1. Background
Women’s health and well-being are recognized as a human right. Additionally, its effect on the health status at family and societal levels has also become increasingly important (1-3). Women’s quality of life is currently seriously affected. Although statistics show women have higher longevity than men, women are more likely to suffer from acute complications, chronic conditions, and long-term and short-term disabilities (4). Cancers are the third leading cause of death worldwide, and 1.67 new cases of breast cancer were diagnosed in developing countries in 2012. Cancers are also the second leading cause of death, with an increasing trend in developing countries including Iran (5-8). Iranian women develop breast cancer a decade earlier compared to women in other countries, with more than 30% of patients under the age of 40 being found in about 6000 annual new cases of breast cancer diagnosed in the country (9). However, the corresponding prevalence rate is only 6% in western countries (10, 11). In fact, the incidence of breast cancer was 22 per 100,000. The prevalence in the same population was 120 per 100,000 women aged 18 - 54 (12, 13). Although the Ministry of Health has adopted policies to identify some of the most factors affecting the incidence of breast cancer, there seems to be no significant success in eliminating such disease (14). Delayed consultation is one of the main causes of death in breast cancer patients. The researchers have shown that delay in seeking medical consultation (three months or more) regarding breast cancer symptoms leads to a late-stage diagnosis of breast cancer and consequently, an increase in mortality rate (15). The continued rise in deaths from breast cancer in Iranian women is partly due to the low adherence rate to breast cancer-screening behaviors and the late-stage diagnosis of the disease (16). Cancer screening tests are not even carried out by educated and healthcare personnel, which is emphasized in the national (17-19) and global guidelines (20, 21). For example, Alam (22) showed in a study in Saudi Arabia that although 82% of women were highly aware of breast self-examination and 61% of mammography, their adherence to the above tests was 41.2% and 18.2%, respectively. The theory of change states that individuals move through six stages of change, including pre-contemplation, contemplation, preparation, action, maintenance, and termination. The individual does not want to engage in the activity in the next six months in the pre-contemplation phase. In the contemplation stage, the individual thinks about the change, but he/she is not well prepared. In a study on the frequency of screening behaviors among teachers in Iran, Moodi et al. (17) showed that 47.9% of the female teachers were in the pre-contemplation and contemplation stages of change, meaning that they showed no action and even preparation for breast self-examination. In addition, 53.9% of individuals were in stages 1 and 2 of change in terms of their adherence to the mammography test (17). Studies on the barriers to screening adherence have shown that barriers such as unawareness of the necessity and importance of testing, the feeling of shame, embarrassment, and anxiety resulting from the testing (23), painful mammography process, and fear of the possible diagnosis of malignant masses (24) play roles in individuals’ reluctance to perform the diagnostic tests. It also seems that women show ambivalence toward these tests. It is thus essential to use new interventional approaches that target the beliefs, cognitive, and behavioral problems of women in their non-adherence to screening tests. One of these methods is motivational interviewing (MI) (25), through which healthcare providers make patients express their tendency to change their behavior and promote their health status. The motivational interviewing uses a communication style, rather than a direct recommendation that triggers patient resistance, and emphasizes the deep commitment and involvement of the patient in the process of behavior change and creates a positive emotional atmosphere resulting from unconditional positive empathy and respect (26-28). Considering the high prevalence and mortality of breast cancer among women in developing countries, on the one hand, and the low adherence to screening tests, including mammography, breast self-examination, and breast clinical examination, among Iranian women as compared to those living in developed countries, on the other hand, there is a need for designing and implementing interventions based on new models of behavior change so as to increase the cancer screening behavior in women.
2. Objectives
The aim of the present study was to investigate the effect of MI-based training, compared to the conventional training, on female teachers’ level of adherence to screening behaviors in the year 2017.
3. Methods
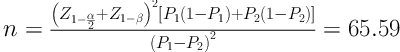
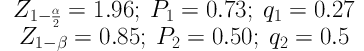
The present research was a quasi-experimental study with a pretest-posttest design. The study population included all female teachers with a minimum degree of BA working in all-girl schools at different levels of study in 2017. The inclusion criteria included the absence of breast and cervical cancers in the individual and the first-degree family members in recent years, no history of breast cancer and uterine infections in the individual and the first-degree family members in recent years, the lack of participation in the cancer screening training programs during the past year, an age between 30 and 50, being married, and non-compliance with screening programs according to the national guideline. The exclusion criterion included the lack of participation in more than one training session. The sample size was estimated using the relevant formula to be 65 per group, according to Dietrich et al.’s study (29), a 95% confidence interval, and an 80% power. In order to increase the reliability, the sample size increased to 70 individuals per group, with overall 140 individuals being selected randomly based on the inclusion and exclusion criteria. The conventional and MI-based training groups were selected from education districts 1 and 2 using a draw method, respectively. Then, the number of schools required for the conventional and MI-based training groups was determined using a simple random sampling method from among all-girl schools in the education districts 1 and 2 according to the sample size, respectively. Considering the lack of cooperation and the work shifts of some subjects, overall 134 individuals (n = 67 in each group) were examined at the end of the study.
Data gathering tools included a demographic questionnaire for age, age at pregnancy, age at marriage, number of deliveries, number of children, and adherence or non-adherence to screening tests in the last two years. Another data-gathering tool was a screening test record form, which included adherence to breast self-examination, clinical examination, and mammography throughout the study. Although the aim of the present study was not to measure the level of awareness and training feedback, the participants’ training feedback was obtained by determining their referrals for performing screening tests. After approving the project and obtaining permissions from the vice chancellor for research and technology of the university, the researcher referred to the education districts 1 and 2 of the city. One of the districts was randomly selected as the MI-based training group and the other as the conventional training group. The list of all-girl schools, in which female teachers were mainly working, was prepared for each district. Female teachers of these schools were considered as the target group according to the number of teachers with the inclusion criteria and the willingness to participate in the study. The researcher then made the required coordination for the implementation of the desired intervention (conventional or MI-based training) at each school by gradually referring to the selected schools and justifying the manager, explaining the study’s objectives, and obtaining their written consent. First, a pretest was conducted using a questionnaire to gather demographic characteristics, age at marriage, age at pregnancy, the number of pregnancies, the numbers of children, determining adherence or non-adherence to screening tests according to the relevant guideline, presence or absence of breast disease and uterine infections, presence or absence of breast and cervical cancers in the individuals and their first-degree family members in the past three years, and participation or non-participation in a screening training program over the past five months. This short questionnaire was completed in two to three minutes. All female teachers who met the inclusion criteria and participated in the study voluntarily were investigated in the form of a group; so, the number of participants varied from five to 10 at most in each group and school. The conventional training group received only three sessions of cancer screening training. The intervention group received the MI-based training as per the table of contents. Regarding the teachers’ working hours, each session lasted between 30 and 45 minutes. The waiting period was 20 weeks after completing the training in both groups and answering the probable questions. It is worth noting that the participants were reminded to send to a research colleague, who assigned such duty, a picture from the mammography test results’ sheet or physician referral form, if any, as well as a picture from a checklist showing the monthly breast self-examination via telegram. All of the teachers studied were covered by a supplementary insurance according to the education plan and did not need to pay extra for the test. As explained at the baseline, in order to ensure that the triple screening test was performed and its report was submitted at the end of the 20th week, the participants were contacted to submit the documents and the result was recorded in the relevant form. The conventional training content, which is typically provided at university-affiliated healthcare centers, was prepared based on the literature and the opinions of experts in the field of health training, obstetrics, and gynecology. The opinions of psychiatrists, clinical psychologists, psychiatric nurses, and counselors, as well as the results of previous studies (30, 31), were used according to Table 1 to finalize the MI-based training and combine the principles of MI with the conventional training. The person who was responsible for providing intervention in both groups had MA in nursing with a history of clinical work. The above individuals provided motivational counseling under the supervision of an experienced individual with Ph.D. in consultation. Data analysis was carried out using SPSS version 21. Frequency, percentage, means, standard deviation, minimum, and maximum values were determined using descriptive statistics. In order to compare quantitative variables between the two groups, independent t-test was used. The chi-square test or its equivalent was used to test the main hypothesis and compare the frequency of mammography screening tests, breast self-examinations, and clinical examinations in the two groups.
| Session | Educational Content |
|---|---|
| First | Familiarization, introduction, and expression of group rules, establishment of a report or relationship, change cycle, the practice of non-adherence to breast cancer screening tests on various aspects of women’s lives, assessment of individual’s motivation, confidence, and readiness for screening. |
| Second | Speaking about breast cancer and screening, extraction of women’s information about breast cancer, and providing more information when needed, assessing short-term and long-term advantages and disadvantages of cancer screening tests, and practicing the decisional balance. |
| Third | Detection of ambivalence about screening, calling for a discussion on change, practicing the detection of values, and creating cognitive conflicts for internal motivation, tolerance to possible resistance, self-efficacy support, and commitment to screening |
4. Results
Considering the lack of cooperation and the workplace transfer of some subjects, 67 individuals in each group, and overall 134 individuals were followed until the end of the study. The results of the independent t-test showed no statistically significant difference between the MI-based and conventional training groups in terms of demographic variables such as age, age at marriage, age at pregnancy, number of pregnancies, and number of children (P > 0.05) (Table 2). 95% of the participants in the MI-based training group and 91% in the conventional training group had an undergraduate education. The chi-square test showed no significant difference between the two groups in terms of the level of education (P = 0.24). 58.2% and 40.3% of women in the MI-based and conventional training groups, respectively, carried out breast self-examinations on a regular basis and this difference was statistically significant (P = 0.02). The frequency of referral and breast clinical examinations carried out by physicians or midwives was higher in the MI-based training group than in the control group (25.4% vs. 14.9%) although this difference was not statistically significant (P = 0.09) (Table 3). In addition, mammography tests were carried out on a regular basis by 10.4% and 4.5% of women in the MI-based and conventional training groups, respectively. Although the participants’ adherence to mammograms was higher in the MI-based training group than in the conventional training group, no statistically significant difference was obtained (P = 0.16).
| Results | Conventional Training Group | Motivational Interviewing Group | P Value |
|---|---|---|---|
| Level of education | 0.24 | ||
| BA | 61 (91) | 64 (95.5) | |
| MA | 6 (9) | 3 (4.5) | |
| Total | 67 (100) | 67 (100) | |
| Age | 44.46 ± 3.82 | 43.55 ± 4.61 | 0.2 |
| Age at marriage | 22.46 ± 4.94 | 22.14 ± 4.37 | 0.7 |
| Age at first pregnancy | 24.32 ± 5.05 | 23.62 ± 3.97 | 0.37 |
| Number of pregnancies | 1.34 ± 3.06 | 3.15 ± 1.04 | 0.23 |
| Number of children | 2.56 ± 1.11 | 2.75 ± 0.86 | 0.27 |
| Group | Motivational Interviewing Training | Conventional Training | Fisher Test Result |
|---|---|---|---|
| Adherence to breast self-examination | 39 (58.2) | 27 (40.3) | |
| Non-adherence to breast self-examination | 28 (41.8) | 40 (59.7) | P = 0.02 |
| Adherence to breast clinical examination | 17 (25.4) | 10 (14.9) | |
| Non-adherence to breast clinical examination | 50 (74.6) | 57 (85.1) | P = 0.09 |
| Adherence to mammograms | 7 (10.4) | 3 (4.5) | |
| Non-adherence to mammograms | 60 (89.6) | 64 (95.5) | P = 0.16 |
| Total | 67 (100) | 67 (100) |
a Values are expressed as No. (%).
5. Discussion
The results of the present study showed that triple tests of mammography, breast clinical examination, and breast self-examination aimed at screening breast cancer were higher in women who received MI-based training than in women receiving the conventional training and this difference was statistically significant only in the breast self-examination dimension. Using motivational interviewing principles in the health promotion-training program among women in the general population as a strategy to increase their commitment to breast cancer screening tests led to an increase in the effectiveness of such training. However, some previous studies in Iran showed that although conventional training for promoting cancer-screening behaviors including breast and cervical cancers could increase the women’s awareness and sometimes their attitude, it did not have significant effects on their referral to healthcare centers for screening tests (10, 31). The present study revealed that the adherence rate to mammography and breast clinical examination in the conventional training group was 15% and it was 50% for breast self-examination, which may be attributed to the fact that professional people are traditionally trying to encourage the patients through direct treatment recommendations and persuading the patients to change their behaviors. Although this method is helpful for some patients, it has been successful only in 5 to 10% of cases (32). This is while person-centered approaches, such as motivational interviewing, create intrinsic motivation through the explanation and resolution of the ambivalence (33). Hence, motivational interviewing has been more effective than traditional training and counseling in 75% of studies (34). Considering that some women, including educated women, such as physicians, nurses, and teachers, may have good knowledge and information about the need for a breast cancer-screening program, they still show no appropriate and satisfactory adherence towards cancer screening, which may be attributed to the subjects’ resistance. Combining motivational interviewing with conventional training methods can lead to overcoming such resistance. Similarly, Wahab et al. (35) investigated the effectiveness of telephone-based MI interventions on the individuals’ level of adherence to colon cancer-screening tests. The results showed an increase in the variety of colon cancer screening behaviors after the intervention, and participants stated that motivational counseling helped them to overcome their resistance to screening tests (35). In a study on the effect of MI-based training on increasing the adherence to changing health behaviors, Holstad et al. (36) showed that the group MI-based training increased the adherence of women with HIV to risk-reduction behaviors. In the MI-based approach, the patient is indirectly guided to change a health behavior in question. Similarly, Lasser et al. (37) showed in their study that patient navigation-based interventions increase the rate of referral for colorectal cancer screening in health centers of urban areas. Consistent with the results of the current study on the lack of a significant difference between the two groups in terms of women’s level of adherence to mammography and breast clinical examination, Menon et al. (38) showed that telephone MI-based training had no effect on colorectal cancer screening tests, including the adherence rate to fecal occult blood test, rectosigmoidoscopy, and colonoscopy, in a single one-minute session with a mean duration of 21.2 minutes and a 12-month follow-up. The reasons for the lack of a significant difference for the method used in the above study could be the motivational interviewing procedure, the low number of sessions, and the short follow-up duration. The reasons for the lack of a significant difference for the MI-based training in the present study, despite its positive effect being referred to by most studies, may be related to the manner based on which this approach was presented in the current study; thus, longer sessions are needed for the group motivational interviewing to be effective, which was reduced to less than one hour due to the teaching time limits faced by teachers participating in the present study, thereby reducing the opportunity for teamwork, discussion, and participation. The short follow-up duration, the small sample size, and fewer reports of examinations were other reasons. On the other hand, motivational interviewing has been effective even in the form of a single short session in some studies. However, since the control group also received conventional training in the present study, the observed difference, though very valuable clinically and statistically, was not significant according to statistical tests. Screening tests for highly educated teachers seemed to increase their tendency for carrying out screening tests in the short-term, and showed that there was no much difference between the above training and the MI-based training approach. VanBuskirk et al. (39) believe that if a motivational interview is carried out in a clinical setting during a single session, it will be useful and effective in increasing the readiness for changing the path to achieve the goals of health behavior change. It seems that the motivational interview elements, such as avoiding confrontation and providing direct recommendations, maintaining non-judgmental opinions, empathy and understanding, listening with contemplation, intensifying cognitive conflicts in order to increase internal motivation, resolving ambivalence in favor of behavioral change, and support for self-efficacy (40, 41) can help increase individuals’ adherence to therapies and diagnostic methods such as mammography tests, breast clinical examinations, and breast self-examinations, which are reduced due to the fear of a definite diagnosis of serious diseases as well as felling of shame and embarrassment in some cultures. Considering the foregoing, there was a significant difference between the two groups in terms of the level of adherence to breast self-examination, but it seems that the nature of screening tests, referral to physicians, and their prescription are strong barriers to clinical examination and mammography, which must be emphasized in future studies. Despite the relative and significant effectiveness of MI-based training, compared to the conventional training, in increasing the frequency of breast cancer screening in this study, the frequency of mammograms and breast clinical examinations was not equal to the corresponding frequency in similar studies and even equal to the screening rate in the general population of countries such as Turkey and less than in the general population of developed countries. Such a difference in the effectiveness may be due to the Iranian women’ insufficient screening adherence to breast cancer and the individual, social, and cultural barriers to clinical tests and mammograms. The lack of occupational diversity and the same education level of women surveyed, the failure to examine the effect of MI-based training on the screening adherence over a longer period, for example, over a one-year period or based on guidelines, the relatively small sample size, and the limited age range of the study group are among the most important limitations of the present study, which should be investigated in future studies.
5.1. Conclusions
Regarding women’s low tendency to perform breast cancer screening tests, despite having good and proper information, the results of the present study showed that adding motivational interviewing principles to the conventional training, as a complementary component, increases the effectiveness of the conventional training in some screening behaviors. Therefore, it is recommended to use motivational interviewing principles in conventional screening programs. The results also showed that although there was a clinically significant difference in some screening behaviors, the difference was not statistically significant. Therefore, it is suggested to carry out further studies on women of different age, occupational, education, and social groups to determine the effect of this treatment approach on health behavior change. Overall, it is recommended to enrich existing conventional training programs using new methods and the theory of behavioral change, such as motivational interviewing.
