1. Background
Pregnancy and at a wider scope, pregnancy and delivery process, have a significant impact on public health status. One of the important aspects of mothers’ lives is having a safe pregnancy and delivery (1). In the recent decades, there have been a significant reduction in the frequency of cesarean sections in developed countries; however, the same trend is increasing in developing countries, which is due to the fear of labor pain as well as complications, such as perineal injury and pain during delivery, especially during their first birth. Episiotomy is the most common surgical procedure practiced after cutting the umbilical cord in midwifery (2). In simple terms, episiotomy refers to a perineal incision, which is a surgical incision made in the perineum to assist the active process of labor and prevent severe perineal tears (3). Perineal tears are divided to four groups, including first to fourth grade perineal tears. First-grade tears usually involve the hymen and perineum of the vagina. Second-grade perineal tears, in addition to the above regions, involve fascia and perineal muscles. Third-grade tear affects a greater extent and involves the anal sphincter, however, fourth-grade tears spread throughout the rectum mucosa and reveal rectum (4, 5). Available evidence shows that routine episiotomy is not an effective form of care and may even be harmful (5). Studies show that the risk of various perineal tears, even that of the third and fourth-grade are increased by more than three times in the second birth of females, who had undergone episiotomy in their first birth (6). According to available data, the episiotomy rate was 40%, yet the same rate was at its highest in Latin America, while it was lower in the European countries (3). Episiotomy is frequently used in Iran; in educational hospitals of Tehran (2008), the episiotomy rate was reported to be about 97% (7). However, various articles have reported episiotomy rates of between 30% and 90% (8). According to the World Health Organization (WHO), the episiotomy rate of 20% is sufficient during childbirth (9, 10). Some possible episiotomy complications include bleeding, infection, third and fourth grade perineal tears, cellulitis, episiotomy opening, abscess formation, flatus and fecal incontinence, rectovaginal fistula, weakened rectal sphincter consistency, necrotizing fasciitis, and even death (11). In addition to the complications, episiotomy is also associated with complications, such as intercourse pain, necessity of suturing, sexual dysfunction, delayed breastfeeding, and delayed postpartum healing (2). Reducing the frequency of episiotomy is practiced in many parts of the world (12, 13). Also, to reduce the episiotomy rate and the subsequent damage to the perineum and genital tract, midwives use different techniques in the second stage of labor, yet overall, there is no similar and effective method for protecting the perineum (9, 14). The management techniques that have so far been implemented to protect the perineum, especially in the second stage of labor, include perineal massage, local heating of the perineum, lack of using hands while the baby’s head is coming out, and Ritgen’s maneuver, all of which are still being investigated in various studies (11). The use of local heating of the perineum is one of the supportive methods that is usually used during the second stage of labor by midwives. The mechanism of this method is to increase the relaxation and expansion of the perineal muscles, as well as to increase the blood supply to the perineum (15, 16). However, there are limited studies in this field to support the perineum to stay intact (13, 15, 17). Considering that the practice of episiotomy is currently one of the important issues in the field of vaginal delivery, which can affect the mother's attitude towards both the choice of vaginal delivery and choice of type of delivery as well as reducing complications of episiotomy and other perineal tear grades, the aim of the present study was to determine the effect of heating pad on the frequency of episiotomy and perineal tears in primiparous females.
2. Methods
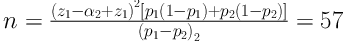
This clinical trial was carried out on primiparous mothers, who referred to Imam Ali Hospital of Andimeshk city, Iran, during year 2014. The sample size was calculated as 57 individuals in each group with a 95% confidence interval (CI) and study power of 90%, using the below formula. A total of 114 individuals were selected and randomly assigned to intervention and control groups.
Inclusion criteria included mother’s age being between 18 and 35 years, baby’s normal birth weight (ranging from 2500 to 4000 grams), term pregnancy, absence of any contraindication for normal delivery at the time of admission, singleton pregnancy with fetus, and cephalic presentation. Exclusion criteria also included the creation of any medical and obstetric contraindications in case of continuation of normal delivery during the implementation of the project, the need for cesarean section, any labor dystocia, such as shoulder dystocia, and carrying out the delivery by maternity aids, such as ventouse. First, the researcher referred to Imam Ali Hospital in Andimeshk after receiving a letter of introduction from the Vice-Chancellor for research of Ahvaz University of Medical Sciences. After obtaining the written consent of the hospital authorities, the researcher selected the subjects from the target population. Continuous sampling was conducted by inviting females, who were eligible to participate in the study after giving oral and written explanations and obtaining written consent from the mothers. A form of demographic characteristics and clinical factors was used to collect data, including maternal age, gestational age (week), maternal birth weight, place of residence and maternal education, as well as labor outcomes, fetal weight, size, and head circumference, first-minute Apgar score of the baby, and duration of the second stage of labor. Practice of episiotomy and perineal tears, evaluated and recorded in the form of intact perineum, fits, second, third and fourth grades tears, were completed for each of the mothers participating in the study. The study procedure was such that secretions scattered around the perineum were first removed using a sterile gauze, and then the heating pad was placed on the external region of the perineum, and the viscous layer on the perineum-facing surface of the pad facilitated the adhesion of the pad to the perineum even in case of presence of extra hair and could not easily be removed from the perineum. This rectangular pad had a length of 5 cm and width of 7 cm and was produced in Iran and made available in reputable pharmacies of the country. This pad had the ability to produce heat to about 50°C continuously and up to a maximum of 12 hours. It was placed on the perineum with the start of the second stage of labor by trained midwives in each shift and removed from the perineum during the mother’s transfer to the labor room. The heat generated by this pad justifies its effects, including increased blood supply to the perineum and perineal relaxation. After delivery of the mother to the labor room, the researcher, who was also a midwife, was unaware of the pad placement or non-pad for each subject and carried out the delivery. Decisions on whether to practice episiotomy or not were made based on the mother’ situation and the experience and opinion of the researcher. The routine Ritgen’s maneuver was carried out to control the process, during which the baby’s head was came out of the vagina in all deliveries. The control group received routine care. A total of seven individuals of the two groups were excluded from the study. Three individuals of the control group were nominated for cesarean section (C-section) due to lack of progression in the second stage of labor and four individuals of the intervention group, two of whom were eligible for the C-section due to lack of progression in the second stage of labor. The other two individuals were candidates for cupping and ventouse during labor. After the delivery, the researcher collected and recorded the data in the relevant form. The person, who performed the intervention was independent of the person, who evaluated the tear grade and the episiotomy rate. The evaluator was also blind to the grouping. Data analysis was carried out using Chi-square and independent t-tests in SPSS version 19.
3. Results
There were 54 and 53 subjects in the intervention and control groups, respectively. The two groups were homogenous in terms of demographic and clinical factors (Table 1). Considering the delivery outcomes, the results showed no significant difference between the two groups in terms of the episiotomy rate. Overall, 22 (40.7%) and 11 individuals (20.8%) underwent episiotomy in the control and intervention groups, respectively, and there was a significant difference between the two groups in this regard (P = 0.025). There was a significant difference between the two groups in terms of frequency of first and second grade tears, with the first grade tears being observed among 13 (24.1%) and 14 individuals (26.4%) of the control and intervention groups, respectively, which was not statically significant (P = 0.25). The frequency of second grade tears in the control and intervention groups was nine (16.7%) and seven (13.2%), respectively, which was not statically significant (P = 0.23) (Table 2). There was only one second grade tear case in the control group and there was no fourth grade tear in each group.
| Subjects’ Characteristics | Intervention Group | Control Group | P Value |
|---|---|---|---|
| Maternal age (y) | 6.24 ±22.65 | 3.63 ± 22.83 | 0.81b |
| Gestational age (wk) | 1.09 ± 39.22 | 1.05 ± 39.53 | 0.14b |
| Maternal weight (kg) | 9.10± 71.24 | 8.75 ± 70.94 | 0.86c |
| Mother’s place of residence | 0.92c | ||
| Urban | 27 (50) | 27 (50.9) | |
| Rural | 27 (50) | 26 (49.1) | |
| Maternal educational level | 0.75c | ||
| Illiterate | 1 (1.9) | 2 (3.8) | |
| Elementary | 8 (14.8) | 8 (15.1) | |
| Middle school | 10 (18.5) | 14 (26.4) | |
| High school | 7 (13) | 3 (5.7) | |
| Diploma | 18 (33.3) | 17 (32.1) | |
| Academic | 10 (18.5) | 9 (17) | |
| Duration of the second stage (min) | 8.46 ± 42.36 | 10.03 ± 38.52 | 0.034b |
| Birth weight of infants (g) | 384.68 ± 3283.02 | 296.58 ± 3239.81 | 0.51b |
| Newborn head circumference (cm) | 1.00 ± 35.09 | 0.92 ± 34.78 | 0.09b |
| The mean Apgar score of the first minute of birth | 0.24 ±8.79 | 0.33 ± 8.86 | 0.51b |
aValues are presented as mean ± SD or No. (%).
bIndependent-test.
cChi-square test.
| Results | Intervention Group | Control Group | Test Resultb(P Value) |
|---|---|---|---|
| The frequency of episiotomy | 11 (20.8) | 22 (40.7) | 0.025 |
| Intact perineum | 14 (26.4) | 8 (14.8) | 0.512 |
| First-grade tear | 14 (26.4) | 13 (24.1) | 0.512 |
| Second-degree tear | 7 (13.2) | 9 (16.7) | 0.236 |
aValues are presented as No. (%).
bIndependent t test.
4. Discussion
The findings of the present study showed that the use of perineal heating pad during the second stage of labor can significantly reduce the amount of episiotomy and also reduce the probability of perineal tears in primiparous females. The frequency of second grade tears in the intervention group was lower than the control group, although it was not statistically significant (Table 2). The results of the current study also revealed that the frequency of episiotomy in the control group was more than the intervention group, which was statistically significant. It can thus be concluded that the use of perineal heating pad was effective in reducing the episiotomy rate in the intervention group. Similarly, Vaziri et al. conducted a study on the effect of warm compresses on two groups consisting of 75 primiparous females in Shiraz, and the results indicated that the episiotomy rate was significantly lower in the intervention group than the control group, which is consistent with the present study (9). However, Dahlen et al. showed in a study in Australia that perineal warm compresses did not lead to a significant difference between the control and intervention groups in terms of episiotomy rate (14). One of the reasons for such difference between the results of the present study with Dahlen’s study is attributed to the fact that Dahlen used a warm compress only in the last 15 minutes of the second stage of labor in his comprehensive study, yet in the present study the heating pad was applied from the beginning and was placed on the perineum for a longer period. Also, Albers showed in his study in New Mexico that there were no significant differences between the three groups treated with perineal warm compresses, massage with the lubricant gel, and control group (no intervention) in terms of episiotomy rate (18). One of the reasons for such difference between the results of the present study and Albers’ study was attributed to the fact that Albers invited not only primiparous females in his study, but also multiparous females. Furthermore, racial differences should not be ignored in the study conducted by Albers and Dahlen. The results showed that there was no statistically significant difference between the intervention and the control group in terms of mean perineal first-grade tear. Stamp used perineal massage in the intervention group during the second stage of labor in his study in Australia and showed no significant difference between intervention and control groups in terms of the frequency of second-grade tears (19). The results of this study were consistent with the results of the present study. Albers also showed no significant differences between warm compresses, perineal massage, and control (no intervention) groups in terms of frequency of first-grade tears, which was consistent with the results of the present study (18). The present study revealed no significant difference between the intervention and control groups in terms of the frequency of second-grade perineal tears. Albers also showed in his study in New Mexico that there was no statistically significant difference between warm compresses, perineal massage, the control group (no intervention) in terms of frequency of second grade perineal tears, which is consistent with the results of the present study (18). Vaziri et al. also showed no significant difference between the two groups in terms of frequency of second-grade perineal tears (9), which is consistent with the results of the present study. Stamp et al. also stated in their study in Australia that there was no significant difference between massage and control groups in terms of frequency of second-grade perineal tears, which is consistent with the results of the present study (19). The results of comparing perineal intactness percentage showed that although there was no statistically significant difference between intervention and control groups in this regard, it was found that the use of perineal heating pad increased the likelihood of having intact perineum in the intervention group as compared to the control group. Albers showed in his study in New Mexico that there was no significant difference between the three groups in terms of intact perineum percentage (18). One of the reasons for such discrepancy between the results of Albers’ study and results of the above study is the presence of non-primiparous females in addition to primiparous females. The racial differences and duration of perineal pad placement, which was shorter in Albers’s study than the present study may have led to such difference in the results. Sohrabi et al. showed in a study in Khalkhal that the use of perineal warm compress method did not significantly influence the perineal intactness percentage, yet this method increased the percentage of having intact perineum (13), which was consistent with the results of the present study. Vaziri et al. showed in his study in Shiraz that using perineal warm compress could increase the perineal intactness percentage in the intervention group both statistically and in terms of percentage (9), therefore, the result of this study is consistent with the results of the present study. Overall, no complications have ever been mentioned in all the limited studies conducted on non-drug perineal treatment methods, especially the local heating of the perineum.
4.1. Conclusion
The results of the current study revealed that the use of perineal heating pad during the second stage of labor can be effective in decreasing the episiotomy rate and improving perineal intactness in primiparous females. Since there are a few studies in this regard, it is recommended to carry out further research in this field and other interventions affecting perineal tear and the episiotomy rate.
