1. Background
Cancer is a chronic disease that has accounted for a significant proportion of deaths in various communities over recent decades (1). According to the World Health Organization (WHO), the number of new cancer cases is projected to increase to 26 million worldwide by 2040 (2). Breast cancer is recognized as the most common cancer and has the highest cancer-related mortality rate among women (3). An analysis of cancer registry data in Iran predicts that the incidence of breast cancer in Iranian women will rise by 63% by 2025 (4).
The chronic and debilitating nature of cancer, along with the need for home care, often necessitates the active involvement of families in the care of cancer patients, significantly impacting their health and well-being during long-term care (5). Caregivers spend the majority of their time with patients, frequently neglecting their own needs and experiencing changes in their lives, such as caregiver burden (6). Previous studies have demonstrated that the diversity and intensity of caregiving roles can lead to psychological issues in family caregivers. If left untreated, their physical and mental health deteriorates, turning them into "hidden patients" (7).
The psychological burden of caregiving, defined as the stress experienced by an individual responsible for the care and maintenance of a patient, has a destructive impact on caregivers' lives (8). This burden has two dimensions: Subjective and objective. The subjective burden refers to caregivers' personal feelings and experiences during caregiving, while the objective burden encompasses events or activities associated with negative caregiving experiences (9, 10). Studies indicate that caregivers view mental health support and psychosocial interventions as urgent needs, yet such efforts are often neglected (11). Caregivers frequently report numerous health-related problems. However, because caregiving burden is not officially recognized as a disease, both patients and caregivers suffer without adequate social support or understanding (12). A study conducted by Vahidi et al. in Tabriz revealed that nearly half of the caregivers (49.4%) had to leave their jobs due to caregiving responsibilities (13). This underscores the necessity of implementing supportive interventions for caregivers of breast cancer patients.
In the 21st century, science and technology are increasingly shaping all areas of human life. It is widely accepted that they can address many challenges and play a critical role in improving well-being (14). Telehealth has recently emerged as an innovative method for delivering healthcare services, addressing issues related to geographical barriers and improving access to care. Telehealth utilizes communication technologies to provide remote healthcare services, including consultations, diagnoses, treatments, and follow-ups (15). Internet-based health services, or e-Health, aim to enhance individuals' physical and mental health through websites. With the growing prevalence of smartphones, e-Health has expanded into mobile health applications, offering texts, images, and videos that can be accessed anytime, even with location changes (16). This shift highlights the need for smartphones to become a widely adopted educational tool, providing flexible access to educational content for caregivers (17).
Given the significant burden faced by caregivers of cancer patients, numerous face-to-face interventions have demonstrated positive outcomes. However, due to their busy schedules, caregivers often lack the time to attend such sessions. Web-based training appears to offer a viable solution to these challenges. Although limited studies have examined the effects and potential limitations of web-based interventions for cancer patient caregivers, further research is necessary to assess their efficacy.
2. Objectives
To address this gap, the present study aimed to evaluate the impact of web-based training on the caregiving burden of family caregivers of patients with cancer undergoing chemotherapy in healthcare centers affiliated with Zahedan University of Medical Sciences.
3. Methods
This quasi-experimental study was conducted with two intervention and control groups with a pre-test and post-test design on 70 family caregivers of patients with breast cancer who visited the hematology department of Khatam Al Anbia Hospital in Zahedan in 2023. The participants were selected through convenience sampling and then were randomly assigned to two intervention and control groups. To do so, 70 cards were prepared, out of which 35 were labeled as the intervention group and 35 as the control group. The cards were mixed, and each caregiver removed a card by chance and was placed in the group whose name was on the card. Accordingly, all caregivers were randomly placed into the intervention and control groups.
The inclusion criteria for the patients were having breast cancer without metastasis undergoing chemotherapy, being at least 20 years old, and living with the family. The inclusion criteria for the caregivers were being responsible for all the care and support responsibilities of the patient, age older than 20 years old, not attending any training and counseling program at the same time, having the ability to use a smartphone, the presence of only one member in the family who needs care, the absence of severe stress in the last 6 months such as the loss of relatives, having at least a middle school degree, and the absence of known neurological diseases. The exclusion criteria were the failure to perform more than one training activity provided on the site, the occurrence of a traumatic event during the study, assigning the task of caring for the patient to another family member, and the death of the patient.
The sample size was estimated based on the mean caregiver burden score in a similar study (Behzadi et al.), with a 95% confidence interval and 95% test power, and based on the following formula (18). According to similar studies, taking into account possible dropout and ensuring sampling adequacy, the sample size was considered 35 persons per group (70 persons in total).
The data for this study were collected using a demographic information form, which assessed participants' gender, age, marital status, occupation, education, place of residence, relationship with the patient, and duration of care. Additionally, the Caregiver Burden Inventory (CBI; Novak & Guest, 1989) was used to measure caregiver burden among family caregivers. This instrument consists of 24 items that evaluate caregiver burden across five dimensions: Time-dependence, developmental, physical, social, and emotional burden. Responses are based on a five-point Likert scale ranging from completely untrue (1), untrue (2), undecided (3), true (4), to completely true (5). The total score ranges from 24 to 120, with higher scores indicating a greater caregiver burden and lower scores reflecting a lesser burden. Novak and Guest reported reliability coefficients of 0.85 for time-dependent caregiver burden and Cronbach's alpha values of 0.86, 0.73, and 0.77 for physical, social, and emotional burden, respectively (19). Abbasi et al. confirmed the inventory's reliability with a Cronbach's alpha of 0.80 for use in Iran, and its validity was determined to be 90% using the content validity method (20). In this study, the reliability of the CBI was confirmed with a Cronbach's alpha of 0.83.
After obtaining the necessary approvals from the vice-chancellor for research and technology at the university, the researcher visited the hematology department of Khatam al-Anbia Hospital in Zahedan. The researcher first identified patients with breast cancer and then spoke with their main caregivers who met the inclusion criteria, explaining the study's objectives and assuring the confidentiality of their information. Caregivers who provided informed consent were selected through convenience sampling and subsequently assigned to intervention or control groups using simple randomization.
After completing the demographic information form, participants in both groups filled out the CBI as a pre-test. A mobile-based practical website called “positive” was developed by an experienced team, and participants in the intervention group were granted free access. The steps for developing the web-based program included identifying the target group and their needs, setting educational goals, determining technical requirements, developing the website, identifying potential obstacles, selecting and organizing content, structuring the sequence of information, and choosing methods for media and content delivery.
The Positive website offered several features, including the ability to create personal accounts and passwords, interaction with a symbolic character called Positive, access to Decalogue exercises related to mental health based on Lluch-Canut's 10 recommendations (21), opportunities for caregivers to provide feedback on educational content, daily educational messages about breast cancer, videos prepared by the researcher, and a discussion forum. Each Lluch-Canut recommendation included two activities, resulting in a total of 20 activities. An example of a recommendation and its related activities is shown in Table 1.
| Recommendation | Activity |
|---|---|
| Appreciate the good things you have in your life | Activity 1: |
| Step 1: Please answer the following question: "What good things do you have in life?" | |
| - My children | |
| - My colleagues | |
| - My parents | |
| - My friends | |
| - My spouse | |
| - My job | |
| - Other things | |
| Step 2: Take a moment during the day to enjoy some of the good things you have. | |
| • If the activity is not performed, the caregiver will receive a reminder later to end the activity: - “Did you find a moment to enjoy?” | |
| • If the answer is no, the message "Remember to enjoy the good things you have" appears. | |
| • If the answer is yes, the caregiver is asked "Did you enjoy this activity or not? | |
| • If the answer is yes, the message "We're glad you're enjoying the good things you have, enjoy them when you can" appears. | |
| • If the answer is no: "Don't worry, most of the time things don't go as you expect." | |
| Activity 2: | |
| Please look at your photo and answer the following questions: | |
| - I am beautiful | |
| - I am happy | |
| - I'm fine | |
| - I am responsible | |
| - I am active | |
| - I am a caregiver | |
| - I am creative | |
| - I am flexible | |
| - I am kind | |
| - I am sober | |
| - I am efficient | |
| - I am cautious | |
| The following statement appears in all the cases that gave a positive answer: "These are the characteristics that you have." | |
| The following statement appears in all the cases that gave a negative answer: "We all have positive qualities. Think about your qualities today”. | |
| Note; For finishing the activity you will receive the following advice: "Grow positivity by increasing your positive mental health". |
The Positive character, shaped like an onion, visually evolved over four weeks. Caregivers received activities from Saturday to Wednesday. Upon logging into the website, a daily welcome message, “Hello. Good morning,” appeared, followed by a question about the caregiver's emotional state: “How are you feeling today?” At the end of each activity, caregivers were asked, “Was today's activity useful for you?” If a caregiver failed to complete an activity for one day, the subsequent day's activity was locked and inaccessible.
The instructional content of the website included topics such as: What is cancer? What type of cancer is breast cancer? Breast cancer screening methods, Breast cancer diagnostic methods, Breast cancer treatments, Breast cancer treatment complications, Breast self-examination, and breast cancer in men. The intervention lasted for 20 days. Caregivers in the intervention group were instructed on how to use the website. To prevent access by the control group, each participant in the intervention group received a unique login code via SMS.
The control group did not receive any training or intervention during the study. One month after completing the intervention, participants in both groups completed the CBI as a post-test. To adhere to ethical protocols, the website address was shared with control group participants after the intervention concluded.
3.1. Data Analysis
The collected data were analyzed using SPSS-27 software, employing both descriptive and inferential statistical methods. The Shapiro-Wilk test was utilized to assess and confirm the normality of the data related to psychological burden in the pre-intervention and post-intervention phases, as appropriate for the sample size. Descriptive statistics, including mean, standard deviation, frequency, percentage, minimum, and maximum values, were calculated for all variables.
The mean scores within each group were compared using the paired samples t-test, while the mean caregiver burden scores between the two groups were analyzed with the independent samples t-test. Additionally, the chi-square test was employed to compare the frequency distributions of qualitative variables between the intervention and control groups. To evaluate the effectiveness of the intervention while controlling for the pre-test effect, analysis of covariance (ANCOVA) was performed.
A significance level of less than 0.05 (P < 0.05) was considered statistically significant throughout the analyses.
4. Results
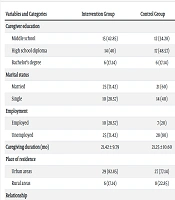
No participants from either the control or intervention groups withdrew from the study; therefore, data from all 70 participants were included in the analysis. The findings revealed that 88.6% of the caregivers in the intervention group and 94.3% in the control group were female. Fisher’s exact test showed no significant difference between the two groups regarding gender (P = 0.67). The mean age of the patients in the intervention and control groups was 47.91 ± 10.65 and 50.45 ± 8.32 years, respectively, with no significant difference between the groups (P = 0.27). Similarly, the mean age of the caregivers in the intervention and control groups was 33.77 ± 5.58 and 31.80 ± 5.17 years, with no statistically significant difference (P = 0.13). The duration of the patients’ illness (cancer) in the intervention and control groups was 21.42 ± 9.79 and 21.25 ± 10.60 months, respectively, and this was also not significantly different, as confirmed by the independent samples t-test (P = 0.171). Other demographic characteristics of the caregivers in the two groups are summarized in Table 2.
| Variables and Categories | Intervention Group | Control Group | P-Value |
|---|---|---|---|
| Caregiver education | 0.73 b | ||
| Middle school | 15 (42.85) | 12 (34.28) | |
| High school diploma | 14 (40) | 17 (48.57) | |
| Bachelor’s degree | 6 (17.14) | 6 (17.14) | |
| Marital status | 0.31 b | ||
| Married | 25 (71.42) | 21 (60) | |
| Single | 10 (28.57) | 14 (40) | |
| Employment | 0.40 b | ||
| Employed | 10 (28.57) | 7 (20) | |
| Unemployed | 25 (71.42) | 28 (80) | |
| Caregiving duration (mo) | 21.42 ± 9.79 | 21.25 ± 10.60 | 0.94 c |
| Place of residence | 0.55 b | ||
| Urban areas | 29 (82.85) | 27 (77.14) | |
| Rural areas | 6 (17.14) | 8 (22.85) | |
| Relationship | 0.71 d | ||
| Spouse | 4 (11.42) | 2 (5.71) | |
| Daughter | 15 (42.85) | 19 (54.28) | |
| Sister | 13 (37.14) | 12 (34.28) | |
| Other | 3 (5.57) | 2 (5.71) |
a Values are expressed as No. (%) or mean ± SD.
b Chi-square test.
c Independent samples t-test.
d Fisher’s exact test.
As presented in Table 3, the mean psychological burden score of caregivers in the intervention and control groups before the intervention was 86.34 ± 12.66 and 87.45 ± 9.86, respectively, showing no statistically significant difference (P = 0.683). However, post-intervention analysis revealed a significant difference (P = 0.002) between the two groups in terms of psychological burden scores (85.82 ± 9.69 in the control group vs. 77.42 ± 11.87 in the intervention group). Additionally, within the intervention group, the mean psychological burden score of caregivers significantly decreased from 86.34 ± 12.66 before the intervention to 77.42 ± 11.87 after the intervention (P = 0.001).
a Values are expressed as No. (%)
b Paired samples t-test.
c Independent samples t-test.
Given that the necessary assumptions were met, the results of the analysis of covariance (ANCOVA), controlling for the pre-test effect (Table 4), demonstrated that after the web-based training intervention, the average psychological burden score of caregivers in the intervention group was significantly lower than that of caregivers in the control group (P = 0.001).
| Source of Changes | Sum of Squares | df | Mean Squares | F | Sig. | Effect Size | Test Power |
|---|---|---|---|---|---|---|---|
| Pre-test | 7157.72 | 1 | 7157.72 | 580.71 | 0.001 | 0.897 | 1 |
| Group | 954.09 | 1 | 954.09 | 77.40 | 0.001 | 0.536 | 1 |
| Error | 825.81 | 67 | 12.32 | - | - | - | - |
| Total | 475644 | 70 | - | - | - | - | - |
5. Discussion
The present study investigated the impact of web-based training on the caregiver burden of family caregivers of patients with breast cancer undergoing chemotherapy. The findings revealed a significant difference between the caregivers who received the training intervention and those in the control group regarding the severity of caregiver burden in the post-intervention phase, confirming the positive effect of web-based distance education in reducing caregiver burden. The beneficial role of distance education in alleviating caregiver burden has been supported by findings from other studies. For instance, Behzadi et al. demonstrated that online network-based training enhanced resilience and reduced caregiver burden among parents of children with cancer (18). Similarly, Ferre-Grau et al. reported that mobile-based training programs for non-professional caregivers effectively reduced caregiver burden (22). These studies emphasize the critical role of web-based training in empowering caregivers and mitigating the burden associated with caregiving responsibilities.
A systematic review by Marzorati et al. further corroborated the benefits of online network-based training, showing improvements in the psychological and physical burden of caregivers of patients with cancer (23). This review highlighted the potential of online education to enhance the caregiving experience by reducing stress and strain among caregivers.
In addition, Tinoco-Camarena et al. evaluated the effectiveness of online dialogue circles and found that these interventions significantly reduced the caregiver burden for those supporting patients with complex chronic diseases, particularly when face-to-face interaction was not feasible (24). Nobakht et al. also reported that web-based daily care training positively impacted the quality of life of mothers of children with cerebral palsy (25). These findings underscore the importance of structured and practical distance education, especially in contexts where in-person training is inaccessible.
However, despite the general effectiveness of web-based training in most clinical and non-clinical settings, some studies have reported contrasting results. For example, Bakitas et al., in a study conducted in Alabama, USA, found that online palliative care training did not significantly reduce the caregiver burden of family caregivers of heart failure patients (26). These discrepancies may be attributed to variations in the type of disease, the nature of the training interventions, and the specific content provided to participants.
Moreover, the present study revealed that the mean psychological burden scores of mothers of children with cancer in the control group significantly decreased in the post-intervention phase compared to the pre-intervention phase. This reduction could be attributed to the caregivers’ exposure to instructional content available in the hematology department. Additionally, web-based training proved to be a highly practical method for caregivers of cancer patients due to its flexibility in terms of time and location. Despite their heavy caregiving responsibilities and time constraints, caregivers can benefit from this method, enabling them to acquire essential knowledge and skills without attending in-person training sessions.
Web-based training also addresses critical challenges faced by caregivers, such as fatigue, anger, and undervaluation. By providing psychological burden management skills, this training method effectively reduces caregiver burden. A notable advantage of web-based training is the opportunity for caregivers to exchange experiences and participate in online forums. Through these social connections, caregivers can share their experiences, receive guidance from others, and alleviate feelings of loneliness and isolation, ultimately improving their mental health. Furthermore, web-based programs encourage participants to engage in activities designed to enhance mental health and boost self-confidence. These activities, combined with evidence-based instruction and digital tools, contribute to reducing both the psychological and physical burden of caregiving.
One of the key strengths of this study was the online delivery of instructional content, enabling participants to access the material without incurring additional time or financial costs. This feature indirectly reduced the economic burden on caregivers while increasing accessibility and convenience. Another innovative aspect of the study was the use of a "positive" personality simulation in the form of an onion, visually representing the caregiver’s progress over the 20-day training program.
However, the study had some limitations. These included inconsistencies in the kinship relationships between caregivers and patients, differences in caregivers' gender, varying durations of care, and the absence of long-term retention assessments of the intervention's effects. Additionally, as the patients were undergoing chemotherapy, external factors such as social support may have influenced the psychological burden of the caregivers. The use of a quasi-experimental design allowed the study to examine the intervention's impact under real-world caregiving conditions. However, since the participants were caregivers of patients with non-metastatic breast cancer, the findings may not be generalizable to caregivers of patients with metastatic cancer. Future studies should aim to investigate caregiver burden over extended timeframes with larger sample sizes and include caregivers of patients with other types and stages of cancer.
5.1. Conclusions
The findings of the present study demonstrated the positive impact of web-based training in reducing the caregiving burden of caregivers of patients with breast cancer. Considering that many caregivers face challenges such as excessive fatigue, anxiety, and diminished quality of life, web-based training emerges as a practical, innovative, and effective method to enhance their well-being. Therefore, implementing web-based training programs can be recommended as an accessible and convenient tool for supporting caregivers of cancer patients and alleviating their caregiving burden. This approach can be integrated into medical centers, allowing caregivers to benefit from training at any time and location. Furthermore, future research should explore the effectiveness of web-based training across various diseases and interventions to identify the most impactful strategies for reducing caregiver burden.