1. Background
About 65% of the total population of the world experience at least one stressful event in their life (1), which can be interpreted as a sudden, unexpected, and shocking experience that is different from the usual ones (2). There are various types of events that could lead to serious damages or mortality (3), including cancer.
The traumatic nature of cancer has been significantly considered in the past decade (4). Cancer continues to increase as a traumatic and stressful event (5) affecting various aspects of an individual’s life (6). Worldwide, breast cancer is the most common type of cancer in women, accounting for 25% of all cases of cancer (7). Throughout the world, over the years of 2008 - 2013, 6.3 million women with breast cancer have been identified (8).
In addition, in 2017, in the United States, more than 255180 new cases of breast cancer have been diagnosed (9). The prevalence of this cancer in Iran is increasing. The incidence of breast cancer in the year 2000 rose from 16.7 per 100000 women to 33.6 in 2009, which would probably increase to 63 per 100000 women by 2020 (10).
Severe diseases, such as cancer, are overwhelming experiences, which exert a high psychological impact on the involved individuals (11). Cancer is a common life stressor, which can negatively affect the patient’s psychosocial state and quality of life through its symptoms and negative consequences, including anxiety and depression, fear of recurrence or spread to other organs, fear of the future, fatigue, pain, physical restrictions, and possibility of social isolation (12).
Oncology diseases are among the most destructive diseases inducing negative effects on the physical, psychological, social, and spiritual conditions of the patients (13). The negative outcomes of cancer, including PTSD, have long been recognized and evaluated. Cancer is a life-threatening situation, which is associated with constant fear of death and can have destructive effects on the physical and psychological functions of the patients (14).
One of the negative responses to the stress caused by accidents is PTSD (15). In the diagnostic and statistical manual of mental disorders, cancer is defined as a type of stress that can cause PTSD. This disorder usually occurs after an extremely stressful and emotional event, which is beyond the common life experiences and is traumatic and unbearable for the majority of the individuals (16).
The prevalence of PTSD has been reported to be 5% - 35%. There are various factors associated with cancer and PTSD. These factors include young age, low income, low education, severe previous damages, concurrent life stressors, weak social support, high social limitations, personality traits, previous emotional problems, low knowledge regarding disease stages, fear of recurrence, disease of high severity, and frequent illness (4).
Untreated PTSD leads to negative outcomes, including depression and mood disorders, as well as reduced physical health and quality of life (17). In general, PTSD is a chronic and unfavorable potential disorder determined by re-experiencing and excessive heart symptoms, as well as negative signs and avoidance of the causative agent (18).
Different studies have been conducted with the aim of reducing PTSD symptoms. In this regard, in a study carried out by Bottche et al. (19), the internet-based cognitive-behavioral therapy was reported to improve PTSD symptoms in the elderly. Moreover, Rosenbaum et al. (20), marked that exercise can be effective in the reduction of PTSD symptoms.
2. Objectives
With regard to the existing knowledge and literature on this issue, it could be stated that low number of studies have been conducted on reducing PTSD symptoms caused by breast cancer through psychological interventions. With this background in mind, this study aimed to evaluate the effect of emotional-cognitive training on PTSD symptoms among females with breast cancer.
3. Methods
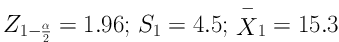
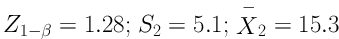
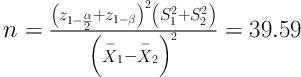
After receive code Ethics Committee of Zahedan University of Medical Sciences with the code of IR.ZAUMS.REC.1396.21 on May 7th 2017. This randomized clinical trial was conducted on females with breast cancer referring to the Chemotherapy unit of Ali Ibn Abitaleb Hospital in Zahedan, Iran, during June-August 2017 using a two-group pretest-posttest design. The study population was selected through convenience sampling technique, and then randomly allocated into two groups of control and intervention. The sample size was calculated based on the mean and standard deviation of the post-traumatic growth score in Knaevelsrud et al., with a confidence level of 95% and a statistical power of 90%, based on the following formula. In each group, 39 people were estimated. Due to potential attrition and in order to increase the validity of the study and more generalizability, in this study, 45 subjects in each group and a total of 90 subjects were determined (21).
However, two cases of the intervention group and three subjects of the control group were eliminated from the research due to the severity of their disease, hospitalization, change of their place of residence, and lack of willingness to continue participating in the study. After obtaining the official introduction letter from the deputy of health for Ali Ibn Abitaleb Hospital of Zahedan, the necessary coordination was carried out to implement the research in this location.
The inclusion criteria were: (1) Minimum age of 20 years, (2) minimum level of literacy, (3) an elapse of at least six months from the diagnosis of the disease, (4) no metastasis in patient’s medical records, (5) elapse of no more than five years from cancer diagnosis, (6) lack of any cognitive and mental disorders, (7) lack of recent life crisis with the exception of cancer, and (8) non-participation in specific educational programs.
On the other hand, the exclusion criteria included absence from educational class for more than one session and increased severity of the disease during the intervention. Written informed consents were obtained from all the participants prior to the study. Subsequently, the samples were randomly allocated into the intervention and control groups through simple random method. To this end, after preparing some envelopes containing A and B letters (A for intervention and B for control) for all evaluated subjects and randomly sorting them out, each subject received an envelope.
Data collection tools consisted of (1) demographic information form icluded age, ethnicity, marriage, education, occupation, place of residence, duration of cancer diagnosis, the stages of cancer, and history of breast cancer in the family and (2) the posttraumatic stress disorder checklist (PCL) containing 17 questions.
The posttraumatic stress disorder checklist (PCL) is a self-report scale that is used to assess the degree of disorder and screen patients from normal people and other patients as a diagnostic tool and includes three dimensions of sign and symptoms of re-experiencing traumatic injury (five questions), emotional numbness signs (seven questions), and signs and symptoms of sever arousal (five questions). Responses are based on a 5-point Likert scale (1 = at all, 5 = too much) scores that range from 17 to 85, with lower scores representing less perceived stress and higher scores reflecting more perceived stress. The validity and reliability of this list in Iran was calculated by Goodarzi (22). In addition, in the present study, reliability of the tool was confirmed by Cronbach’s alpha for the whole questionnaire of 0.88.
After getting approval from the Research Ethics Committee and permission of managers of hospital, intervention was implemented. At first, women with breast cancer who referred to the chemotherapy department were selected based on inclusion criteria and informed consent was obtained from patients in the study. Subjects were then randomly assigned to two intervention and control groups. In this way, the pockets containing study groups (A intervention and B control) were prepared and randomly arranged. Gradually, by identifying eligible individuals, one of the envelopes that identified the group was allocated to the selected individuals, respectively. At first, a pre-test was done using a questionnaire for all patients. If the patient belongs to the control group, the necessary coordination and address of the patient were taken for the post-test. It should be noted that women in the control group did not receive any other training and care during this period, except for usual care. If the patient is assigned to the intervention group, then coordination of the time and place of the training sessions was made depending on the patient’s place of residence.
The content of the training sessions, based on the Ramos et al. psychotherapy program (23), was adapted by the faculty members of Zahedan University of Medical Sciences.
The intervention group received five sessions of emotional cognitive education program in two sessions per week based on the content in Table 1. The intervention was performed in the group and the number of members in each group varied from four to eight, depending on the place of residence and favorable time for patients. The intervention was weekly in two sessions and the duration of each session varied from 60 to 90 minutes. After 12 weeks of the last training session, the chemotherapy was scheduled to be performed in the chemotherapy department, and otherwise the referral to the patient’s home was to collect information about the post-test.
| Session | Contents |
|---|---|
| One | Introduction and expression of the group rules, review of the disease, psychosocial consequences and treatment process, normalization of emotional reactions in cancers |
| Two | Education and practice of three techniques of emotional disclosure, emotional discharge, and self-regulation of emotions |
| Three | Fears and concerns related to breast cancer, facilitation and practice of cognitive processing and conscious mental rumination |
| Four | Review of achievements (positive dimensions) and losses (negative dimensions) after cancer diagnosis, development of values and new prioritization of values, redefinition of goals and creation of a new philosophy for life |
| Five | Spirituality, positive thinking, practice of patience and tolerance, conclusion |
Structure and Contents of Cognitive-Emotional Training Sessions
The educational contents were adapted from the psychotherapy program of Ramos et al. (23) that was reviewed by the faculty members of Zahedan University of Medical Sciences, Zahedan, Iran. The educational content of the training sessions are summarized in Table 1.
3.1. Statistical Analysis
The data were analyzed by SPSS21 being collected and coded. The frequency, percentage, mean, standard deviation, minimum, and maximum were determined using descriptive statistics. The Paired t-test was applied to compare means in the groups before and after the intervention. Furthermore, the comparison of the two groups was accomplished using the Independent t-test. The significance level in this study was P = 0.05.
4. Results
Based on exclusion criteria, two patients from the intervention group and three patients from the control group were excluded. Therefore, statistical analysis was performed on data from 85 patients.
The demographic characteristics of the subjects are presented in Table 2. According to the results, the two study groups were significantly different in terms of some demographic characteristics, such as occupational status and level of education (P < 0.05). Nonetheless, no difference was observed between the two groups regarding the possible effective variables on PTSD, such as age, duration of cancer diagnosis, and history of cancer in family (P > 0.05).
| Variable | Intervention | Control | P Value |
|---|---|---|---|
| Marital status | 0.9b | ||
| Single | 8 (18.6) | 11 (26.2) | |
| Married | 35 (81.4) | 31 (73.8) | |
| Total | 43 (100) | 42 (100) | |
| Occupational status | 0.01b | ||
| Employed | 8 (18. 6) | 18 (42. 9) | |
| Housewife | 35 (81.4) | 24 (57. 1) | |
| Total | 43 (100) | 42 (100) | |
| History of cancer in family | 0.31b | ||
| Yes | 3 (7) | 6 (14. 3) | |
| No | 40 (93) | 36 (85. 7) | |
| Total | 43 (100) | 42 (100) | |
| Cancer grade | 0.14b | ||
| One | 3 (7) | 9 (21, 4) | |
| Two | 20 (46.5) | 18 (42. 9) | |
| Three | 20 (46.5) | 15 (35. 7) | |
| Total | 43 (100) | 42 (100) | |
| Level of education | 0.002b | ||
| Below diploma | 25 (58. 1) | 11 (26.2) | |
| Diploma | 16 (37. 2) | 19 (45. 2) | |
| Above diploma | 2 (4. 7) | 12 (28. 6) | |
| Total | 43 (100) | 42 (100) | |
| Age | 43.90 ± 8.43 | 40.30 ± 10.82 | 0.09c |
| Duration of cancer diagnosis | 2.34 ± 1.08 | 2.50 ± 1.21 | 0.54c |
Demographic Characteristics of the Participants in the Intervention and Control Groupsa
According to Table 3, the mean score of PTSD in the intervention group decreased from 58.81 ± 15.80 before emotional-cognitive education to 32.13 ± 8.51 after the intervention. In the control group, this mean score changed from 59.59 ± 16.56 at the pre-intervention stage to 51.38 ± 13.91 at the post-intervention stage. Moreover, the mean changes in the PTSD scores were -26.67 ± 13.75 and -8.21 ± 8.09 in the intervention and control groups, respectively.
Comparison of Mean Post-Traumatic Stress Disorder in Women with Breast Cancer Before and After Cognitive-Emotional Training Program in Intervention and Control Groupsa
The Independent t-test indicated a significant difference between the study groups regarding mean PTSD score after the emotional-cognitive training (P = 0.001). In addition, there was a significant difference between the groups regarding the mean changes in the PTSD score (P = 0.001).
5. Discussion
Based on the results of the current study, group emotional-cognitive training led to the reduction of PTSD in the females with breast cancer undergoing chemotherapy. Accordingly, similar results were obtained in the studies conducted by Khosravi and Jenabian (24), Perlick et al. (18), Gawlytta et al. (25), Weinreb et al. (26), Bottche et al. (19), and Kazemi and Raminfard (27), who investigated treated breast cancer patients, veterans of the Vietnam War and their families, patients with severe sepsis, pregnant women, old patients, and patients with PTSD, respectively. Khosravi and Jenabian (24), evaluated the effectiveness of mindfulness-based cognitive therapy (MBCT) on the reduction of PTSD symptoms and improvement of memory and quality of life among the patients with breast cancer who were treated. They reported the positive impact of the mentioned method on the evaluated areas, which is in line with our findings. The two studies had similar target groups and implemented group intervention.
The difference between the two studies was that in the mentioned study, eight MBCT training sessions were held for the intervention group with a 60-day follow-up. However, in the present study, only five cognitive-emotional training sessions were administered with a longer follow-up (90 days). Moreover, the number of the subjects in the mentioned group (N = 24) was lower, compared to that in the current study.
Gawlytta et al. (25), evaluated the effectiveness of internet-based cognitive-behavioral intervention on the reduction of PTSD after severe care of sepsis among patients and their spouses. According to their results, the symptoms of PTSD changed during the intervention and led to the elimination of PTSD at the end of the intervention, which is in line with this study.
In the mentioned study, the internet-based intervention was performed by a psychologist twice a week for five weeks, followed by three-, six- and twelve-month follow ups. Moreover, the duration of training sessions in the mentioned study was twice of that of the current study, which were performed using the internet with longer follow-ups.
Given the use of the internet, the intervention was executed individually for each subject and the participants received personal response from the psychologist at the end of the process. Despite the difference in the target groups of the two studies and lack of in-person intervention in the mentioned study, the results of the both studies indicated that cognitive interventions could effectively reduce PTSD.
In this respect, a meta-analysis study was conducted on a total of 20 clinical trials by Kuester et al. (1), to determine the effectiveness of internet-based intervention on PTSD. The evaluated intervention in the mentioned research included cognitive behavioral therapy and written expression. According to the results, internet-based cognitive-behavioral therapy intervention and writing had a significant impact on the reduction of the PTSD symptoms.
In another study, Bottche et al. (19), investigated the effect of internet-based cognitive-behavioral intervention on the mitigation of PTSD symptoms among the elderly. They demonstrated that PTSD symptoms decreased in the target group after the intervention. Although the subjects of the intervention group had no cancer and received no in-person intervention, their results are consistent with our findings to some extent due to the fact that a part of the applied intervention in the current study was cognitive therapy.
Weinreb et al. (26), conducted a study on pregnant women to reduce their postpartum PTSD symptoms. According to their results, PTSD symptoms significantly decreased in the subjects of the intervention group, compared to that in the control group. Despite the investigation of pregnant women in the mentioned study, their results are relatively in line with our findings due to the application of psychological training sessions.
Moreover, Kazemi and Raminfard (27), carried out a study on the effectiveness of training anger management on increased social compatibility and improved symptoms of PTSD. In the mentioned study, anger management was trained to the subjects through seven 90-minute sessions. According to their results, the education of anger management led to the reduction of PTSD symptoms, increased social compatibility, and improved condition of patients with PTSD. With regard to the allocation of one training session to emotion regulation in the current study, the results of the mentioned study can be confirmative of the effectiveness of emotion regulation and anger management education on the reduction of PTSD symptoms.
In a study performed by Sigmund (28), investigating the effect of spirituality on the treatment of PTSD, three priests held 12 sessions in a trauma center to reduce the PTSD symptoms in patients. They reported that the presence of the clergy was beneficial in the reduction of PTSD symptoms. Spirituality is largely dependent on the culture of the individuals. However, with regard to the higher emphasis on spirituality and tolerance in the final training session of the current study, it could be concluded that spirituality had a positive effect on reduced PTSD symptoms.
In a meta-analysis study conducted on 47 studies by Gutermann et al. (29), it was reported that psychological investigations decreased PTSD symptoms in the youth. In spite of the difference between the mentioned research and the current study in terms of the target group, given the assessment of a psychological intervention and use of emotional-cognitive training in the present study, their results are incongruence with our findings.
On the other hand, the results of a study carried out by Mahmoudi Gharaei et al. (30), investigating the effect of supportive mental-social interventions on PTSD symptoms among earthquake-stricken adolescents of Bam, Iran, were inconsistent with our findings. In the mentioned research, 30 survivors of the earthquake, who received no pharmaceutical treatment due to the severity of their disorder or concurrency of other psychological disorders, participated in group intervention sessions including one psychological recite session and three cognitive-behavioral treatment sessions.
Disorder symptoms were evaluated immediately and three months after the intervention. According to their results, while the execution of short-term interventions (i.e., one psychological recite session and three cognitive-behavioral treatment sessions) led to the reduction of frequency index of PTSD symptoms, the long-term version had no significant impact (30).
The results also showed that in post-test, 12 weeks after the intervention, the mean scores of post-traumatic stress in the control group also decreased significantly. In explaining this finding, it can be stated that over time, from the onset and diagnosis of the disease as a result of the involvement of patient with the disease and its symptoms, it seems that finding the adaptive ways can reduce the post-traumatic stress by some time.
The limitations of the current study included a short 12-week interval between the pretest and posttest, small sample size, and significant difference between the study groups in terms of demographic variables (e.g., education and occupation), which must be considered in future studies. In addition, the meaning of cancer and its impact on life varies across cultures and regions. Diagnosis of cancer in different culture can lead to different psychological disorders and screening for these disorders should be considered. Therefore, generalization of results to other communities should be done with caution. This is another limitation of the current study that readers should pay close attention to it.
5.1. Conclusions
The results of the current study indicated cognitive-emotional training had positive effects on the reduction of PTSD symptoms in the intervention group. Therefore, this technique could be applied by the nurses, especially those working in the chemotherapy units, as an effective technique to reduce PTSD symptoms in the women with breast cancer, in case of the patients’ willingness. In addition, it is recommended that the effect of this method be evaluated on patients with other cancers in future studies.
