 4.77 ± 4.91 | 0.76 b |
a Values are expressed as No. (%) or mean ± SD.
b Chi-square test.
c Independent samples t-test.
| Group | Pre-intervention | Post-intervention | Paired Samples t-Test |
|---|---|---|---|
| Intervention | 49.74 ± 9.76 | 70.37 ± 8.49 | P = 0.001; df = 34; t = -12.16 |
| Control | 47.34 ± 7.85 | 49.40 ± 8.85 | P = 0.99; df = 34; t = 3.54 |
| Independent samples t-test | P = 0.28; df = 68; t = 1.13 | P = 0.001; df = 68; t = 9.85 |
Before the intervention, the mean scores for treatment adherence in the intervention and control groups were 49.74 ± 9.763 and 47.34 ± 7.851, respectively, and after the intervention, they were 70.37 ± 8.94 and 49.40 ± 8.85. The paired samples t-test indicated a significant increase in treatment adherence scores for patients in the intervention group post-intervention compared to pre-intervention (P = 0.001), whereas the control group showed no significant change in treatment adherence scores before and after the intervention (P = 0.993). Additionally, the independent samples t-test demonstrated significant differences in the mean treatment adherence scores between the two groups after the intervention (P = 0.001).
5. Discussion
The results of this study indicate that the self-efficacy-based training intervention significantly enhanced treatment adherence among patients with heart failure when compared to the control group. Similarly, Moeini et al. validated the impact of a family-oriented educational program on the treatment adherence of patients with heart failure (1). The focus in that study was on family-oriented education, whereas in our study, a family member participated in all the self-efficacy training intervention sessions. The success of these interventions in improving treatment adherence in heart failure patients underscores the critical role that family member involvement plays in educational programs for managing heart failure as a chronic condition. Additionally, Falahinia et al. found that patient education with family participation was more effective in enhancing adherence to the treatment regimen than individual education alone (14). Peyman et al. investigated the influence of education based on self-efficacy theory on self-care behaviors in heart failure patients, observing a significant difference in self-care scores between the intervention and control groups post-intervention (15). Aslani et al. assessed the impact of an empowerment program on self-efficacy in 56 patients with acute coronary syndrome at Imam Khomeini Hospital in Pol-e Dokhtar, Lorestan province, noting a significant improvement in self-efficacy-based self-care behaviors between the two groups by the end of the program, which aligns with the findings of the current study (16).
Gallagher et al. demonstrated that treatment adherence was suboptimal among all patients, even when they were aware of being monitored (17). Similarly, Dunbar et al. found that patients' medication adherence did not improve following an intervention. One reason for these differing results could be the duration of follow-up; in Dunbar et al.'s study, follow-up and assessment occurred 4 and 8 months post-intervention, potentially diminishing adherence to treatment plans over time (18). Therefore, given the long-term treatment required for patients with heart failure, repeated training sessions could be highly beneficial, underscoring the importance of comprehensive education for this patient population. Previous studies employing various intervention strategies to enhance treatment adherence in heart patients have mostly found these methods to be effective in improving adherence levels. Educational interventions can thus motivate patients to more effectively engage in recommended behaviors and adhere to their treatment and medication regimens. A limitation of the current study was the reliance on self-reported questionnaires for data collection, which may be influenced by the psychological, emotional, and physical states of the patients, potentially impacting their responses and, consequently, the study's findings.
5.1. Conclusions
The results of this study indicate that a self-efficacy-based training program can significantly enhance treatment adherence among patients with heart failure. Therefore, the development and implementation of self-efficacy-based training interventions, which are cost-effective and encourage participation from heart failure patients, can lead to improvements in patient outcomes.