1. Background
Pain is an unpleasant emotional and sensory experience caused by tissue damage (1) and a prevalent symptom among intensive care unit (ICU) patients. Between 45 to 82% of ICU patients suffer from various degrees of pain as a stress factor (2, 3). This, in turn, leads to physiological changes and hemodynamic instability as a result of heightened levels of catecholamine and hormone secretion (4).
Pain can also instigate consequences such as changes in the depth and pace of respiration, increased cardiac workload, muscle spasm (5), suppression of the immune system, and constant catabolism (6). Considering the outcomes and complications mentioned above, pain management is one of the crucial nursing care procedures, especially for ICU patients, since they are not able to describe and express the pain they suffer from (7). Unsuccessful pain management results in prolonged hospitalization, patients’ readmission and dissatisfaction with the provided care, and eventually disease aggravation and increased mortality rates (8, 9). Assessment, management, and effective pain relief can increase patients’ physical comfort, improve the quality of life, facilitate resumption of normal everyday life, and reduce hospitalization costs (10, 11).
Numerous studies have revealed the inadequacy of pain management the in current health systems. Evidence suggests many patients experience mild to severe pain levels (12). Okuyama et al’s study on the efficiency of pain management in cancer patients showed that pain was not sufficiently managed and treated in 70% of the patients (13). Also, the results of a review study conducted by Park and Kim in 2014 proved that pain management and treatment were not thorough in ICU patients. In fact, due to their inability in expressing the pain they are in, these patients might suffer from more severe levels of pain, and if pain is controlled and treated via pharmacological and non-pharmacological methods, it might result in a reduction of pain-related stress responses in these patients (14). A very important part of nursing care is to constantly monitor and evaluate pain levels, which are neglected most of the time (15). Therefore, it is highly recommended that reliable pain assessment instruments be made accessible in ICUs (15), even though a considerable number of nurses might not use them (16). In order to assess and manage pain level, communication with patients on ventilator support who have reduced consciousness might be difficult due to the inserted the tracheostomy tube, the amount of sedatives patients take, or their connection to the ventilator (17, 18).
Successful pain management is the result of accurate systematic analysis to make the right decision with regard to painkiller prescription, if necessary (19). In this respect, the use of strategies such as pain management algorithms or protocols is crucial. One such algorithm was developed in 1990, which is now considered an inclusive approach to the use of pain assessment tools, and it plays an effective role in assisting ICU nurses and doctors to manage patients’ pain level based on the evaluation findings (20). This algorithm consists of a list of behavioral and physiological indexes enabling nurses to make an accurate assessment of the patient’s pain level and then to decide whether or not to use painkillers accordingly. In a number of studies, this algorithm was used in patients who were unable to express their pain (9, 20), and its application in ICU patients who are mostly incapable of verbal communication is complicated (21).
Nurses’ low level of success in managing patients’ pain has been widely reported. A research conducted by Ross et al. verified that ICU nurses are not highly willing to use pain assessment tools in patients with loss of consciousness and they have inadequate information about pain management protocols, which in turn, can have a negative impact on their performance in controlling patients’ pain (1). Sessler et al. showed that 35 to 55% of nurses estimate the pain level lower than what it actually is, and 64% of patients receive no medications before or during painful procedures (22). Rahimiyan et al. focusing on patients’ pain control after abdominal surgery, demonstrated that nurses’ pain management was not desirable (23). van Gulik et al. indicated that nurses’ observation of unplanned pain control interventions was poor, while their attention to planned protocols was suitable (24). On the contrary, based on the results reported by Francis and Fitzpatrick, the majority of nurses have an acceptable awareness and performance in assessing pain in semi-conscious patients. However, most previous studies on this area suggest a lack of successful pain management, especially in the case of patients with loss of consciousness , there have been discrepant results as well (25). Therefore, it is vital to emphasize on the use of pain management algorithms and to incorporate them in medical practice for patients who are unable to report their status. This is possible through deploying valid pain assessment tools based on a well-defined and consistent method.
A limited number of studies have addressed the assessment, recording, and reevaluation of pain in ICUs (26). Previous studies have mostly highlighted the impact of pharmacological and non-pharmacological interventions on pain intensity, while the evaluation of pain management protocols is generally neglected, especially in the case of ICU patients. According to the investigations conducted in ICUs in Iran, decisions concerning pain management are mostly made based on changes in the patient’s vital signs and personal opinions, and most often painkiller prescription is dependent on the doctor’s orders and not the patients’ real needs; furthermore, no following reevaluation is performed based on specified protocols. In addition, pain assessment information is not systematically recorded, and due to the fear of possible complications and drug-dependence, medications are infused at a lower dosage than the prescribed amount. All of these factors run the risk of unsuccessful pain management, pain control, and pain relief, which in turn, are the underlying causes of negative and disturbing physical and psychological effects of pain. Improper monitoring and uncontrolled infusion of painkillers could lead to other complications as well.
Therefore, it is necessary to study the efficiency of pain management programs, considering the insufficient pain management, especially in patients with loss of consciousness, the negative impacts of nurses’ negligence of standard pain management and pain control methods (1, 5, 6), the contradictory results reported in the literature, and the fact that Iranian ICU nurses do not practice any inclusive approach to manage and control patients’ level of pain.
2. Objectives
The present research aims at evaluating the impact of a pain management algorithm on the level of pain intensity in patients with loss of consciousness admitted to an ICU.
3. Methods
The present study was a randomized single-blind clinical trial performed among intubated patients with loss of consciousness. The patients were on ventilator support and hospitalized in the ICU of Khatam al-Anbiya Hospital in Zahedan. Sample size was determined in accordance with the study of Shahriari et al. (27) and based on the Equation 1.
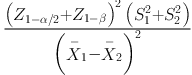
Sample size was estimated at 42 for each group. To increase the confidence interval and considering possible sample attrition, the number of patients in each group was set at 45; thus, a total of 90 patients were studied. After obtaining a written consent form from the patients’ legal guardians, the participants were chosen through convenience sampling. Using permuted block randomization, the subjects were assigned into two groups of pain management algorithm and control. Since both groups were necessary for carrying out this research, the patients were enrolled according to six schemes of four-member blocks, in which As and Bs were respectively assigned to the pain management algorithm and control groups (for example, AABB, ABAB, BBAA, etc.); each block consisted of two participants from each group. The order of the blocks was determined randomly by means of a random number generator, and patients were entered into the intervention or control groups according to the blocks. Single-blindness of this research was due to the fact that the pain assessor was not aware of the group allocations.
The most important inclusion criteria were: 18 to 65 years of age, no history of plegia, no history of chronic pain such as migraine or backache, no history of neuromuscular or sensorimotor disorders, no history of paralytic medications consumption, level of consciousness between 5 to 8 according to Glasgow Coma Scale, and initiation of painkiller infusion. On the other hand, the most notable exclusion criteria were regaining full consciousness and tracheal extubation at any point throughout the study, transfer to surgery room for surgical operations, consumption of muscle relaxant medications at any point during the research, patient’s transfer to any other ward or any other hospital, patient’s demise, and impossibility of changing painkiller dosage for any particular reason according to doctors’ prescriptions (as one of the phases of algorithm implementation).
The instruments used in this study included a demographic checklist (consisting of personal information and particularities of the disease) and the Behavioral Pain Scale (BPS). BPS is used as a pain assessment tool in patients who are on mechanical respiratory support and are unable to describe their pain level. This instrument was designed by Payen et al. (28) and consists of three parts, including facial expression, upper limb movement, and compliance with mechanical ventilation, each one being scored between 1 to 4. Higher scores indicate a higher level of pain and agitation. The total score ranges between a minimum of 3 (minimum pain level) and a maximum of 12 (maximum pain level). The reliability of this instrument has been confirmed by studies conducted in Iran and abroad (28-32). In addition, its internal consistency was reported 0.94 according to Cronbach’s alpha coefficient. Also, in the present study, the reliability of this tool was established using Cronbach’s alpha coefficient (0.91) and intraclass correlation coefficient (0.89) (28).
In order to conduct this research, after obtaining approval of the university’s Ethics Committee (registered with the code IR.Zaums.REC.1396.357) and permission of the hospital authorities, the research team began data collection. After explaining the purpose of the research and the intervention procedure to families of the qualified patients, the authors asked them to submit a written consent on behalf of their patient to participate in the study.
The algorithm used here is an inclusive approach to the use of pain assessment and pain evaluation tools. It plays a significant role in helping ICU nurses and doctors in managing patient’s pain based on the findings of the evaluation. This algorithm involves repeated assessments of pain and adjustment of the prescribed painkiller dosage in accordance with the latest assessment of pain intensity (5). In the intervention group, pain management algorithm was implemented in three work shifts throughout an entire day. The researcher was responsible for implementing the algorithm and explaining it to the nurses of the ward as well. The researcher applied the algorithm in three working shifts: In the morning between 8 to 10 a.m., in the evening between 3 to 5 p.m. and at night between 10 p.m. and midnight. This algorithm incorporates two types of pain assessment instruments for both patients who are capable of communication and those with loss of consciousness who are on ventilation support and incapable of verbal communication. Since the present study addresses patients with loss of consciousness, BPS was chosen for this purpose according to the algorithm.
Based on pain management algorithm and by using BPS, the researcher measured and recorded the patients’ pain level twice during every working shift, once before implementing the algorithm and another time after that. In the event that the initial BPS score was between 3 and 5, pain relief measures including the infusion of painkillers would be reduced after consulting the physician in charge. In other words, the patient’s intake of sedatives would be lowered as required. Based on the algorithm, 15 minutes after intravenous sedative infusion, pain was reassessed and the resulting score was recorded in certain sheets.
In case the initial level of pain intensity measured by BPS exceeded 5, pain relief measures would increase after informing the anesthesiologist and consulting with him/her. As in the previous situation, 15 minutes after the intravenous infusion, pain intensity was reevaluated and the result was recorded in the forms. It should be noted that in all cases an anesthesiologist was consulted prior to increasing or decreasing the patient’s medication dosage. Pain relief measures varied according to the doctor’s orders, and they included painkillers such as midazolam, fentanyl, and morphine. The medications were infused separately or in pairs. Participants of the control group only received the routine care and pain control measures provided by the ward. Pain assessment was carried out in the three shifts, similar to the intervention group.
After data collection, SPSS 15 was employed for analyzing them. Descriptive statistical tests (including frequency distribution table, mean, and standard deviation) were used to describe the data. Firstly, using Shapiro Wilk normality test, the normality of data was evaluated. Since it was proven normal, the mean values of quantitative variables in the intervention and the control groups were compared using the independent t-test. Besides, in order to examine the mean values of quantitative variables before and after the intervention separately in the two groups, paired t-test was used. Chi-square test was employed to analyze qualitative variables in the two groups. Finally, P value less than 0.05 was considered significant.
4. Results
The mean age of the participants was 42.07 ± 14.46 years, and 61 (67.8%) of the patients were male and the rest were female. With regards to marital status, the majority of patients were married (61.1%). Regarding the infusion of midazolam, fentanyl, and morphine sulfate, the results show that midazolam and fentanyl were infused in most patients (82.2% and 83.3%, respectively), while morphine sulfate was infused in just 16.7% of the patients. Additionally, the results showed that there was no significant difference between the intervention and control groups in terms of age, gender, marital status, and infusion frequency of the three sedative medications (Table 1).
| Variable/Group | Intervention | Control | P Values |
|---|---|---|---|
| Gender | 0.259 | ||
| Male | 12 (26.7) | 17 (37.8) | |
| Female | 33 (73.3) | 28 (62.2) | |
| Marital status | 0.085 | ||
| Single | 10 (22.2) | 8 (17.8) | |
| Married | 31 (68.9) | 24 (53.3) | |
| Widow(er) | 3 (6.7) | 6 (13.3) | |
| Divorced | 1 (2.2) | 7 (15.6) | |
| Midazolam infusion | 0.098 | ||
| Yes | 34 (75.6) | 40 (88.9) | |
| No | 11 (24.4) | 5 (11.1) | |
| Fentanyl infusion | 0.57 | ||
| Yes | 40 (88.9) | 35 (77.8) | |
| No | 5 (11.1) | 10 (22.2) | |
| Morphine sulfate infusion | 0.396 | ||
| Yes | 9 (20) | 6 (13.3) | |
| No | 36 (80) | 39 (86.7) | |
| Age, mean ± SD | 39.78 ± 15.47 | 44.36 ± 13.16 | 0.134 |
The mean values of pain intensity in the two groups were the same before the intervention and throughout the three work shifts. In other words, there was no significant difference in the mean value of pain in the two groups in the morning shift prior to implementing the intervention (P = 0.605), while after the intervention the difference of the same variable between the two groups became significant (P < 0.001). Also, the mean changes of pain intensity in the intervention group was more than that in the control group, and the difference was statistically significant (P < 0.001; Table 2).
| Shift Time/Group | Before Intervention | After Intervention | Changes | P Valuea |
|---|---|---|---|---|
| Morning | ||||
| Intervention | 5.89 ± 1.22 | 4.16 ± 0.37 | 1.73 | 0.001 |
| Control | 5.76 ± 1.21 | 5.87 ± 1.34 | -0.11 | 0.559 |
| P valueb | 0.605 | 0.001 | 0.001 | |
| Evening | ||||
| Intervention | 6.80 ± 1.31 | 4.53 ± 0.63 | 2.27 | 0.001 |
| Control | 6.56 ± 1.41 | 6.42 ± 1.77 | 0.14 | 0.542 |
| P valueb | 0.396 | 0.001 | 0.001 | |
| Night | ||||
| Intervention | 7.53 ± 1.10 | 5.41 ± 0.66 | 3.02 | 0.001 |
| Control | 7.11 ± 1.33 | 6.73 ± 1.79 | 0.38 | 0.098 |
| P valueb | 0.105 | 0.001 | 0.001 |
aPaired t-test.
bIndependent t-test.
5. Discussion
The findings of the present study illustrate that implementing the pain management algorithm in patients with loss of consciousness can reduce their pain intensity. Thus, the mean changes of pain in the intervention group exceeded those in the control group during the three work shifts of algorithm implementation, and the difference between the two groups in terms of the same variable was significant. The reduction of pain intensity after receiving the intervention in the pain management algorithm group substantiates the efficacy of this algorithm. Additionally, frequent pain assessments and pain level evaluations through this approach show the efficiency of pain relief measures and consistent pain monitoring in patients who are unable to express it.
According to Shahriari et al. the mean pain level was significantly lower in participants who received the pain management program than those in the control group, indicating the effectiveness of the implemented program (27). These results are consistent with the findings of the present study, which suggest that pain levels of patients can be successfully controlled through a pain management program. Even though the protocol used by Shahriari et al. was different from the algorithm used in the present research and their study population consisted of patients with loss of consciousness after general surgeries, which is different from that of the present research, pain intensity was assessed repeatedly in both works, and deciding whether or not to change the patient’s medication dosage was based on specific programs used in the studies, both of which proved to be highly effective.
Chanques et al. proposed that the mean value of pain was significantly lower in the group that received regular pain assessment (twice a day) than that in a control group (6). The results obtained from the research by Egerod et al. are totally consistent with the present findings. In that research, implementing a sedative and soothing protocol in patients on ventilator support resulted in a reduction of pain intensity and a better control of pain level (33). Egerod et al.’s study differs from the present research in terms of the category of implemented protocol, yet, despite this difference, in both studies implementation of the protocol led to a better management of pain in the intervention group. To explain this finding, it could be mentioned that applying pain management programs in the form of protocols or algorithms leads to more effective pain control and pain relief, since they provide consistent pain assessment and repeated pain level evaluations in an integrated manner. Consequently, healthcare personnel are able to give timely responses to patient’s pain by changing the therapeutic relief measures. One of the advantages of applying pain management algorithms in ICUs is the use of the same instrument for both assessing and controlling pain, which encourages a sense of commitment among the nursing staff to make use of it in order to assess pain level in patients. This also leads to an enhanced physician-nurse relationship in terms of changing the prescribed dosage of sedative medications (34, 35).
In a research aimed at utilizing a multi-functional pain management protocol in patients undergoing total joint replacement surgery, the protocol was successful in reducing patients’ pain intensity (36). Even though the research by McDonald et al. was conducted on a different study population and a different pain assessment tool was employed, its findings were in line with the present results. In a study by Wong et al. implementing a pain management protocol in triage, especially for patients with skeletal problems, caused a significant reduction in pain intensity compared with a control group (37). The main difference between that study and the present one is in the population under investigation, that is, Wong et al.’s study targeted fully conscious patients and pain intensity was measured by using a visual pain assessment tool. Despite this difference, the results obtained by the two studies were consistent. This point highlights the importance and efficiency of repeated pain assessments, careful recording, reporting pain intensity values, and adjustment of sedative dosage in accordance with the patient’s needs regardless of the level of consciousness. It can be concluded that even in the case of patients who are unable to express their level of pain, it is possible to better control pain by means of objective evaluation tools.
Pharmacological treatments cannot be adjusted according to the patient’s needs in case pain management and pain assessment techniques fail to make a consistent and accurate report of the level of pain, which disrupts the course of treatment. In this regard, the suggestion made by Wells et al. for considering pain as the fifth vital sign is notable, since using instruments of pain assessment and recording its level can significantly improve nurses’ performance in handling and evaluating patients’ pain intensity (26)
Chanques et al. (6) and Rafiei et al. (38) proposed that consistent assessment of patient’s pain and restlessness not only leads to a more coordinated relationship between physicians and nurses, but also it entails a more effective medication adjustment in terms of the infused sedatives, and consequently, a significant reduction of pain intensity in ICU patients. These two studies were similar to the present one with respect to study populations and the tools used. Gelinas et al. exploring pain reassessment in traumatized patients who were on ventilator support, came to analogous results and observed that implementing the pain management program enhanced patient’s pain management from 40% to 93% (35). These findings reaffirm that to develop an effective management program, it is crucial to repeat the assessment after taking the therapeutic measures. In line with the findings of the present research, Keykha et al. investigating patients on ventilator support, found that executing pain control and soothing protocols can play a decisive role in improving pain control in ICU patients (39).
Regarding the limitations of the present study, it could be mentioned that the sample size of patients under investigation was rather small and that the research only covered patients of one hospital. Thus, generalization of our findings to other situations and patients should be performed with cautious.
5.1. Conclusions
According to the findings, implementation of a pain management algorithm involving repeated pain assessment can be considered an integrated and systematic method to provide better pain control in patients with loss of consciousness who are not able to express the pain they suffer from. Since this algorithm was found effective in reducing patients’ level of pain, it is strongly recommended that ICU nurses use it at all times, since adopting protocols and algorithms helps nurses make a more efficient use of pain assessment tools and obliges them to be more responsive and accountable towards patients in pain. As a result, a better pain control will be observed among patients whose level of pain is commonly ignored.
