1. Background
Chronic renal failure is one of the biggest health problems in the world (1). According to available evidence, chronic renal failure affects more than 10% of the general population worldwide, accounting for more than 800 million people (2). In Iran, about 320 thousand people suffer from severe chronic renal failure. Approximately 49% of these patients have had a kidney transplant, and the rest use hemodialysis (48%) and peritoneal dialysis (3%) (3). Hemodialysis is the most common form of renal replacement therapy for patients with chronic renal failure (4, 5), which causes changes in the lifestyle and health status of the individual. Hemodialysis not only compromises physical health but also other aspects of health and affects the quality of life of patients (6, 7). In Iran, the annual growth rate of patients undergoing hemodialysis is 15% (8). These patients suffer from long-term complications such as anorexia, nausea, vomiting, oliguria, early fatigue, shortness of breath, limb edema, anemia, electrolyte imbalance, and pulmonary edema (9).
While undergoing dialysis, patients receive a complex treatment regimen and experience extensive and fundamental changes in their lifestyle, which leads to limitations in the physical, mental, and social functioning of the patients (10). Adherence to restrictions can create conflict and tension in living with hemodialysis and may be overwhelming for the patient, which in turn will lead to different reactions. Hemodialysis patients also face changes in self-concept and self-confidence, disruption in family roles, and loss of self-worth and position (11). Hemodialysis disrupts the individual's life and changes the course of the patient's and his/her family's lives, and by affecting the course of the individual's family life, it will also have negative effects on the community (12). Physical and psychological problems caused by hemodialysis reduce the quality of life, cause frequent hospitalizations, and increase the cost of treatment and healthcare for patients (13). Thus, to improve the quality of life of hemodialysis patients, it is very important to ensure their adherence to treatment and guide them to engage in more healthy lifestyle behaviors (14).
A health-promoting lifestyle, which is defined as controlling some behaviors and choosing health-promoting behaviors in daily life for one's health (15), is a way of life that ensures, maintains, and promotes the health and well-being of an individual, reduces the risk of disease exacerbation and premature death, and with its help, the individual can enjoy more aspects of life (16). A health-promoting lifestyle is a combination of six dimensions that include belief in the power of God to maintain the mental dimension of health, a sense of responsibility for health, maintaining interpersonal relationships to promote the social dimension of health, stress management to prevent physical and mental diseases, exercise and physical activity, and adherence to a healthy diet to maintain health (17). Studies conducted on the lifestyle of hemodialysis patients have shown that health-promoting behaviors in hemodialysis patients are affected by kidney disease and hemodialysis treatment and have no favorable outcomes (18, 19).
To better plan for changing unhealthy behaviors and promoting health, various theories and models have been proposed. One of the most important models is Pender's health promotion model. This model developed by Pender in 1982 is one of the descriptive models in nursing and can predict health behaviors (20). The main goal of this model is to promote health and empower individuals to achieve optimal health (21, 22). According to this model, health behaviors are influenced by social, psychological, and environmental factors. Accordingly, perceived barriers and benefits, interpersonal factors, and self-efficacy are considered to be the most important effective constructs in changing behavior and promoting health (23). This model provides nurses with more opportunities to help individuals, families, and communities improve their health, functional capacity, and quality of life (24). Lifestyle changes should be considered alongside other treatments as a key factor in reducing complications and improving symptoms (25).
Numerous studies have shown that training interventions based on the health promotion model have a positive effect on the quality of life, self-efficacy, and health-promoting behaviors in people in different age groups and with chronic diseases such as diabetes, hypertension, and heart disease. The evidence suggests that this method is effective in changing patients' behavior (26-29). Although a limited number of studies have examined the effectiveness of interventions based on this model on self-efficacy, adherence to treatment, and mental health in hemodialysis patients, their results confirmed the effectiveness of this model (30, 31). However, the researchers in the present study could not find a study that specifically addressed the effect of a training intervention based on Pender’s health promotion model on the lifestyle of hemodialysis patients. Moreover, the studies that have examined the effect of health promotion behavior education on patients’ lifestyles did not use a specific theoretical framework for education (32).
2. Objectives
Therefore, to fill this gap in the literature and improve patients’ lifestyles to promote their health, the present study sought to investigate the effect of a training intervention developed based on Pender’s health promotion model on the lifestyle of patients undergoing hemodialysis.
3. Methods
This quasi-experimental study adopted a pre-test and post-test design with a control group. The research population consisted of hemodialysis patients admitted to the dialysis wards of hospitals affiliated with Zahedan University of Medical Sciences in 2022. The sample size was estimated to be 18.36 patients, based on a similar study by Masoudi et al., with a confidence level of 95% and a statistical test power of 95% using the sample size formula. However, to account for potential participant dropout and to ensure sampling adequacy, the sample size was increased to 30 persons per group, totaling 60 participants (30).
After obtaining the necessary permits from the Vice-Chancellor for Research, the researcher visited the hemodialysis departments of the hospitals and provided information about the study objectives and procedures to the hospital officials. Participants were selected from patients who met the inclusion criteria, were willing to participate (both patients and their primary caregivers), and signed an informed consent form. The selected patients were randomly assigned to intervention and control groups through drawing lots.
The inclusion criteria for patients were: Age 20 to 60 years, undergoing hemodialysis for at least 6 months, literacy, Iranian nationality, fluency in Persian, and no mental illnesses or other severe chronic illnesses. The inclusion criteria for primary caregivers were being at least 18 years old and willing to participate. Exclusion criteria included the occurrence of new illnesses during the study, absence from training sessions, kidney transplantation, and withdrawal by the patient or caregiver.
Data were collected using a demographic information form recording variables such as age, gender, marital status, education, and duration of dialysis, and Walker’s (1987) health-promoting lifestyle profile (HPLP-II). This instrument contains 52 items across 6 subscales: Spiritual growth and self-actualization (items 1 - 8), health responsibility (items 9 - 22), interpersonal relationships/social support (items 23 - 30), stress management (items 31 - 37), physical activity (items 38 - 44), and nutrition (items 45 - 52). Items are scored on a four-point Likert scale (never = 1, sometimes = 2, often = 3, always = 4), with total scores ranging from 52 to 208. Higher scores indicate higher levels of health-promoting behaviors. The instrument's reliability was confirmed with a Cronbach’s alpha of 0.94, with subscale values ranging from 0.79 to 0.94 (33). In Iran, Mohammadi Zeidi et al. confirmed its validity using exploratory factor analysis and estimated reliability with a Cronbach’s alpha of 0.82, with subscale values ranging from 0.64 to 0.91 (34). In this study, reliability was confirmed with a Cronbach’s alpha of 0.87.
Before the study, the researcher provided instructions about the study objectives and procedures to participants and obtained written consent from patients and caregivers. After assigning patients to intervention and control groups, the demographic form and HPLP-II items were completed through interviews with all patients. Patients in the intervention group attended a training intervention based on Pender’s health promotion model, consisting of six 45-minute individual sessions held at the patient's bedside during dialysis. Each session focused on one dimension of Pender's model (nutrition, physical activity, stress management, health responsibility, interpersonal relationships/social support, and spiritual growth), based on perceived benefits, barriers, and self-efficacy (Table 1). Participants were asked to follow behavior change programs and apply them in daily activities. The researcher followed up on care performance by telephone and answered questions for 3 months. An educational booklet was provided to patients and caregivers after the intervention. Control group patients received routine care only, but were also provided with an educational booklet to comply with ethical protocols. The HPLP-II items were completed again one and three months after the intervention for all patients in both groups.
| Sessions | Focus | Perceived Benefits | Perceived Barriers | Perceived Self-Efficacy |
|---|---|---|---|---|
| 1 | Nutrition | Explaining the benefits of following a balanced diet in controlling the patient's condition and improving quality of life, discussing essential nutrients and their impact on general health | Discussing barriers to healthy eating, unhealthy eating habits, and the patient's challenges in changing them | Teaching patterns and behaviors related to proper nutrition, providing solutions to overcome barriers to healthy eating, and quitting unhealthy eating habits |
| 2 | Physical activity | Explaining the benefits of exercise for improving physical and mental health, the role of exercise in reducing anxiety and stress | Discussing barriers to physical activity, physical conditions, and mobility limitations of each patient | Teaching appropriate physical and sports patterns and activities for patients undergoing hemodialysis, time management techniques for incorporating sports activities in the daily schedule, and providing appropriate exercises according to the patient's physical condition and limitations |
| 3 | Interpersonal relationships/social support | Discussing the benefits of having effective interpersonal relationships and receiving social support for mental health and desirable quality of life, the positive effects of communication on increasing a sense of belonging, and reducing loneliness | Discussing the barriers to establishing effective communication with others, such as fear of judgment, lack of self-confidence, etc., the problems faced by the patient in establishing effective communication with loved ones | Teaching the concept of communication, effective techniques for establishing communication such as active listening, expressing emotions, etc., problem-solving and conflict-solving styles in social interactions and personal life, encouraging the establishment of new relationships and strengthening existing ones |
| 4 | Self-actualization/spiritual growth | Discussing the benefits of setting personal goals and striving to achieve them in increasing life satisfaction, and the impact of spiritual growth on increasing hope and motivation | Discussing barriers to self-actualization such as lack of time, lack of social support, fear of failure, etc., and the patient's negative beliefs that prevent self-knowledge and spiritual growth. | Teaching the concept of self-actualization, techniques for increasing psychological growth and self-actualization in dialysis patients, encouraging having a purpose in life, methods for managing and pursuing personal goals, encouraging positive thinking and empowerment in facing challenges and obstacles, encouraging the patient to perform prayers and acts of worship to strengthen spiritual beliefs |
| 5 | Health responsibility | Discussing the importance of medical check-ups and follow-up treatment, the positive effects of self-care on quality of life | Discussing barriers to access to healthcare services, barriers to self-care, barriers to patient adherence to treatment, patient beliefs and misconceptions about various aspects of self-care such as skin care, fistula, etc., providing care and following up on treatment | Teaching the concept of health responsibility, correcting the patient's incorrect beliefs and misconceptions about self-care, teaching self-care techniques, and strategies to increase health responsibility, and providing solutions to remove barriers to adherence to treatment based on each patient's needs |
| 6 | Stress management | Discussing the benefits of stress management in improving quality of life and daily functioning, the effect of relaxation techniques on reducing stress and improving mental health | Discussing obstacles to implementing stress management techniques, and life stressors that lead to stress. | Teaching the concept of stress, and relaxation techniques, and encouraging patients to find and use personal methods to reduce stress and improve mental health |
The collected data were analyzed using SPSS version 22 software. Descriptive statistics, including measures of central tendency and dispersion such as mean, median, mode, variance, and standard deviation, were employed. Inferential statistics were also utilized. The Shapiro-Wilk test was conducted to assess the normal distribution of the data. Additionally, the independent samples t-test and chi-square test were used to compare demographic variables between the two groups. To examine changes in means over time and between the intervention and control groups, repeated measures analysis of covariance (ANCOVA) was employed, along with the Bonferroni test to correct for type I error in multiple comparisons. The significance level for all statistical procedures was set at 0.05 (P < 0.05).
4. Results
No participants in either the intervention or control groups withdrew from the study. The Shapiro-Wilk test indicated that the demographic data in both groups were normally distributed. Analysis using independent samples t-tests and chi-square tests revealed no statistically significant differences between the intervention and control groups regarding demographic variables such as age, gender, marital status, education, and duration of dialysis (P > 0.05) (Table 2). Therefore, the two groups were homogeneous concerning these demographic variables.
| Variables and Categories | Intervention Groups | Control Groups | Statistics |
|---|---|---|---|
| Gender | χ2 = 0.06; df = 1; P = 0.79 b | ||
| Male | 15 (50) | 14 (46.7) | |
| Female | 15 (50) | 16 (53.3) | |
| Total | 30 (100) | 30 (100) | |
| Ethnicity | χ2 = 4.8; df = 1; P = 0.06 b | ||
| Fars | 6 (20) | 14 (46.7) | |
| Baloch | 24 (80) | 16 (53.3) | |
| Total | 30 (100) | 30 (100) | |
| Marital status | χ2 = 1.002; df = 1; P = 0.31 b | ||
| Single | 7 (23.3) | 4 (13.3) | |
| Married | 23 (76.7) | 26 (86.7) | |
| Total | 30 (100) | 30 (100) | |
| Main caregiver | χ2 = 0.37; df = 2; P = 0.82 b | ||
| Spouse | 13 (43.3) | 14 (46.7) | |
| Parents | 9 (30) | 10 (33.3) | |
| Child | 15 (26.7) | 6 (20) | |
| Total | 15 (100) | 30 (100) | |
| Age | 490.3 ± 15.72 | 48.20 ± 14.23 | t = 0.21; df = 58; P = 0.83 c |
| Academic years | 10.56 ± 7.897 | 11.8 ± 6.924 | t = 0.992; df = 58; P = 0.325 c |
a Values are expressed as No. (%) or mean ± SD.
b Chi-square test.
c Independent samples t-test.
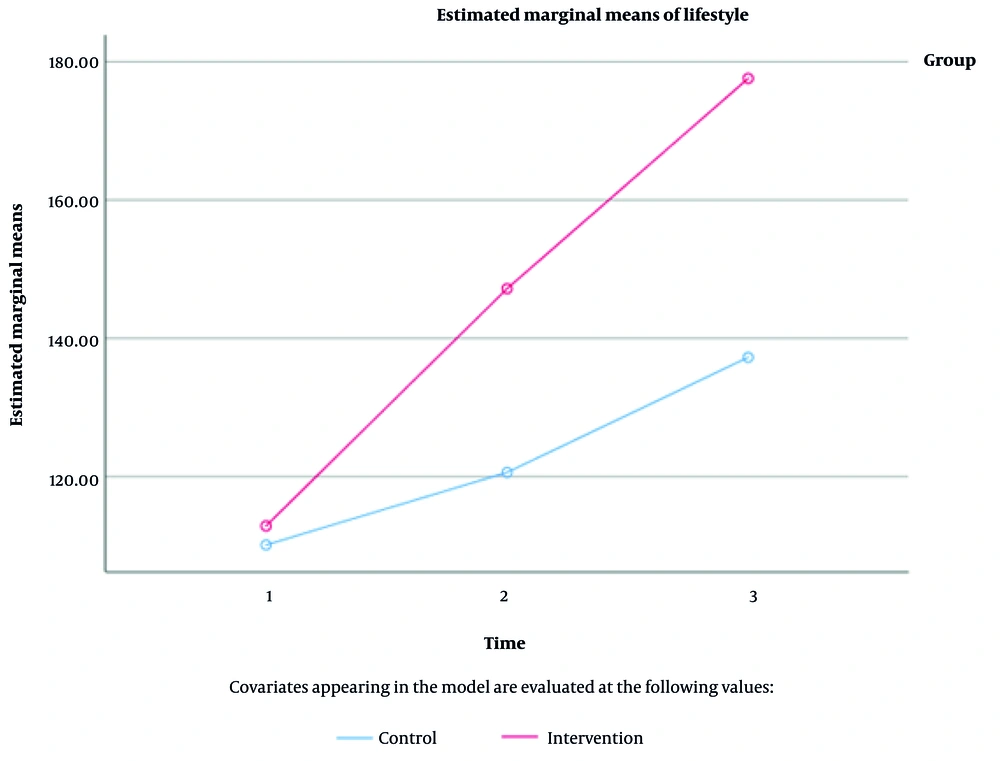
The mean lifestyle score of hemodialysis patients was not significantly different between the two groups before the intervention (P = 0.47). However, the mean total lifestyle score of patients in the intervention group increased compared to the control group one month and three months after the intervention. Repeated measures ANOVA did not show a significant interaction effect of time and group (P = 0.06). Table 3 presents a comparison of the mean scores for the six lifestyle dimensions before, and one and three months after the intervention. The time-group interaction effect in the repeated measures ANOVA between the intervention and control groups, one month and three months post-intervention, was not significant for the dimensions of health responsibility, stress management, and interpersonal relationships/social support (P > 0.05). However, the difference in means for health responsibility was statistically significant over time (P = 0.04).
| Variables and Times | Intervention Groups | Control Groups | P-Value b | ANOVA | ||
|---|---|---|---|---|---|---|
| PGroup | PTime | PTime/Group | ||||
| Nutrition | 0.001 | 0.02 | ≤ 0.001 | |||
| Pre-intervention | 24.86 ± 5.63 | 26.10 ± 7.46 | 0.47 | |||
| One month after the intervention | 32.96 ± 3.10 | 27.26 ± 7.36 | < 0.001 | |||
| Follow-up c | 39.23 ± 2.12 | 29.26 ± 7.70 | < 0.001 | |||
| Physical activity | 0.001 | 0.04 | < 0.001 | |||
| Pre-intervention | 27.70 ± 5.01 | 26.46 ± 4.91 | 0.34 | |||
| One month after the intervention | 34.10 ± 5.44 | 29.06 ± 4.59 | < 0.001 | |||
| Follow-up | 42.16 ± 3.49 | 32.56 ± 4.17 | < 0.001 | |||
| Health responsibility | 0.04 | 0.04 | 0.61 | |||
| Pre-intervention | 18.03 ± 4.49 | 17.73 ± 3.42 | 0.77 | |||
| One month after the intervention | 23.73 ± 1.96 | 20.63 ± 4.73 | 0.002 | |||
| Follow-up | 34.26 ± 62.97 | 27.63 ± 1.62 | 0.01 | |||
| Stress management | 0.93 | 0.76 | 0.94 | |||
| Pre-intervention | 10.70 ± 1.74 | 8.70 ± 1.84 | 0.06 | |||
| One month after the intervention | 15.70 ± 1.70 | 9.56 ± 2.89 | < 0.001 | |||
| Follow-up | 19.93 ± 1.50 | 1073 ± 3.15 | < 0.001 | |||
| Interpersonal relationships/social support | 1 | < 0.001 | 0.22 | |||
| Pre-intervention | 14.03 ± 4.12 | 13.56 ± 3.02 | 0.61 | |||
| One month after the intervention | 21.36 ± 2.29 | 20.16 ± 2.87 | 0.07 | |||
| Follow-up | 26.93 ± 1.81 | 24.46 ± 2.77 | < 0.001 | |||
| Self-actualization | 0.08 | 0.009 | 0.03 | |||
| Pre-intervention | 14.90 ± 2.84 | 15.06 ± 2.44 | 0.8 | |||
| One month after the intervention | 19.23 ± 1.97 | 19.83 ± 2.40 | 0.29 | |||
| Follow-up | 23.60 ± 2.35 | 21.63 ± 1.69 | < 0.001 | |||
| Total lifestyle score | < 0.001 | 0.002 | 0.06 | |||
| Pre-intervention | 113.20 ± 19.46 | 19.80 ± 10.90 | 0.47 | |||
| One month after the intervention | 147.66 ± 11.32 | 120.13 ± 19.16 | < 0.001 | |||
| Follow-up | 178.80 ± 6.50 | 136.03 ± 21.49 | < 0.001 | |||
Abbreviation: ANOVA, analysis of variance.
a Values are expressed as mean ± SD.
b Independent samples t-test.
c Three months after the intervention.
Given the significant interaction effect of time and group in the repeated measures ANOVA for the dimensions of nutrition, physical activity, and self-actualization, point-by-point comparisons were conducted again with Bonferroni correction for time and group. The results indicated that the mean score for nutrition significantly improved one and three months after the intervention compared to the pre-intervention phase (P < 0.001). Figure 1 illustrates a comparison of the mean lifestyle scores for hemodialysis patients in the intervention and control groups during the pre-intervention phase and one month and three months post-intervention.
5. Discussion
The findings of the present study suggest that, although the training intervention based on Pender’s health promotion model did not have a statistically significant effect on the lifestyle of hemodialysis patients, it was clinically meaningful. Several studies have demonstrated that education based on health-oriented theories can promote health-related behaviors in patients. For instance, Jafari Naal Ashkanani et al. examined the effect of an educational program based on the planned behavior pattern on improving the lifestyle of hemodialysis patients. Their findings indicated that, following the educational intervention, the lifestyle scores of participants in the intervention group improved significantly compared to the control group. The scores of all constructs of the theory of planned behavior for participants in the intervention group increased significantly post-intervention compared to the control group (35).
Additionally, Khodaveisi et al. and Salahinezhad et al. reported a significant improvement in the mean score of health-promoting behaviors in the intervention group after conducting a training program based on Pender’s health promotion model (17, 36). It appears that training interventions developed based on Pender’s health promotion theory provide a coherent and purposeful framework for teaching and focusing on specific health-promoting behaviors, identifying and strengthening the factors affecting these behaviors, thereby improving patients' lifestyles.
The present study also demonstrated that the intervention significantly improved the nutritional behaviors of hemodialysis patients. Similarly, Khodaveisi et al. reported changes in the nutritional habits of patients undergoing coronary angioplasty after implementing a training intervention based on Pender’s health promotion model (36). However, some studies, such as Oshvandi, found no significant difference in the nutritional behaviors of participants in the intervention and control groups after executing the training intervention (37). These conflicting findings may be attributed to differences in training interventions, treatment conditions, or individual differences in sensitivity to and perception of nutritional changes.
The present study also showed no statistically significant difference in physical activity between hemodialysis patients in the intervention and control groups, as confirmed in previous studies (e.g., Oshvandi, Mohammadipour et al.) (28, 37). Moreover, Xiao et al. reported that physical activity and exercise obtained the lowest scores (38). However, Ebrahimi et al. and Babaei et al. showed that the training intervention improved the level of exercise and physical activity in participants (39, 40). These contradictory findings could be attributed to differences in the research population, varying levels of perceived threat and perceived sensitivity by individuals, and the time required for patients to adapt to and accept physical activities.
Health responsibility was another aspect of health-promoting behaviors examined in the present study, where no statistically significant difference was observed between the intervention and control groups. The findings of this study are consistent with some other studies, including those by Dashti Dehkordi et al. and Radmehr et al. (19, 41). Behnam Moradi et al. examined the effect of health promotion education based on Pender’s model on health responsibility and stress management in postmenopausal women and reported a significant improvement in health responsibility among participants (42). Furthermore, Ebrahimi et al. showed that education improved women's sense of responsibility for their health (39). Oshvandi also reported a statistically significant difference in health responsibility between the intervention and control groups post-intervention (37). These studies reported contradictory findings, likely due to differences in the demographic and psychological characteristics of participants, which affected their outcomes.
The present study found no statistically significant change in stress management among patients in the intervention group after conducting the training intervention. In contrast, Behnam Moradi et al. studied the effectiveness of health promotion education based on Pender’s model in health responsibility and stress management in postmenopausal women and reported that the training intervention improved stress management ability in the intervention group compared to the control group, with a significant difference between the two groups (42). Ebrahimi et al. also showed that education improved stress management (39). Moreover, Babaei et al. demonstrated that the training intervention was effective in improving some aspects of lifestyle, including stress management (40).
Factors influencing health behaviors are multidimensional and interrelated, directly and indirectly affecting health-promoting behaviors. These factors, working together, support the processes that influence individuals to make decisions and engage in health-promoting behaviors. These factors can account for contradictory findings reported in previous studies. Additionally, hemodialysis patients may require a longer time to adapt to the disease and, consequently, manage their stress due to their specific disease conditions.
Furthermore, the present study indicated that interpersonal relationships/social support did not significantly improve in patients in the intervention group after conducting the training intervention. Similarly, Rakhshani et al. found no association between a health-promoting lifestyle and quality of life among Iranian older adults (43). In contrast, Oshvandi reported a significant improvement in interpersonal relationships in both the intervention and control groups post-intervention (37). Zheng et al. also demonstrated that a nurse-led lifestyle intervention program effectively improved interpersonal relationships and health-promoting behavior in patients with metabolic syndrome (44). Furthermore, Babaei et al. revealed that the training intervention was effective in improving interpersonal relationships (40). Likewise, Borzou et al. and Khani et al. (2020) reported a significant increase in interpersonal relationships in the intervention group compared to the control group (20, 32). The ineffectiveness of the training intervention based on Pender’s health promotion model in the present study on interpersonal relationships may be attributed to the nature of the disease, as making changes in interpersonal relationships is more challenging than other behaviors and requires more time.
The data in the present study demonstrated that the training intervention had no significant impact on spiritual growth and individual self-actualization in patients in the intervention group. Similarly, Babaei et al. showed that the training intervention was not effective in improving participants’ self-actualization scores (40). Moreover, Dashti Dehkordi et al. indicated that the mean scores of health-promoting behaviors in the self-actualization domain did not differ significantly between the two groups post-intervention (19). However, Borzou et al. and Khani et al. reported a significant increase in the level of self-actualization after conducting the intervention program in the treatment group compared to the control group (20, 32). These conflicting differences can be attributed to patients’ understanding and experience of the nature of their diseases and symptoms, leading to differences in the level of importance given to one or more of the six aspects of patients’ lifestyles.
One of the strengths of the present study was the employment of Pender’s health promotion model as the theoretical framework, which created a comprehensive and evidence-based construct for developing the training intervention. Additionally, assessing various lifestyle components, including nutrition, physical activity, and health responsibility, led to a more comprehensive understanding of the training intervention's impact on patients' lives. Furthermore, the long-term evaluation of the intervention's effect at one-month and three-month intervals provided the opportunity to observe more sustainable effects of the training program.
One of the main limitations of the present study was the use of a self-report tool for data collection, which may have led to bias in findings. Furthermore, patients’ differences and mental states could have affected their adherence to the training program and, consequently, lifestyle changes, which were factors beyond the researcher's control and may have affected the study's findings.
5.1. Conclusions
The present study showed that the training intervention based on Pender’s health promotion model clinically improved the lifestyle of patients undergoing hemodialysis. The significant improvement observed in most lifestyle dimensions over time indicates that the effects of educational interventions extend beyond short-term impacts and remain sustainable over longer periods. This highlights the importance of continuing educational programs and enhancing patient support over time. Given the limitations of this study, such as the effect of patients’ individual differences and mental states on the findings, future studies need to examine the long-term effects of the training program with more diverse groups and larger sample sizes to provide more reliable findings about the effectiveness of health-oriented educational models.